Upper extremity arteries are affected by a myriad of vascular disorders. Atherosclerosis is the most common arterial disease, but other conditions, such as vasculitis, chronic repetitive traumatic injuries, and trauma, constitute a significant portion of the arterial diseases. This chapter summarizes the salient features of these disorders.
Atherosclerosis
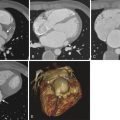
Atherosclerosis is less commonly encountered in the upper extremities than in the lower extremities. The risk factors for atherosclerosis include diabetes, hypercholesterolemia, smoking, and hypertension. Subclinical disease is common, but symptomatic disease is rare given the small muscle mass and lower demand for oxygen in the upper extremities. Asymptomatic disease is often discovered when asymmetrical arm blood pressures are found during clinical examination. Symptoms include arm pain with exertion, rest pain, and digit ulceration. Coldness, nail and skin atrophy, and hair loss can be indicative of long-term ischemic change. Patients with proximal subclavian artery stenosis may have symptoms of subclavian steal syndrome—dizziness, vertigo, and syncope during arm exertion ( Fig. 47-1 ). Similarly, ischemic symptoms may occur following creation of an arteriovenous fistula or graft in the upper extremity that steals the blood and brings out subclinical atherosclerotic disease caused by decreased flow to the distal arterial bed ( Fig. 47-2 ).
A clinical diagnosis of upper extremity arterial stenosis may be suspected when a blood pressure difference of greater than 10 mm Hg between the arms is identified during physical examination. Noninvasive vascular laboratory tests such as segmental limb pressures, pulse volume recordings, and wrist-brachial index measurement should be performed. On measurement of segmental limb pressures, a difference of greater than 10 mm Hg between the arms suggests proximal disease affecting the brachiocephalic or subclavian or axillary arteries, whereas a difference of greater than 10 to 20 mm Hg between the successive arm levels suggests intervening occlusive disease. On pulse volume recordings, mild disease is characterized by loss of dicrotic notch and an outward bowing of the downstroke. Decreased amplitude of the waveform suggests severe disease. The normal wrist-brachial index is 1.0 and a value of less than 0.85 is indicative of arterial disease. Noninvasive tests after exercise are helpful to detect subclinical disease. Similarly, vasospastic disorders can be tested after exposing the hands to the appropriate stimuli (cold water in cases of Raynaud syndrome).
Imaging evaluation of upper extremity atherosclerosis can be performed with duplex ultrasonography, computed tomography angiography (CTA), and magnetic resonance angiography (MRA). Catheter angiography is reserved for evaluation of small vessel disease in the hand and for interventions. An occlusion is suspected on duplex ultrasonography with appropriate technical settings (low pulse repetition frequency and appropriate wall filters) when there is no color flow on color Doppler and absence of flow on spectral Doppler. A stenosis of 50% or more luminal narrowing is suspected when the peak systolic velocity at the site of narrowing is more than two times that of the proximal normal segment. A ratio of the peak systolic velocity in the stenotic segment to the peak systolic velocity in the proximal normal segment that is more than 4:1 suggests greater than 75% luminal narrowing. The waveforms distal to the stenosis show decreased peak systolic velocity, increased acceleration time (tardus parvus pattern), and monophasic flow pattern. The proximal subclavian artery is often difficult to evaluate with duplex ultrasonography. However, the presence of a hemodynamically significant stenosis can be suspected when a tardus parvus monophasic waveform is seen in the distal subclavian artery or the axillary artery. A reversal of flow in the vertebral artery may be seen if the stenosis is proximal to the origin of the vertebral artery. This is often referred to as subclavian steal syndrome. In patients with a coronary bypass graft using the internal mammary artery, coronary-subclavian steal may occur, wherein there is reversal of flow through the internal mammary artery on duplex ultrasonography with exertion of the upper extremity.
CTA with multidetector computed tomography is highly accurate in localization and estimation of percentage of stenosis or occlusion of peripheral arterial disease affecting the upper extremity (see Fig. 47-1 ). Caution should be exercised when performing these studies. The contrast material should be injected through the asymptomatic arm to prevent streak artifacts from the contrast material–filled subclavian veins. Plaques are identified as mural-adherent calcified or noncalcified linear structures protruding into the lumen. Ulceration of the plaque may be seen as a central or paracentral acutely angulated depression within the plaque surface. Occlusions may be seen as filling defects within the arteries. Collateral vessels may be identified in the presence of occlusion or hemodynamically significant stenosis. As with other locations in the body, atherosclerosis tends to affect the vessel origins and bifurcation points.
