Key Points
- ▪
Knowledge of normal and variant anatomy of the upper extremity arterial vasculature is critical.
- ▪
A standardized and comprehensive duplex examination protocol is critical.
- ▪
Knowledge of possible diseases/lesions potentially within the upper extremity arterial vasculature, and how to maximize their recognition, is critical.
Arterial Anatomy of the Upper Extremity
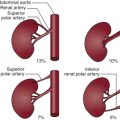
The arterial anatomy of the arm and the hand is depicted schematically in Figures 3-1 and 3-2 . The subclavian artery on the right side usually arises along with the common carotid artery from the innominate artery at the level of the sternoclavicular joint and in its distal extent rises slightly above the clavicle. However, variation may occur, such as the anomalous origin of the right subclavian artery directly from the descending aorta distal to the left subclavian artery and independently of the right common carotid artery.


On the left side, the subclavian artery arises from the distal arch of the aorta at the level of the fourth thoracic vertebra, and then arches laterally.
The main trunk of the subclavian artery is considered to be divided into three parts. The first part extends from the origin to the medial border of the scalene muscle. The second part lies behind the muscle. The third part extends from the lateral border of the scalene muscle and then over the first rib.
From the first segment and posterosuperior aspect of the subclavian artery arises the vertebral artery, the most constant of all its branches. The internal mammary artery arises from its inferior aspect, courses downward parasternally in a pedicle alongside its accompanying nerve and vein, and can become a useful collateral pathway along with its many vascular connections.
The thyrocervical trunk and its three branches, the inferior thyroid, transverse scapular, and superficial cervical arteries, the most important and variable of collateral pathways, supply flow around subclavian and innominate artery occlusive disease. These structures display the textbook configuration of a main trunk and three branches in only 46% of cases. The trunk is absent in 17% of cases.
Arising from the posterior aspect of the second part of the subclavian artery is the costocervical trunk, which passes above the pleura to the first rib, dividing into the deep cervical and superior intercostal to supply the first and second intercostal spaces. These vessels are small and are not considered to be significant collateral pathways. The third segment of the subclavian artery usually has no branches.
On each side of the body, the subclavian artery becomes the axillary artery at the level of the outer border of the first rib and the inferior border of the teres major muscle and then descends into the axilla. As with the subclavian artery, the axillary is divided into three parts: the first part lies medial to the pectoralis minor muscle, the second part behind it, and the third part on the lateral side of the muscle.
From 6 to 11 arteries may arise from the axillary artery and anastomose with each other to form a meshlike network that is effective as a collateral pathway in the presence of thoracic-scapular-humoral trauma. Although the configuration is fairly consistent, there is some variation related to the origin of these arteries. These arteries are the superior thoracic, thoracoacromial, lateral thoracic, subscapular, upper subscapular, and anterior and posterior circumflex humeral arteries.
At the level of the lower border of the teres major muscle, the brachial artery begins, leaving the axilla and running downward and medially to the humerus. Where this artery reaches the elbow joint, where it is positioned midway between the epicondyles, it comes in front of the humerus.
The brachial artery has several branches along its course, forming important potential pathways around the elbow and, occasionally, a superficial brachial artery (9% incidence). When present, the superficial brachial artery may either replace the brachial artery or parallel it down the arm and continue as the radial or rarely, the ulna artery. Smaller branch vessels supply the muscles of the arm, and the majority of them are nameless.
The brachial artery bifurcates into the ulnar artery and the radial artery at approximately 1.5 cm distal to the radiohumeral line, with the ulnar artery most often being the deeper and more dominant vessel. In 13% to 25% of cases, the radial artery has a variable origin arising from the axillary artery or from the proximal, mid-, or distal brachial artery. It is most often unilateral and is then called the brachioradial artery. In this same sample of patients, a brachioulnar artery was present in 5% with the same pattern of origin as the brachioradial artery.
