Shoulder
- Hamid Torshizy
- Tudor H. Hughes
- Christine B. Chung
- Tudor H. Hughes
The shoulder girdle is a general term describing a complex network of soft tissue and osseous structures, demarcated by numerous joints, which serve to both suspend and connect the upper extremity to the torso. Injuries of the shoulder girdle are common, with sites of injury varying with the age of the patient. In general, whereas fractures of the clavicle are the most common cause of skeletal injury in younger populations, glenohumeral and acromioclavicular joint dislocations predominate between 20 and 40 years of age, and proximal humeral fractures prevail in older adults. This section will emphasize common mechanisms of injury, common patterns of injury, classification of injury types, variations of injury, and common pitfalls to diagnosis.
Anatomy
The osseous structures constituting the shoulder girdle are the clavicle, the scapula, and the proximal humerus ( Fig. 14-1 ). The scapula is further divided into the acromion, coracoid, scapular body, neck proper, and glenoid. Interposed between these structures are three joints, the acromioclavicular, sternoclavicular, and glenohumeral.

The clavicle is an S-shaped bone that is more tubular medially, gradually becoming flatter at its lateral extent. It connects the manubrium to the scapula, forming a diarthrodial joint proximally (sternoclavicular) and distally (acromioclavicular). Several ligaments act as key stabilizers of the clavicle. The coracoclavicular ligament, consisting of the conoid (medial) and trapezoid (lateral) portions, acts to bind the clavicle to the scapula. The acromioclavicular ligament links the clavicle to the acromion. Several muscles insert on the clavicle, including the pectoralis major, deltoid, sternocleidomastoid, and trapezius.
The scapula is a flat, triangular bone that is often divided into two parts, the body and the neck. The body is composed of several osseous prominences. These include the spine dorsally which terminates in the acromion process, the superior lateral angle which forms the glenoid fossa, and the superior and inferior angle. The coracoid process arises just medial to the glenoid fossa along its superior edge. The neck refers to the flared portion of the scapula that forms the glenoid fossa.
The proximal humerus is anatomically divided into the head, anatomic neck, surgical neck, and the lesser and greater tuberosities. The anatomic neck refers to the constricted portion of the humeral head circumference. The surgical neck is the constricted osseous portion arising below the tuberosities. The greater tuberosity is an osseous prominence arising from the head laterally, serving as insertion primarily for the supraspinatus, infraspinatus, and teres minor tendons. The lesser tuberosity is an osseous prominence arising from the anterior humerus below the anatomic neck, serving as attachment for the subscapularis tendon. The tuberosities are separated by an osseous concavity, the bicipital groove, which houses the long head of the biceps tendon.
Osseous Emergencies
Clavicle Fractures
Fractures of the clavicle are one of the most common injuries of the shoulder girdle, with the majority occurring during childhood and 50% occurring in children under 10 years of age. Fractures occur as a result of falls with direct trauma or from falls on an outstretched arm. In childhood, fractures are often either a greenstick or bowing variety. In adults, fractures have been traditionally categorized using the Allman classification, with injuries divided anatomically into those affecting the proximal third, middle third, and distal third of the clavicle ( Fig. 14-2 ).

Injuries involving the middle third are most common, accounting for nearly 80% of fractures. Patterns can be transverse and complete or comminuted. Frequently the distal fragment is depressed due to the weight of the upper extremity and the proximal fragment is elevated due to the pull of the sternocleidomastoid muscle. A more exaggerated pattern involves overriding of edges, where the distal fragment underlies the proximal.
Fractures of the outer third account for 15% of injuries and can be associated with fractures through the base of the coracoid process. Unlike fractures involving the middle or inner one third, fractures of the outer third can be associated with disruption of the coracoclavicular ligaments, which include the conoid and trapezoid ligaments. Commonly this can lead to superior displacement of the medial fragments and an increase in the distance between the coracoid and clavicle, caused by the unopposed pull of the sternocleidomastoid muscle attachment to the clavicle. However, this may not be readily apparent on standard views. Therefore, whenever a fracture of the outer third is encountered, it is recommended that stress views be obtained to accentuate possible ligamentous injury.
Lastly, fractures of the medial or inner third account for 5% of injuries. These fractures are difficult to identify owing to overlapping ribs and spine. Fractures are best identified on steeply angled lordotic anteroposterior (AP) projection and/or on computed tomography (CT).
Pitfalls of diagnosis include lack of adequate technique for evaluation of undisplaced fractures of the middle third, which requires 15 degrees cephalic angulation of the beam. In addition, episternal ossicles, accessory ossification centers located posterior or cephalad to the manubrium, may be mistaken for fracture ( Fig. 14-3 ). Fractures of the clavicle are infrequently associated with injury to the underlying subclavian artery and brachial plexus in the setting of severe trauma.

