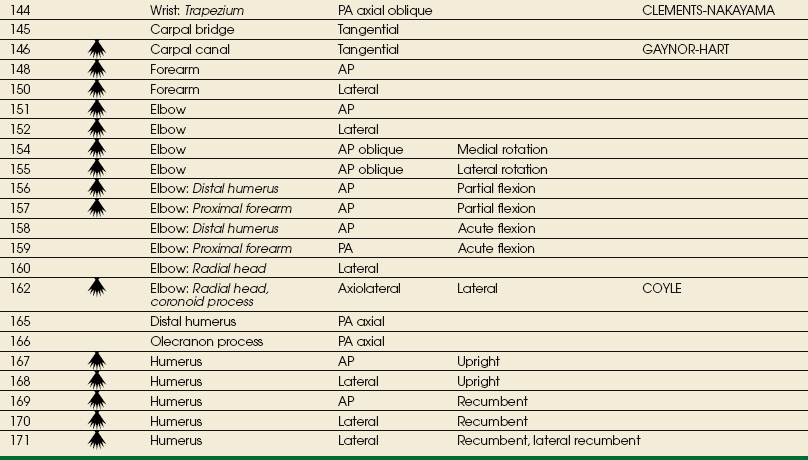
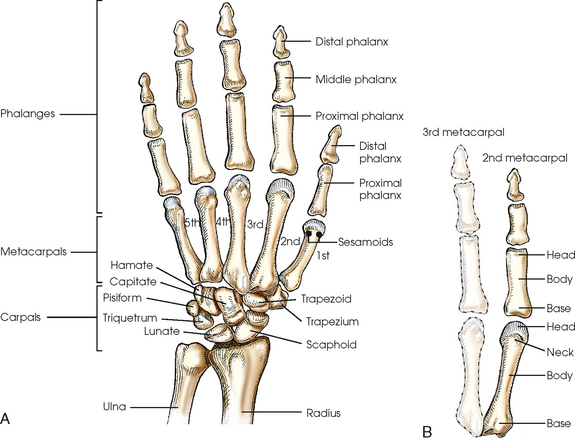
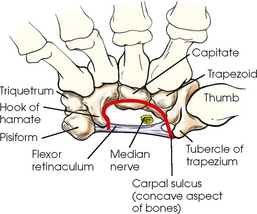
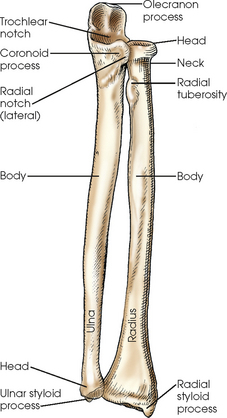
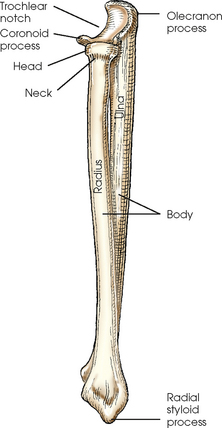
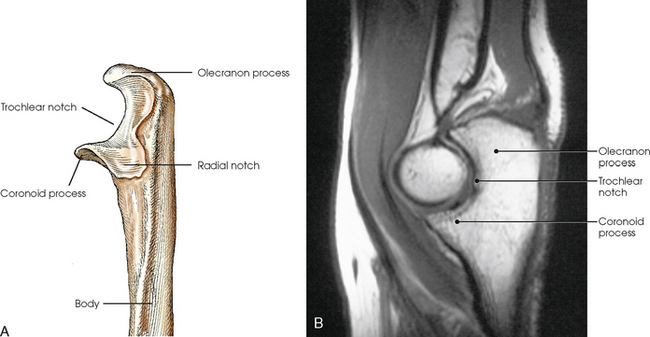
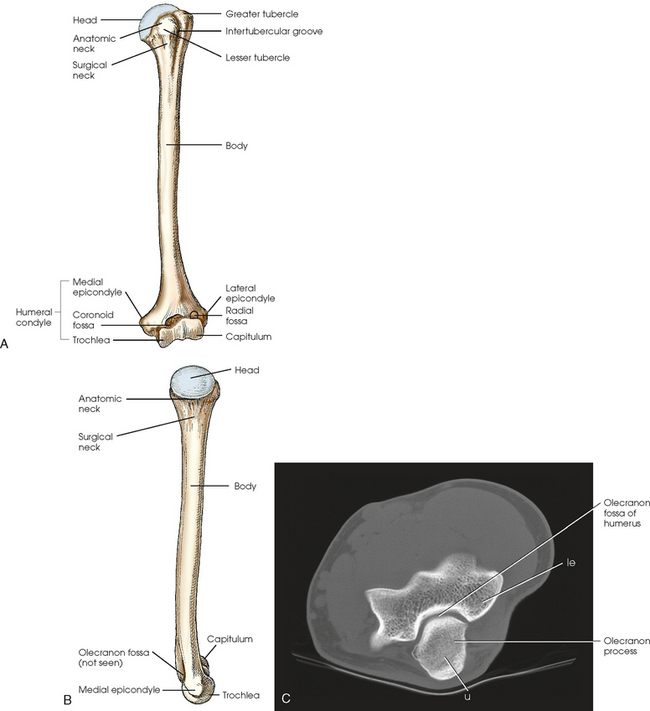
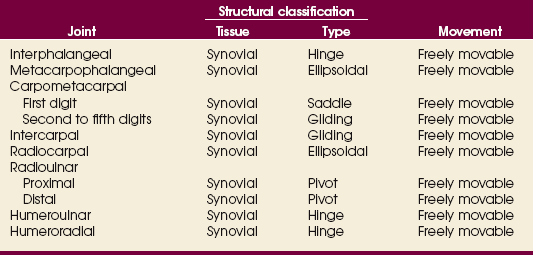
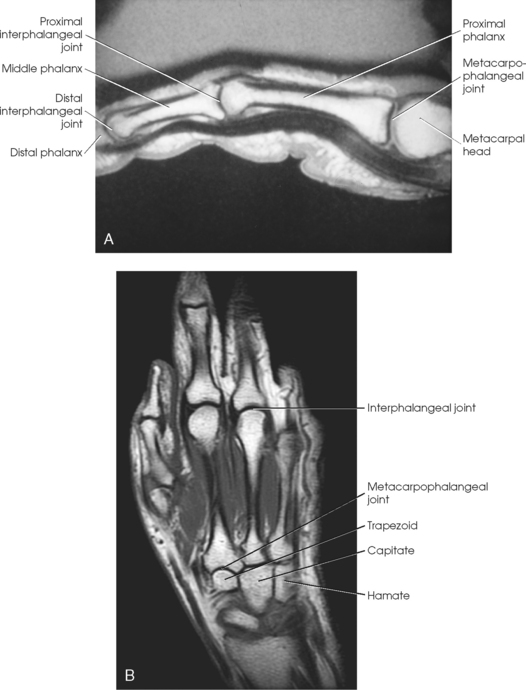
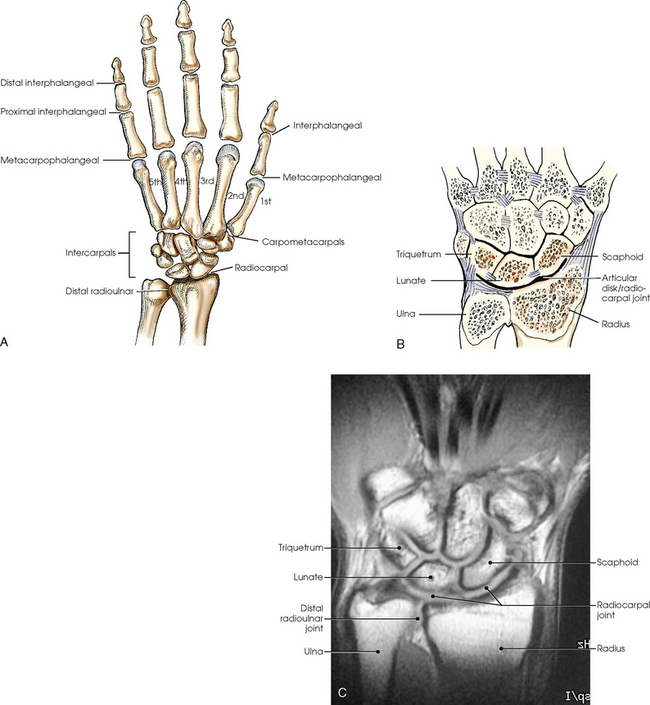
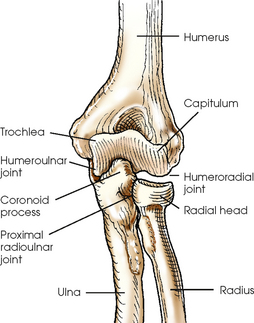
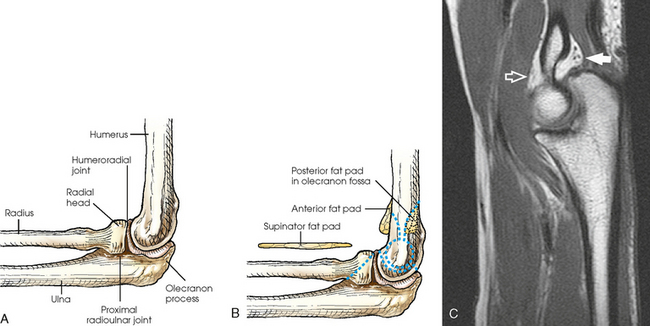
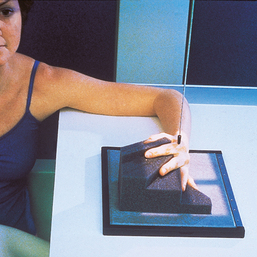
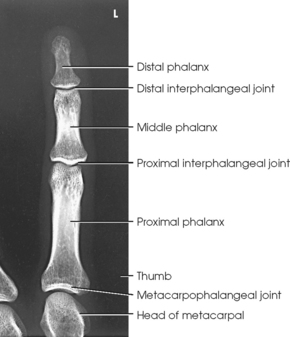
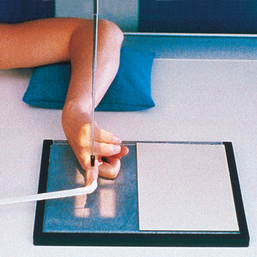
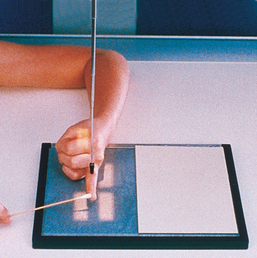
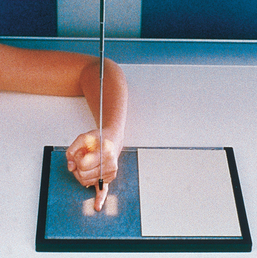
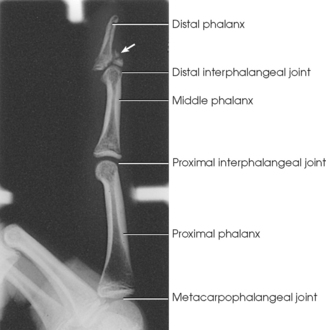
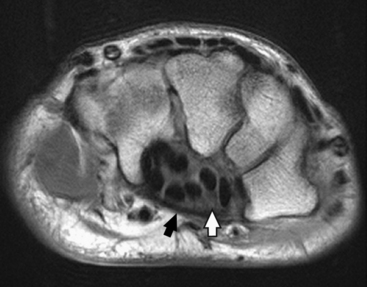
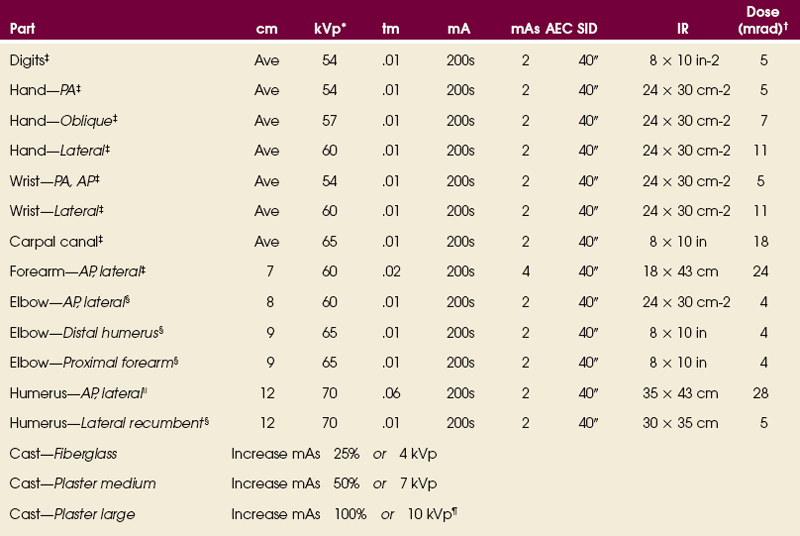
4 Anatomists divide the bones of the upper limbs, or extremities, into the following main groups: The proximal arm and shoulder girdle are discussed in Chapter 5. The hand consists of 27 bones, which are subdivided into the following groups: • Phalanges: Bones of the digits (fingers and thumb) • Metacarpals: Bones of the palm • Carpals: Bones of the wrist (Fig. 4-1) Five metacarpals, which are cylindric in shape and slightly concave anteriorly, form the palm of the hand (see Fig. 4-1). They are long bones consisting of a body and two articular ends—the head distally and the base proximally. The area below the head is the neck where fractures often occur. The first metacarpal contains two small sesamoid bones on its palmar aspect below the neck (see Fig. 4-1). A single sesamoid is often seen at this same level on the second metacarpal. The metacarpal heads, commonly known as the knuckles, are visible on the dorsal hand in flexion. The metacarpals are also numbered 1 to 5, beginning from the lateral side of the hand. The wrist has eight carpal bones, which are fitted closely together and arranged in two horizontal rows (see Fig. 4-1). The carpals are classified as short bones and are composed largely of cancellous tissue with an outer layer of compact bony tissue. These bones, with one exception, have