Other anomalous vessel origins of lesser significance have been identified in both the upper arm and forearm, and absent or rudimentary ulnar and radial arteries have been reported but is considered rare. When either the radial or ulnar arteries are absent, there function is replaced by anterior interosseous artery.
The ulnar artery is the more dominant of the two forearm arteries. Although the radial artery gives off only small branches that supply the musculature of the forearm, the ulna artery has a large branch, the common interosseous artery, which divides and delivers branches to both sides of the interosseous membrane.
The more superficial radial artery runs downward beneath the brachioradialis muscle and extends into the hand, where the deep palmar arch is formed by the anastomosis of a deep palmar branch of the ulna artery with the radial artery. This arch is complete in 97% of cases, and this results in an excellent collateral network for the hand.
The ulnar artery lies between the deep and superficial flexor muscles and continues down the arm to the hand, where it joins the superficial palmar branch of the radial artery to form the superficial palmar arch. The arch is incomplete in 20% of cases. The perforating branches of the deep palmar arch are thought to be responsible for blood supply to the dorsum of the hand, and the recurrent branches from the deep arch are thought to be the collateral supply when the radial and ulnar arteries are ligated.
The digital arteries are formed by the volar metacarpal arteries from the deep arch, the dorsal metacarpals from the perforating arteries, the common volar digitals from the superficial arch, and the dorsal branch of the radial artery.
Recommendations for the management of patients with occlusive disease of the subclavian and brachiocephalic arteries are given in Box 3-1 .
Class IIa
- 1.
Extra-anatomic carotid-subclavian bypass is reasonable for patients with symptomatic posterior cerebral or cerebellar ischemia caused by subclavian artery stenosis or occlusion (subclavian steal syndrome) in the absence of clinical factors predisposing to surgical morbidity or mortality (690–692). ( Level of Evidence: B )
- 2.
Percutaneous endovascular angioplasty and stenting is reasonable for patients with symptomatic posterior cerebral or cerebellar ischemia caused by subclavian artery stenosis (subclavian steal syndrome) who are at high risk of surgical complications. ( Level of Evidence: C )
- 3.
Revascularization by percutaneous angioplasty and stenting, direct arterial reconstruction, or extra-anatomic bypass surgery is reasonable for patients with symptomatic ischemia involving the anterior cerebral circulation caused by common carotid or brachiocephalic artery occlusive disease. ( Level of Evidence: C )
- 4.
Revascularization by percutaneous angioplasty and stenting, direct arterial reconstruction, or extra-anatomic bypass surgery is reasonable for patients with symptomatic ischemia involving upper-extremity claudication caused by subclavian or brachiocephalic artery occlusive disease. ( Level of Evidence: C )
- 5.
Revascularization by either extra-anatomic bypass surgery or subclavian angioplasty and stenting is reasonable for asymptomatic patients with subclavian artery stenosis when the ipsilateral internal mammary artery is required as a conduit for myocardial revascularization. ( Level of Evidence: C )
Class III: No Benefit
- 1.
Asymptomatic patients with asymmetrical upper-limb blood pressure, periclavicular bruit, or flow reversal in a vertebral artery caused by subclavian artery stenosis should not undergo revascularization unless the internal mammary artery is required for myocardial revascularization. ( Level of Evidence: C )
Duplex Evaluation of the Upper Extremity Arteries
The purpose of duplex evaluation is to identify the presence or absence of occlusive or aneurysmal disease and, subsequently, to determine extent and degree. Common indications include:
- □
Upper extremity ischemia
- □
Asymmetrical brachial systolic blood pressure readings
- □
Suspected upper extremity arterial embolism
- □
Reduced pulses
- □
Bruit
- □
Suspected subclavian “steal”
- □
Evaluation of arterial trauma
- □
Thoracic outlet syndrome (evaluation is under a separate protocol)
The most common contraindication to duplex examination is the presence of wound dressings.
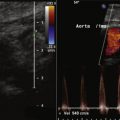
Several examples of normal and abnormal scans are shown in Figures 3-3 to 3-12 .






Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree