Urethra and Penis
▪ NORMAL MALE URETHRA
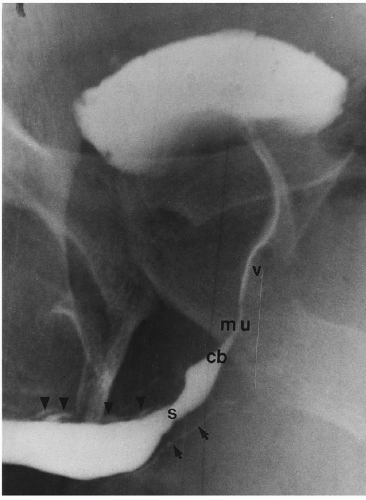
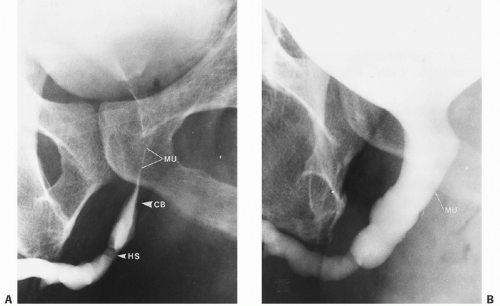
Although the normal anatomy of the male urethra has been described in Chapter 1, a brief review of urethral anatomy as defined by radiographic landmarks is in order before discussing urethral strictures and tumors. During dynamic retrograde urethrography, the entire urethra can be visualized (Fig. 17.1A). If properly performed, contrast medium can be seen jetting through the bladder neck (BN) into the bladder. The verumontanum is seen as an ovoid filling defect in the posterior (prostatic) urethra. The distal end of the verumontanum marks the proximal boundary of the membranous urethra (MU). The distal boundary of the MU is the conical tip of the bulbar urethra. The MU is approximately 1 cm in length and is that portion of the urethra that passes through the urogenital diaphragm. This is also the region of the external sphincter of the urethra. The anterior urethra extends from its junction with the MU to the urethral meatus. It is divided into the bulbar (most dependent) segment and the penile or pendulous segment. There is usually mild angulation of the urethra where these two segments join at the penoscrotal junction.
On voiding studies, the BN opens widely and becomes funnel shaped (Fig. 17.1B). Although the verumontanum usually still can be seen, the proximal bulbar urethra has less of a conical appearance. However, the MU remains the narrowest segment between these parts of the urethra, although it may dilate up to 6 or 7 mm in diameter during voiding.
MU LANDMARKS
Proximal: Distal end of verumontanum
Distal: Conical tip of bulbar urethra
The landmarks of the MU must be recognized so that it can be accurately located on retrograde or voiding studies. Normal urethral landmarks must be identified so that they are not confused with a pathologic stricture (Fig. 17.2).
▪ ACQUIRED URETHRAL STRICTURES IN MEN
Gonorrhea
Gonorrhea is a sexually transmitted disease more prevalent in underdeveloped countries where low-hygienic standards prevail; sexual promiscuity is a major contributing factor. The estimated number of cases of gonorrhea in North America in 1974 reached 2.7 million. Since the early 1980s, sexual promiscuity has decreased because of fear of acquired immunodeficiency syndrome, and the incidence of gonorrhea has decreased to approximately 800,000 cases per year. Early antibiotic treatment of gonorrhea eradicates the disease without sequelae. No treatment or inadequate treatment results in a chronic inflammatory reaction that can cause a urethral stricture.
Approximately 40% of all urethral strictures in the United States are caused by gonorrhea, whereas the remainder are caused by other diseases such as chlamydia or mycoplasma, tuberculosis, schistosomiasis, tumor, trauma, or iatrogenic injury.
Gonococcus ascends the anterior urethra after sexual contact with an infected partner, affecting the columnar epithelial cells, which become congested. The submucosal glands of Littré, which line the anterior urethra and have a lubricating function, become infected and produce a thick, purulent urethral discharge within 48 hours after exposure. Without adequate treatment, the infection extends into the corpus spongiosum surrounding the anterior urethra, resulting in venous thrombosis and surrounding tissue necrosis. Granulation tissue develops where columnar cells have desquamated and sloughed. The combination of necrosis and granulation develops into fibrous scarring that is more prominent in the bulbar urethra, owing to less effective flushing by urination and the preponderance of glands of Littré in this area. Over a period of months or years, the scarring becomes irregular. Some scarring is hard-fibrous tissue that is difficult to dilate, whereas other scarring is softer and more easily dilated. Gonococcal strictures typically are multiple and several centimeters long. Most of the hard-fibrous scars are present in the most dependent portion of the bulbous urethra. Surgical or radiologic intervention is usually required to alleviate obstructive symptoms secondary to such strictures.
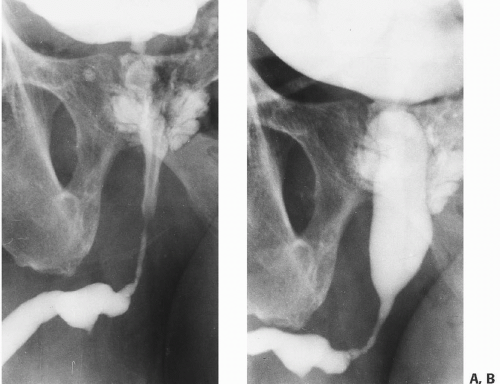
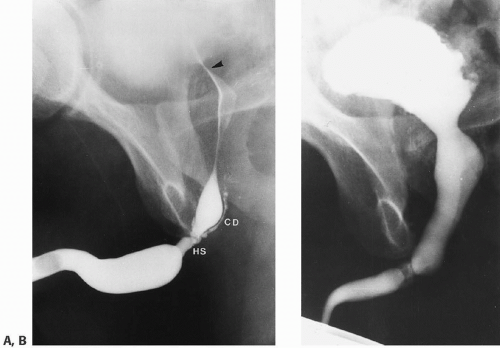
Infection may spread for several centimeters proximal and distal to the hard-fibrous scar, producing further scarring that is not as advanced as the initial site and is consequently softer. The proximal spread of the infection may extend as far as the MU, but the obstructive symptoms, including straining to void, weak stream, and a feeling of incomplete emptying of the bladder, are caused by the hard scarring in the bulbar urethra. This is the primary stricture, and the adjacent softer scars are secondary strictures. The hydrostatic pressure in the urethra during voiding is quite high proximal to hard scarring, resulting in dilation of the urethra proximal to the scar. At least some of this dilation occurs in areas of softer proximal scarring (Fig. 17.3).