two or three names; this atlas uses the preferred terms (see box). The proximal row of carpals, which is nearest the forearm, contains the scaphoid, lunate, triquetrum, and pisiform. The distal row includes the trapezium, trapezoid, capitate, and hamate. The anterior or palmar surface of the wrist is concave from side to side and forms the carpal sulcus (Figs. 4-2 and 4-3). The flexor retinaculum, a strong fibrous band, attaches medially to the pisiform and hook of hamate and laterally to the tubercles of the scaphoid and trapezium. The carpal tunnel is the passageway created between the carpal sulcus and flexor retinaculum. The median nerve and the flexor tendons pass through the carpal canal. Carpal tunnel syndrome results from compression of the median nerve inside the carpal tunnel. Fig. 4-2 Axial MRI of wrist. Bones in same position as in Fig. 4-3. Note arched position of carpal bones and carpal sulcus protecting tendons of fingers (black circles within sulcus) and median nerve (white arrow). Flexor retinaculum (black arrow) is also seen. The forearm contains two bones that lie parallel to each other—the radius and ulna. Similar to other long bones, they have a body and two articular extremities. The radius is located on the lateral side of the forearm, and the ulna is located on the medial side (Figs. 4-4 and 4-5). The body of the ulna is long and slender and tapers inferiorly. The upper portion of the ulna is large and presents two beaklike processes and concave depressions (Fig. 4-6). The proximal process, or olecranon process, concaves anteriorly and slightly inferiorly and forms the proximal portion of the trochlear notch. The more distal coronoid process projects anteriorly from the anterior surface of the body and curves slightly superiorly. The process is triangular and forms the lower portion of the trochlear notch. A depression called the radial notch is located on the lateral aspect of the coronoid process. The arm has one bone called the humerus, which consists of a body and two articular ends (Fig. 4-7, A and B). The proximal part of the humerus articulates with the shoulder