Introduction
Magnetic resonance imaging (MRI) is an essential modality in evaluating the ligamentous and soft tissue elements of the upper cervical spine. This region has horizontally oriented facets and no intervertebral discs; ligaments and membranes are thus crucial in stabilization at these levels. This makes MRI an invaluable tool in assessing high cervical injury. MRI also demonstrates prevertebral and posterior neck soft tissue edema in such injuries. It is now considered the gold standard imaging study for the evaluation of patients with neurologic findings or when CT imaging findings are consistent with upper cervical spine trauma/injury. In one study, MRI demonstrated injury in 21% of the patients with normal radiographs or CT scans. While several grading systems have been developed to classify and guide the management of these injuries, evaluation is based predominantly on the analysis of individual anatomic components. Additionally, MRI can be utilized for the evaluation of congenital and degenerative conditions of the upper cervical spine. As in other areas of the spine, MRI also has utility in assessing the spinal cord and canal. In this chapter, we seek to describe utility and common applications of MRI of the upper cervical spine.
Normative Cervical Spinal Cord Dimension
A fundamental understanding of normative values for cervical spine measurements is important when evaluating for pathology. Plain radiographs and CT scans have been utilized to obtain the measurements of spinal canal and spinal cord dimensions for decades. These imaging methods are inherently limited by effects of magnification and poor soft tissue resolution. MRI, specifically T2-weighted images, provides the detail necessary to accurately measure various components of the axial spine. As with most anatomical measurements in the body, there are significant variations based on age and sex.
Spinal Canal/Cord Diameter
The evaluation of the spinal canal diameter in the axial spine is best performed using midsagittal T2-weighted image, with a reference line drawn intersecting the most concave portions of both the anterior and posterior elements of C1. Measurements along this line can be used to define the spinal canal diameter of the axial spine that is the distance from the tectorial membrane to the anterior-most aspect of the posterior arch of C1. Similarly, the measurements of spinal cord diameter can be made along this same line ( Fig. 1 ).
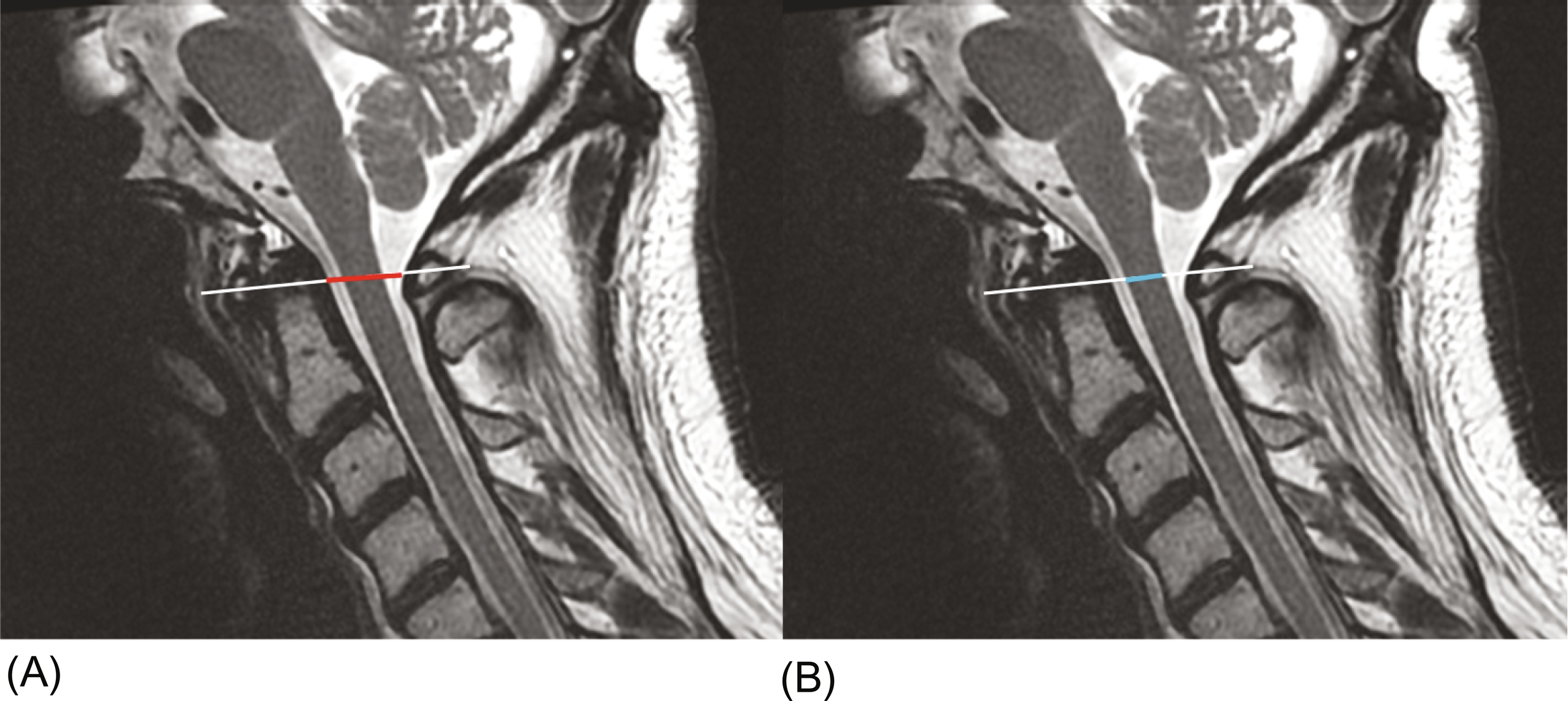
One prospective multicenter trial found both spinal canal and cord diameter in the axial spine are dependent on age, gender, and body height in normal volunteers with no known cervical pathology. Therefore, there is no universal normal value that can be applied across all patients.