MRA with gadolinium is one of the best methods of assessing the extent of atherosclerotic disease in the upper extremities ( Fig. 47-3 ). Noncontrast methods are not adequate for the assessment of proximal subclavian artery disease; however, the reversal of flow in the vertebral arteries may be seen with two-dimensional time of flight sequences. Arterial disease affecting the arm and forearm may be assessed with various noncontrast methods; however, the arteries of the hand require high-resolution imaging that is often inadequate on noncontrast MRA. Time-resolved techniques allow detection of collateral flow pattern and help assess the hemodynamic significance of a stenosis.

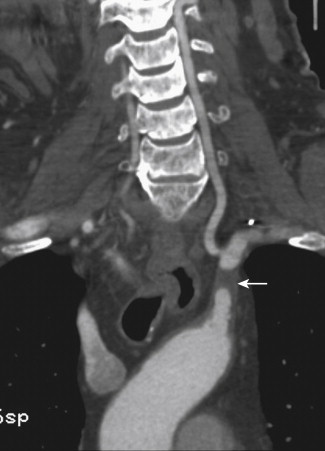
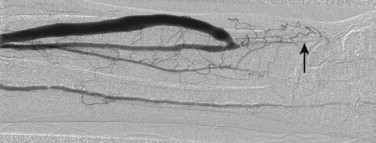
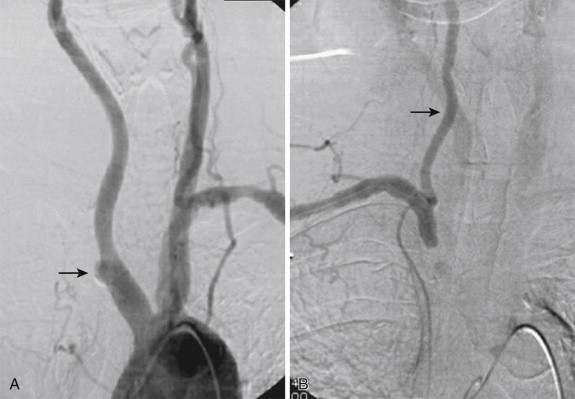
Catheter angiography is reserved for assessment of small vessels in the hand. Digital arterial occlusive disease secondary to atherosclerosis is common but rarely symptomatic, unless the disease is severe or the proximal arterial flow is diverted (such as after creation of an arteriovenous fistula or graft in patients with renal failure), when it leads to gangrene or ulceration of the fingers. Catheter angiography may demonstrate luminal narrowing, irregularity of the luminal surface in the presence of ulcerated plaques, collateral flow, and arterial occlusions ( Fig. 47-4 ). Catheter angiography of the carotid arteries demonstrates the reversal of flow in the vertebral artery in the presence of proximal subclavian artery stenosis ( Fig. 47-5 ). Similarly, coronary angiography may demonstrate reversal of flow through the internal mammary artery bypass graft in patients with coronary-subclavian steal syndrome. Catheter angiography is part of endovascular and open interventional procedures on the blood vessels. It is useful for assessing the patency of stents and bypass grafts (see Fig. 47-4 ).
Pearls and Pitfalls
- 1.
Upper extremity atherosclerosis is often subclinical, rarely causes symptoms, and is incidentally discovered on physical examination when a difference in blood pressure between the arms prompts further investigation.
- 2.
Proximal subclavian artery disease leads to subclavian steal syndrome; patients have dizziness, vertigo, and syncope, especially after upper extremity exertion. Duplex ultrasonography, MRA, and catheter angiography are helpful in diagnosing this condition.
- 3.
Digital artery atherosclerosis is best evaluated with catheter angiography.
- 4.
Steal phenomenon from hemodialysis fistula or graft is best assessed through angiography. A catheter is positioned above the level of the arteriovenous anastomosis, and contrast material is injected before and after compression of the venous outflow. A significant improvement of distal flow with venous outflow occlusion and immediate improvement in clinical symptoms suggest steal phenomenon.