girdle and is described further in Chapter 5. The distal humerus is broad and flattened and presents numerous processes and depressions. The entire distal end of the humerus is called the humeral condyle and includes two smooth elevations for articulation with the bones of the forearm—the trochlea on the medial side and the capitulum on the lateral side. The medial and lateral epicondyles are superior to the condyle and easily palpated. On the anterior surface superior to the trochlea, a shallow depression called the coronoid fossa receives the coronoid process when the elbow is flexed. The relatively small radial fossa, which receives the radial head when the elbow is flexed, is located lateral to the coronoid fossa and proximal to the capitulum. The olecranon fossa is a deep depression found immediately behind the coronoid fossa on the posterior surface and accommodates the olecranon process when the elbow is extended (Fig. 4-7, C). The proximal end of the humerus contains the head, which is large, smooth, and rounded and lies in an oblique plane on the superomedial side. Just below the head, lying in the same oblique plane, is the narrow, constricted anatomic neck. The constriction of the body just below the tubercles is called the surgical neck, which is the site of many fractures. Table 4-1 contains a summary of the joints of the upper limb. A detailed description of the upper limb articulations follows. The interphalangeal (IP) articulations between the phalanges are synovial hinge type and allow only flexion and extension (Fig. 4-8). The IP joints are named by location and are differentiated as either proximal interphalangeal (PIP) or distal interphalangeal (DIP), by the digit number, and by right or left hand (e.g., the PIP articulation of the fourth digit of the left hand) (Fig. 4-9, A and B). Because the first digit has only two phalanges, the joint between the two phalanges is simply called the IP joint. The carpals articulate with each other, the metacarpals, and the radius of the forearm. In the carpometacarpal (CMC) articulations, the first metacarpal and trapezium form a synovial saddle