An important cause of pain in the area of the acromioclavicular joint is distal clavicular osteolysis. Most instances are caused by overuse, particularly from weight lifting, although it may also occur as a consequence of traumatic joint separation. The radiographic manifestation is focal osteopenia in the distal 2 cm of the clavicle, as well as loss of the articular cortical margin ( Fig. 14-4 ).

Scapular Fractures
The scapula is protected by overlying soft tissues, thus injuries of the scapula occur infrequently, accounting for 3% to 5% of all shoulder girdle injuries. The mean age of patients who present with injuries ranges from 35 to 45 years. Common mechanisms include axial loading on an outstretched arm (scapular neck, glenoid), direct high-energy trauma (body), direct trauma (acromion, coracoid), glenohumeral joint dislocation (glenoid, coracoid), or traction by ligaments (avulsion fractures). Overall, the majority of injuries are caused by severe high-impact trauma, with vehicular accidents accounting for 75% of them. Fractures are generally described according to anatomic area: acromion, coracoid, body, and neck/glenoid, with glenoid fractures further dividing into extra-articular and intra-articular. Fractures of the scapular neck (10% to 60%) and the body (49% to 89%) are most common.
Fractures involving the acromion process are most often transverse in orientation and affect the acromial base. Kuhn and coworkers classified acromial fractures into three types, with surgery reserved for type III injuries. Type I are nondisplaced and subdivided into an avulsive type IA or direct trauma type IB ( Fig. 14-5 ); type II fractures are displaced laterally, anteriorly, or superiorly and do not reduce the subacromial space; and type III fractures reduce the subacromial space by an inferiorly displaced acromial fracture or an acromial fracture associated with an ipsilateral superiorly displaced glenoid neck fracture. The os acromiale, a secondary ossification center identified at the level of the acromioclavicular joint, may persist into adult life and be mistaken for a fracture ( Fig. 14-6 ). It is present in 2.7% of randomly selected adults and when present, occurs bilaterally in 60% of cases. Distinction from fracture is made by its typical location, recognizing its well-corticated borders and/or symmetry.


Coracoid fractures are characterized into two types based upon the fracture location with respect to the coracoclavicular ligaments. Type I fractures occur proximal to the coracoclavicular ligament attachment ( Fig. 14-7 ) and may require surgical correction because they are often associated with acromioclavicular separation, clavicular fracture, superior scapular fracture, and/or glenoid fracture. Type II fractures occur distal to the coracoclavicular ligament attachment and are treated conservatively ( Fig. 14-8 ). These fractures are very difficult to identify on standard AP views and are best demonstrated by 25- to 45-degree cephalic angulation of the beam in the frontal projection. Stress fractures of the base of the coracoid, a less common pattern of injury, have been described in trapshooters. A small secondary ossification center located on the surface of the coracoid, often presenting as a fine shelf of bone, should not be confused with fracture.


Glenoid fractures either involve or spare the articular surface. Extra-articular glenoid fractures are classified according to the presence or absence of concomitant acromioclavicular separation or clavicular fracture. Unlike their extra-articular counterparts, intra-articular fractures of the glenoid are more complex. Ideberg and coworkers classified fractures into five types, with a sixth type added by Goss and colleagues. Type I involves the glenoid rim with type IA affecting the anterior and type IB the posterior surfaces; type II are transverse or oblique fractures through the glenoid fossa with inferior fragment displaced; type III are oblique fractures of the glenoid exiting at the mid to superior scapular border, often associated with acromioclavicular fracture and/or dislocation; type IV are horizontal fractures exiting through the medial scapular border; type V are a type IV fracture pattern with separation of the inferior half of the glenoid; and type VI is a comminuted fracture.
Fractures of the scapular body are generally categorized as being vertical or horizontal. Numerous classifications exist in the literature. The classification system introduced by Zdravkovic and Damholt is a system most used by orthopedic surgeons in the clinical setting. This classification divides injuries into three types: type I are fractures of the body ( Fig. 14-9 ); type II are fractures of the apophyses, including the acromion and coracoid; and type III are fractures of the superolateral angle, including the glenoid neck. Nutrient canals or foramina can mimic fractures, most commonly in the body and spine ( Fig. 14-10 ). They are usually oriented horizontally, paralleling the superior border of the scapula, and demonstrate a well-corticated margin. In addition, a persistent ossification center at the inferior angle of the scapula can also simulate a pathologic process. Scapular fractures are commonly associated with important findings, including pulmonary injury, brachial plexus injury, clavicle fractures, rib fractures, and other fractures of the axial and appendicular skeleton.


Atypical Injuries of the Shoulder Girdle
Avulsion injuries of the shoulder girdle represent a less common pattern of injury, with failure occurring at insertion of ligaments. The most common sites of injury include the inferolateral margin of the glenoid at the insertion of the long head of the triceps tendon ( Fig. 14-11 ) and the lateral scapular margin at the insertion of the teres minor muscle. Lastly, insufficiency fractures of the scapula represent a rare pattern of injury seen most commonly with mineralization disorders such as encountered in osteomalacia.

Fractures of the Proximal Humerus
Fractures of the proximal humerus are biphasic in occurrence, most commonly occurring in people in their second decade of life and in people over 50 years of age. Patients presenting from 20 to 50 years of age are less common, and their injuries are the result of high-impact trauma. Fractures in patients younger than 20 years often result in separation of the proximal humeral epiphysis, whereas fractures in patients over the age of 50 years are often associated with osteoporosis.
Fractures of the proximal humerus can be classified using an anatomic basis. In general, isolated fractures of a single region are uncommon. Fractures of the surgical neck are most common and often associated with fractures of the greater tuberosity. There is often anterior and medial displacement of the shaft owing to the pull of the pectoralis major muscle. Fractures of the anatomic neck, though less common, have a higher potential for complication with avascular necrosis because of disruption of the blood supply to the humeral head. Atypical patterns of injury include isolated fractures of the tubercles and should elicit a search for signs of shoulder dislocation.
Alternatively, the Neer classification takes into account the number of fragments and degree of angulation and/or displacement. Fractures are classified as being one-, two-, three-, or four-part in nature. One-part fractures account for 80% of cases and are nondisplaced and stable injuries occurring most often at the surgical neck. Two-part injuries constitute 10% of all fractures, with the most common pattern being anterior and medial displacement of the shaft and fracture extension to the tubercles. Three-part fractures account for 3% of cases and are characterized by displaced fractures of the surgical neck associated with displaced fractures of either the lesser or greater tuberosity. Rotator cuff tears are common with this pattern of injury, requiring open reduction and repair of both the cuff and the fracture fragment. Lastly, four-part fractures account for about 4% of injuries and are characterized as severely comminuted fractures that may be associated with dislocation ( Fig. 14-12 ). These fractures often result in avascular necrosis. When fractures of the proximal humerus occur, they may be associated with other soft tissue injuries to the brachial plexus, axillary artery, and joint capsule.

Joint Emergencies
Acromioclavicular Joint
The acromioclavicular (AC) joint is the second most commonly dislocated joint in the shoulder, accounting for nearly 12% of all dislocations. The glenohumeral joint constitutes 85% of shoulder dislocations, and the sternoclavicular joint makes up the remaining 2% to 3% of dislocations. Dislocations of the AC joint most commonly occur between the ages of 15 and 40 years, usually precipitated by a fall onto an outstretched hand or directly by a fall on the point of the shoulder.
The Tossy and Allman classification is the most widely used classification describing injuries to the AC joint ( Fig. 14-13 ). In a type I separation, conventional radiographs appear normal or may show some soft tissue swelling over the joint. In a type II injury, there is disruption of the AC ligament and partial disruption of the coracoclavicular ligaments so that the clavicle migrates superiorly less than 5 mm or 50% of the width of the clavicle on weight-bearing views. In type III injuries the AC and coracoclavicular ligaments are completely disrupted, and there is clavicular migration exceeding 5 mm or 50% of the bone width. Rockwood and coworkers proposed three additional grades to the classification. In type IV injuries the clavicle displaces posteriorly into or through the trapezius muscle. In type V injuries, superior clavicle migration is more pronounced than in a type III separation. In type VI injuries the clavicle dislocates inferiorly below the coracoid or acromion process, often with associated rib fractures. Types IV to VI are extremely rare injury patterns.