Vertebral Artery on MRI
The course of vascular structures is important in operative planning. In the axial spine, the vertebral artery is the largest and most significant vascular structure to be aware of, particularly with posterior surgical approaches to this region. In the typical course, the symmetric vertebral arteries course within the transverse foramen, exiting at C1 and coursing medially in a bony groove called the sulcus arteriosus before entering the foramen magnum. On MRI, vascular structures are best evaluated on MRA, though these may not routinely be included in studies of the cervical spine. Therefore, the course of the vertebral artery can be adequately assessed as a flow void on T2-weighted images ( Fig. 2 ).

Both sagittal and axial views can be used to assess the course, with thin cut images allowing for a more comprehensive view of any vessel loops. Important considerations when evaluating the vertebral artery are tortuosity that may put the vessel at greater risk during surgical dissection. In addition, it is important to know of any anatomical variants such as dominance of one side or atypical courses of the vessel that may alter surgical planning or decision-making intra-operatively.
Trauma
Fractures of the upper cervical spine account for an estimated half of all cervical fractures. Injury in this region can be clinically fraught, as many of these patients have an associated cranial injury that can limit physical examination or may have only mild symptoms of neck pain and stiffness. Instability of the upper cervical spine can have devastating neurologic consequences, making its prompt identification crucial to proper management. Several classification schemes have been devised to attempt to guide clinical decision making in these patients.
In combination with radiographic and CT imaging, a holistic picture of a patient’s injuries can be created. The indications to obtain a cervical spine MRI in the setting of trauma are diverse, including: to assess for ligamentous injury, to evaluate the spinal cord in patients with neurologic deficit (and prognosticate by differentiating hemorrhagic from nonhemorrhagic cord injury), to identify epidural hematoma, to rule out an occult bony injury with negative CT or radiographs, and to assess spinal stability to determine whether immobilization in a cervical collar is necessary. The routine use of cervical spine MRI in trauma patients, however, is highly contested, particularly in the setting of an obtunded or comatose patient. Some authors argue that MRI is the gold standard for assessing cervical spine stability in patients unable to participate in neurologic exam, while others believe this study to be an unnecessary and costly endeavor that does not ultimately affect patient outcome.
Transverse Ligament Injury
The transverse ligament (TL) is crucial to atlantoaxial stability; its disruption is considered the most important pathologic contributor to instability at this level. When there is transverse ligament disruption associated with a dens fracture, there is a high rate of nonunion, as dens displacement or angulation is associated with injury to the transverse ligament.
The transverse ligament can best be appreciated using axial sections of a gradient echo sequence, where it is visualized as a band of homogenous low-intensity signal between the synovial capsule and the cerebrospinal fluid. Tears are seen as gross disruption of the ligament on MRI ( Fig. 3 ).
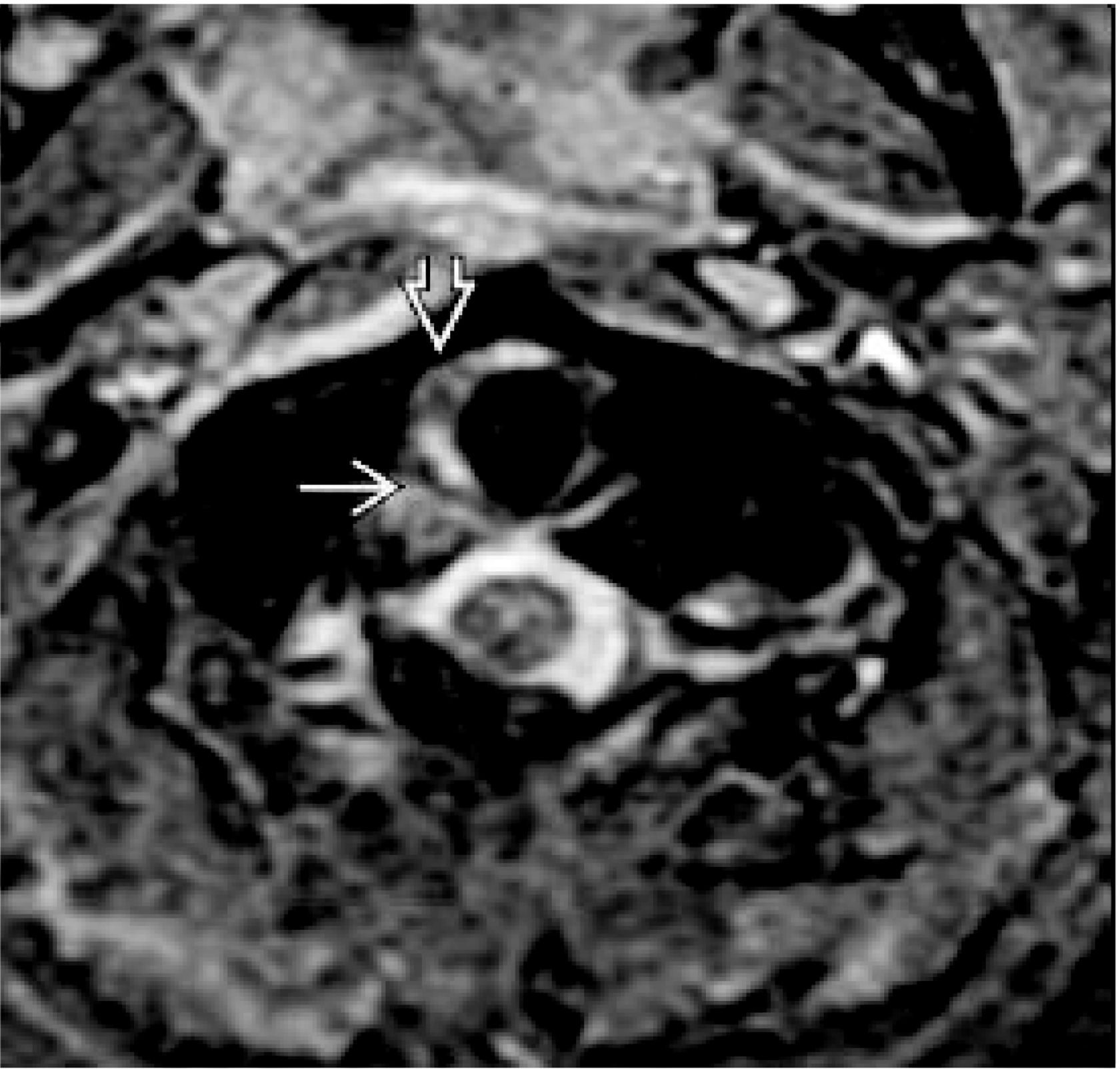
More commonly, T2 axial sections are obtained and demonstrate a uniform hypointense structure of an intact TL dorsal to the dens. When injured, there is an increase in T2 signal intensity indicative of edema, tearing, or avulsion ( Fig. 4 ).

Alar Ligament Injury
It has been found that 30%–50% of the patients with craniocervical instability have avulsion of the alar ligament (AL), which can best be evaluated in the coronal plane on MRI. This bilateral structure connects the dens to the occipital condyle ( Fig. 5 ).

In one study, the AL was identified using MRI on either side in approximately 80% of healthy patients. Interestingly, it was found that of these healthy patients, 36%–48% had effusion at C1-C2, which in the absence of alar ligament visualization may represent rotational injury. In another study of diverse groups, including healthy volunteers, patients with cervical spine trauma, and cadaveric samples, nearly all alar ligaments could be identified; resection of the ligament on cadaveric samples could also be appreciated as a void on MRI.
Tectorial Membrane Injury
The tectorial membrane (TM) is an extension of the posterior longitudinal ligament, connecting the dorsal aspect of the dens and the vertebral bodies of C2 and C3 to the clivus. Along with the alar ligament, it prevents anterior subluxation of the head on the cervical spine and limits flexion. It appears as a thin, hypointense structure in T2 sequences ( Fig. 6 ).