joint, which permits the thumb to oppose the fingers (touch the fingertips). The articulations between the second, third, fourth, and fifth metacarpals and the trapezoid, capitate, and hamate form synovial gliding joints. The intercarpal articulations are also synovial gliding joints. The articulations between the lunate and scaphoid form a gliding joint. The radiocarpal articulation is a synovial ellipsoidal type. This joint is formed by the articulation of the scaphoid, lunate, and triquetrum, with the radius and the articular disk just distal to the ulna (Fig. 4-9, C). The distal and proximal radioulnar articulations are synovial pivot joints. The distal ulna articulates with the ulnar notch of the distal radius. The proximal head of the radius articulates with the radial notch of the ulna at the medial side. The movements of supination and pronation of the forearm and hand largely result from the combined rotary action of these two joints. In pronation, the radius turns medially and crosses over the ulna at its upper third, and the ulna makes a slight counterrotation that rotates the humerus medially. The elbow joint proper includes the proximal radioulnar articulation and the articulations between the humerus and the radius and ulna. The three joints are enclosed in a common capsule. The trochlea of the humerus articulates with the ulna at the trochlear notch. The capitulum of the humerus articulates with the flattened head of the radius. The humeroulnar and humeroradial articulations form a synovial hinge joint and allow only flexion and extension movement (Figs. 4-10 and 4-11, A). The proximal humerus and its articulations are described with the shoulder girdle in Chapter 5. The three areas of fat1,2 associated with the elbow joint can be visualized only in the lateral projection (Fig. 4-11, B and C). The posterior fat pad covers the largest area and lies within the olecranon fossa of the posterior humerus. The superimposed coronoid and radial fat pads, which lie in the coronoid and radial fossae of the anterior humerus, form the anterior fat pad. The supinator fat pad is positioned anterior