Nonatherosclerotic, Noninflammatory Arterial Occlusive Disease
Dissection
Dissection affecting the upper extremity arteries is usually secondary to extension of an aortic dissection. It usually affects the brachiocephalic and subclavian arteries, and rarely does this extend to the axillary artery. Isolated dissections without the involvement of the aorta should raise the possibility of collagen vascular disorders such as Marfan and Ehlers-Danlos syndromes. Dissections involving the brachial and forearm arteries are rare and are usually secondary to trauma or vascular interventions ( Fig. 47-6 ). Dissection flap is rarely visible on ultrasonography but can be well recognized on CTA and MRA. The true lumen is recognized by its small size and early filling with contrast material.

Fibromuscular Dysplasia
Fibromuscular dysplasia affects the medium and small arteries. Commonly observed in young and middle-aged females, it affects the renal arteries, extracranial cerebral arteries, iliofemoral arteries, and splanchnic arteries. Upper extremity arteries are rarely affected. Among the upper extremity arteries, the subclavian artery is the most commonly affected artery, followed by the brachial, axillary, and forearm arteries. Patients are usually asymptomatic, and the disease is discovered incidentally on imaging. Rarely patients may present with distal embolism. Duplex ultrasonography, CTA, and MRA may show the beaded appearance of the artery ( Fig. 47-7 ). Ultrasonography is useful to assess the presence of hemodynamically significant stenosis. Catheter angiography confirms the diagnosis (see Fig. 47-7 ). Both upper extremities should be assessed to rule out the presence of bilateral disease (see Fig. 47-7 ). In addition, evaluation of the renal and carotid arteries must be performed to detect the presence of subclinical disease in these territories, because fibromuscular dysplasia tends to involve multiple territories in one third of the patients. Hemodynamically significant, symptomatic lesions respond well to angioplasty.

Raynaud Syndrome
In this condition an abnormal vasoconstriction of the digital arteries to cold temperature or emotional stress results in color changes in the skin of the digits. With exposure to cold temperature the digits become cold, with sharply demarcated pallor (paleness) or cyanosis (blue discoloration), or both. With rewarming the skin becomes red because of reperfusion. The symptoms usually involve a single finger and spread to other fingers symmetrically in both hands. Patients may complain of numbness, ache, or a sensation of pins and needles. Diagnosis is usually clinical, but noninvasive vascular tests and color Doppler ultrasonography may demonstrate changes in the digital flow. Such changes include decreased amplitude on pulse volume recordings in the digits in response to exposure to cold temperature ( Fig. 47-8 ) and decreased amplitude with monophasic flow and absent diastolic flow on Doppler ultrasonography. Catheter angiography may also demonstrate vascular spasm of the digital arteries with exposure to cold that reverses on rewarming. The secondary form of Raynaud syndrome refers to the presence of underlying diseases such as atherosclerosis or connective tissue disorders that disrupt the normal complex regulation of regional blood flow to the digits and skin.

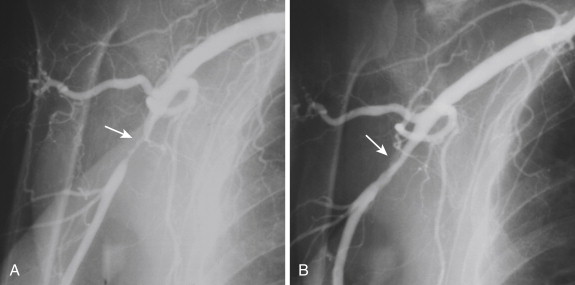
Frostbite
Frostbite is a severe localized cold-induced injury resulting from freezing of tissue on exposure to cold weather. On exposure to subfreezing temperatures, ice crystals form extracellularly and sometimes intracellularly, leading to cellular disruption and inflammation. Depending on the severity, frostbite is classified into first degree (superficial involvement with pallor and anesthesia of the skin), second degree (blisters with edema and erythema), third degree (hemorrhagic blisters with black skin eschar), and fourth degree (complete tissue necrosis involving muscles and bone). There is associated vascular thrombosis of the affected tissue. Vascular occlusion may be seen on MRA. However, catheter angiography is highly sensitive in identifying the extent of vascular occlusion in the hands (Fig.47-9, A ) and for institution and follow-up of thrombolytic therapy ( Fig.47-9 , B ).