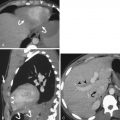
Sternoclavicular Joint
Dislocation of the sternoclavicular joint is uncommon but an important diagnosis. Dislocations are classified as either anterior or posterior, with anterior being more common. Anterior dislocations are caused by trauma to the anterior shoulder. With the clavicle acting essentially as a lever and the sternoclavicular joint as a fulcrum, the impact force is transmitted to the sternoclavicular joint, resulting in dislocation. Rarely, spontaneous dislocations may occur in patients with osteoarthrosis. Injuries of the sternoclavicular joint are often difficult to diagnose on standard AP radiographs, particularly with the overlapping mediastinal and spinal contours. The only clue to injury may be an offset of the medial ends of the clavicles appearing at different levels on standard frontal radiographs, but the direction of dislocation may be impossible to ascertain without CT. When using radiography, it is important to image both joints because comparison with the contralateral side is essential. Posterior dislocations are important because of associated soft tissue injuries ( Fig. 14-14 ). Complications include trauma to the vascular structures, hematoma formation, fractures of the regional skeleton, injury to the trachea and/or esophagus, and development of pneumomediastinum and/or pneumothorax.

Glenohumeral Joint
The glenohumeral joint is the most commonly dislocated joint in the body. The joint is anatomically predisposed to dislocation owing to the discrepancy between the large surface area of the humeral head and the significantly smaller surface area of the glenoid fossa. It is this configuration that allows for the large dynamic range of this joint. Dislocations are classified as anterior (subcoracoid, subglenoid, subclavicular, intrathoracic), posterior, inferior (luxatio erecta), and superior.
Anterior glenohumeral joint dislocations account for nearly 95% of glenohumeral joint injuries and are the result of an external rotation and abduction injury of the upper extremity. The most common type is a subcoracoid dislocation, which is characterized by anterior, inferior, and medial displacement of the humeral head beneath the coracoid process ( Fig. 14-15 ). Subglenoid dislocation is characterized by anterior, inferior, and more medial displacement with the humeral head resting beneath the inferior rim of the glenoid. Subclavicular anterior dislocation results in anterior, inferior, and even more medial displacement so that the humeral head terminates beneath the clavicle. Lastly, intrathoracic anterior dislocation occurs when the humeral head penetrates the intercostal space. Anterior glenohumeral joint dislocations are most commonly associated with impaction fractures in the posterosuperior aspect of the humeral head (Hill-Sachs deformity), occurring in as many as 75% of cases, and to the anterior/anteroinferior glenoid margin (Bankart lesion), seen in about 5% to 8% of cases. In addition, 15% of dislocations are associated with fractures of the greater tuberosity of the humerus ( Fig. 14-16 ).


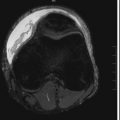
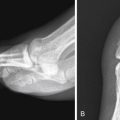
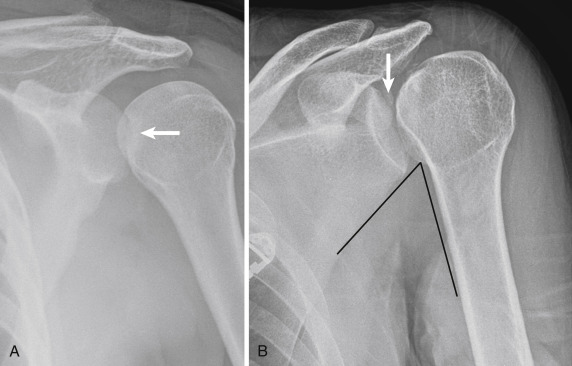
Posterior glenohumeral dislocations are uncommon, accounting for 2% to 4% of glenohumeral joint dislocations. The mechanism of injury is either a fall on an outstretched hand or a direct trauma to a flexed, adducted, and internally rotated shoulder, which forces the internally rotated humeral head posteriorly. When this occurs, the anterior aspect of the humeral head can impact the posterior glenoid margin. Classically associated with convulsive seizures, bilateral patterns of injury are common. Posterior dislocations are subtle and can be more challenging to diagnose. Nearly 50% to 60% of injuries are still missed on initial evaluation. Radiographic signs of injury include the arm remaining fixed in internal rotation (“lightbulb” sign), linear sclerosis of the medial humeral head with impaction deformity (“reverse Hill-Sachs deformity”; Fig. 14-17 ), and an injury to the posterior labrum (“reverse Bankart lesion”). Additional signs include loss of the normal overlap of the humeral head and glenoid margin on standard AP views (“crescent” sign), widening of the glenohumeral joint space more than 6 mm on standard AP views (“rim” sign), disrupted scapulohumeral arch, and a posteriorly dislocated humeral head on axillary views ( Fig. 14-18 ). There are two other fractures that are important in posterior dislocations. When a posterior glenoid rim fracture or a lesser tuberosity fracture is identified, a prior dislocation should be considered ( Fig. 14-19 ).


Inferior glenohumeral dislocations (luxatio erecta) occur as a result of headfirst fall onto a fully abducted outstretched arm, which causes impingement of the humerus against the acromion and levers the humeral head out from the glenoid fossa ( Fig. 14-20 ). Patients present with the upper extremity fixed in severe abduction, with their arm straight up as if asking a question. The radiographic appearance is pathognomonic, with the upper extremity fixed in abduction, the humeral head dislocated inferiorly to the glenoid, and the humeral shaft pointing superiorly and laterally. Associated injuries include tearing of the inferior capsule, tearing of the rotator cuff, injury to the brachial plexus, injury to the adjacent vasculature, and fractures of the surrounding regional skeleton (clavicle, coracoid, glenoid rim, greater tuberosity of the humerus).

Superior glenohumeral dislocations are a result of trauma to a flexed elbow while the arm is in adduction, resulting in superior dislocation of the humeral head, with the humeral head resting beneath the acromion process. Associated injuries include tearing of the joint capsule, tearing of the rotator cuff tendons, and fracture of the regional skeleton.
Elbow
- Jason E. Payne
- Joseph S. Yu
Anatomic Considerations and Mechanics
The elbow consists of three articulations confined within a single joint capsule: the ulnotrochlear, radiocapitellar, and proximal radioulnar joints. Each articulation allows a specific range of motion and provides a certain degree of stability. The ulnotrochlear articulation serves as the primary static stabilizer of the elbow, and its principal action is flexion-extension with a normal range of motion of approximately 0 to 140 degrees. The semispherical capitellum of the humerus articulates with the discoid radial head resulting in an axial-rotational joint. The radiocapitellar joint in conjunction with the proximal radioulnar articulation allows supination and pronation of the forearm ranging from 0 to 180 degrees.
Soft tissues also contribute to the stability of the elbow with the collateral ligament complexes representing important stabilizers of the elbow joint. The ulnar collateral ligament (UCL) is composed of the anterior, posterior, and transverse bands that originate on the medial epicondyle. The anterior band of the UCL is the most important resistor to valgus stress. The radial collateral ligament (RCL), lateral UCL, annular ligament, and accessory lateral collateral ligament compose the lateral collateral ligament complex. The RCL arises from the lateral epicondyle, blending with the annular ligament at the radial neck, and serves to prevent radial head displacement from the lesser sigmoid notch. The lateral UCL inserts on the supinator crest of the ulna preventing posterolateral rotatory instability.
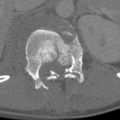
Fractures around the elbow account for approximately 5% of all skeletal fractures. The majority of fractures around the elbow are closed fractures. The patient’s age and sex may be predictive in the injury pattern. Many elbow injuries occur in skeletally immature patients. It is therefore important to recall the sequence of ossification in the pediatric elbow ( Fig. 14-21 ).