to and parallel with the anterior aspect of the proximal radius. When the elbow is flexed 90 degrees for the lateral projection, only the anterior and supinator fat pads are visible, and the posterior fat pad is depressed within the olecranon fossa. The anterior fat pad resembles a teardrop, and the supinator fat pad appears as shown in Fig. 4-11, B. The fat pads become significant radiographically when an elbow injury causes effusion and displaces the fat pads or alters their shape. Visualization of the posterior fat pad is a reliable indicator of elbow pathology. Exposure factors designed to show soft tissues are extremely important on lateral elbow radiographs because visualization of the fat pads may be the only evidence of injury. *kVp values are for a three-phase, 12-pulse or high-frequency generator. †Relative doses for comparison use. All doses are skin entrance for average adult at cm indicated. ‡Tabletop, extremity IR. Screen-film speed 100. §Tabletop, standard IR. Screen-film speed 300. |Bucky, 16:1 grid. Screen-film speed 300 or equivalent CR. ¶Gratale P, Turner GW, Burns CB: Using the same exposure factors for wet and dry casts, Radiol Technol 57:328, 1986. When the upper limb is radiographed, the following steps should be initiated: • Remove rings, watches, and other radiopaque objects, and place them in secure storage during the procedure. • Seat the patient at the side or end of the table to avoid a strained or uncomfortable position. • Place the IR at a location and angle that allows the patient to be in the most comfortable position. Because the degree of immobilization (particularly of the hand and digits) is limited, the patient must be comfortable to promote relaxation and cooperation in maintaining the desired position. • Unless otherwise specified, direct the central ray at a right angle to the midpoint of the IR. Because the joint spaces of the limbs are narrow, accurate centering is essential to avoid obscuring the joint spaces. • Radiograph each side separately when performing a bilateral examination of the hands or wrists; this prevents distortion, particularly of the joint spaces. • Shield gonads from scattered radiation with a sheet of lead-impregnated rubber or a lead apron placed over the patient’s pelvis (Fig. 4-12). • Use close collimation. This technique is recommended for all upper limb radiographs. • Placing multiple exposures on one IR is a common practice. The side of the unexposed IR should always be covered with lead, especially when the new computed radiography IRs are used. • Use right or left markers and all other vital identification markers when appropriate. Position of part: When radiographing individual digits (except the first), take the following steps: • Because lateral digit positions are difficult to hold, tell the patient how the digit is adjusted on the IR and demonstrate with your own finger. Let the patient assume the most comfortable arm position. • Ask the patient to extend the digit to be examined. Close the rest of the digits into a fist and hold them in complete flexion with the thumb. • Support the elbow on sandbags or provide other suitable support when the elbow must be elevated to bring the digit into position. • With the digit under examination extended and other digits folded into a fist, have the patient’s hand rest on the lateral, or radial, surface for the second or third digit (Figs. 4-20 and 4-21) or on the medial, or ulnar, surface for the fourth or fifth digit (Figs. 4-22 and 4-23). • Before making the final adjustment of the digit position, place the IR so that the midline of its unmasked portion is parallel with the long axis of the digit. Center the IR to the PIP joint. • Rest the second and fifth digits directly on the IR, but for an accurate image of the bones and joints, elevate the third and fourth digits and place their long axes parallel with the plane of the IR. A radiolucent sponge may be used to support the digits. • Immobilize the extended digit by placing a strip of adhesive tape, a tongue depressor, or other support against its palmar surface. The patient can hold the support with the opposite hand. • Adjust the anterior or posterior rotation of the hand to obtain a true lateral position of the digit.
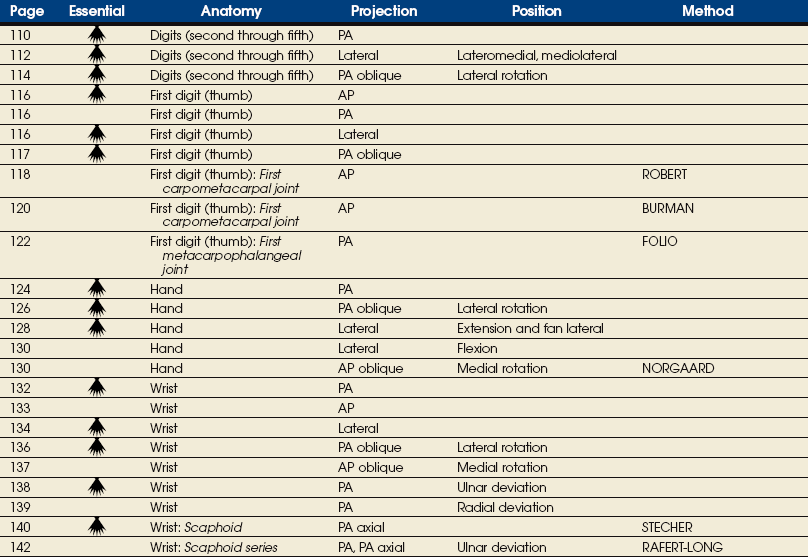
UPPER LIMB

ANATOMY
Hand
METACARPALS
WRIST
CARPAL SULCUS
Forearm
ULNA
Arm
Upper Limb Articulations
Fat Pads
EXPOSURE TECHNIQUE CHART ESSENTIAL PROJECTIONS
SUMMARY OF PATHOLOGY
Condition
Definition
Bone cyst
Fluid-filled cyst with wall of fibrous tissue
Bursitis
Inflammation of bursa
Dislocation
Displacement of bone from joint space
Fracture
Disruption in continuity of bone
Bennett
Fracture at base of first metacarpal
Boxer’s
Fracture of metacarpal neck
Colles
Fracture of distal radius with posterior (dorsal) displacement
Smith
Fracture of distal radius with anterior (palmar) displacement
Torus or buckle
Impacted fracture with bulging of periosteum
Gout
Hereditary form of arthritis in which uric acid is deposited in joints
Joint effusion
Accumulation of fluid in joint associated with underlying condition
Metastases
Transfer of cancerous lesion from one area to another
Osteoarthritis or degenerative joint disease
Form of arthritis marked by progressive cartilage deterioration in synovial joints and vertebrae
Osteomyelitis
Inflammation of bone owing to pyogenic infection
Osteopetrosis
Increased density of atypically soft bone
Osteoporosis
Loss of bone density
Rheumatoid arthritis
Chronic, systemic, inflammatory collagen disease
Tumor
New tissue growth where cell proliferation is uncontrolled
Chondrosarcoma
Malignant tumor arising from cartilage cells
Enchondroma
Benign tumor consisting of cartilage
Ewing sarcoma
Malignant tumor of bone arising in medullary tissue
Osteosarcoma
Malignant, primary tumor of bone with bone or cartilage formation
General Procedures
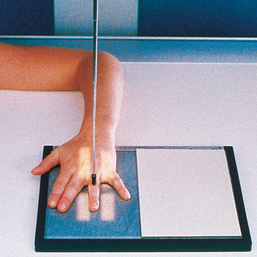
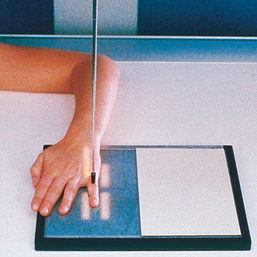
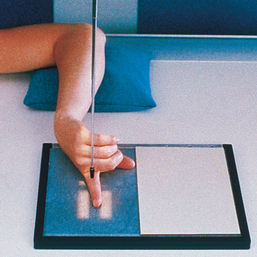
Digits (Second Through Fifth)
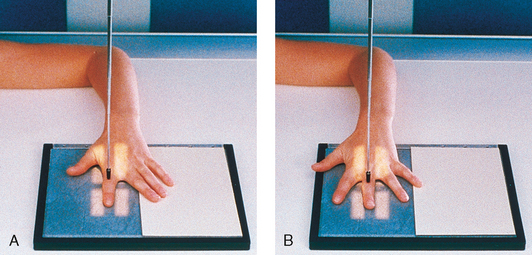
![]() LATERAL PROJECTION
LATERAL PROJECTION