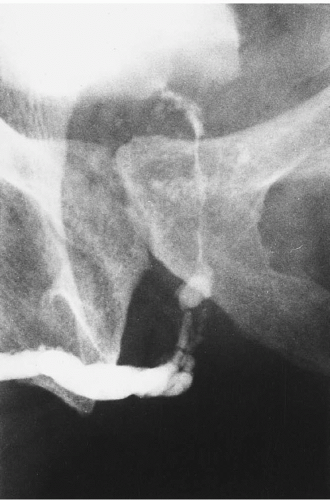
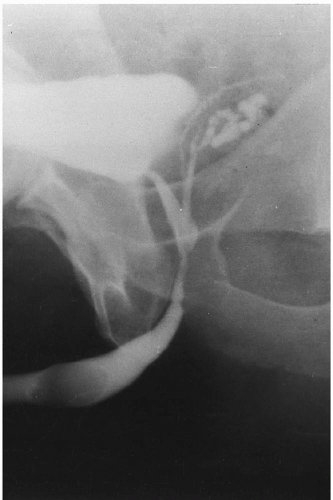
Pseudodiverticulum formation results from a gonococcal periurethral abscess that eventually ruptures into the urethra, leaving a cavity. Most pseudodiverticula affect the inferior aspect of the urethra, but they can occur anteriorly in the region of the penoscrotal junction (Fig. 17.4). Occasionally, a periurethral abscess is large enough to extend to the perineum and penetrate both into the urethra and through the perineum, creating a urethrocutaneous fistula. It is not unusual for multiple fistulae to form. Consequently, urination usually occurs through the perineal fistulae, resulting in the so-called watering can perineum. Whereas this clinical finding can occur as a rare complication of gonorrhea, it is more typical of tuberculosis or schistosomiasis. The abscess cavity resulting in the fistula generally contracts by fibrosis leaving only the narrow fistulous tract from the urethra to the perineum (Fig. 17.5).
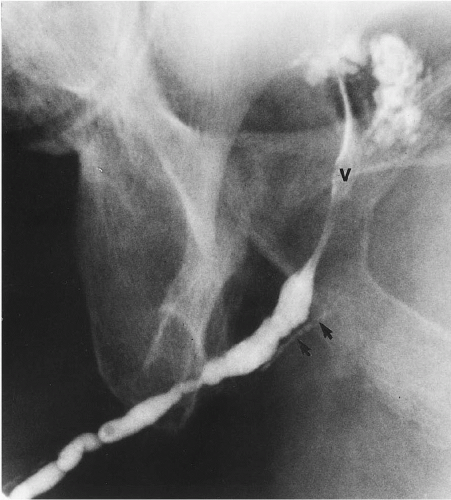
High-intraurethral pressure proximal to a stricture results not only in dilation of the urethra, but also can cause reflux of urine into the prostatic ducts. Ostia for these ducts, 30 to 40 in number, are found in the floor of the prostatic urethra around the verumontanum. This reflux may be massive and may allow infection to enter the prostate, potentially resulting in a prostatic abscess or formation of multiple prostatic calculi (Fig. 17.6). As with other causes of bladder outlet obstruction, the pressure necessary to urinate through a hard stricture may be high enough to result in hypertrophy of the detrusor muscle of the bladder, leading to trabeculation and diverticulum formation. In some cases, vesicoureteral reflux occurs, with eventual dilation of one or both upper urinary tracts. Residual urine in the bladder can result in recurrent infections and stone formation.
Dynamic retrograde urethrography is the most efficacious way of imaging gonococcal strictures and commonly shows several
centimeters of irregular urethral narrowing. The stricture may be smooth or have a beaded appearance (Fig. 17.7). Although the bulbar urethra is the most common area of occurrence, gonorrheal strictures may occur anywhere in the anterior urethra or may even involve the entire anterior urethra. It is not unusual to see small collections of contrast along the dorsum of the urethra in an area of postinflammatory stricturing; these are dilated glands of Littré. If the disease has spread proximally to the MU, the normal cone shape of the proximal bulbous urethra becomes asymmetric and narrowed, giving an elongated appearance to the MU (Fig. 17.8). Abnormality of the normal convex cone shape of the proximal bulbous urethra indicates scarring extending into the MU. This radiologic finding is of prime importance to the urologist, because surgical treatment may involve cutting the scar tissue and consequently the distal sphincter, which can result in iatrogenic incontinence. The verumontanum nearly always can be seen on the dynamic retrograde urethrogram. If the cone of the bulbous urethra is distorted, resulting in loss of the distal landmark for identifying the MU, its location can be inferred to be just below the distal end of the verumontanum.
centimeters of irregular urethral narrowing. The stricture may be smooth or have a beaded appearance (Fig. 17.7). Although the bulbar urethra is the most common area of occurrence, gonorrheal strictures may occur anywhere in the anterior urethra or may even involve the entire anterior urethra. It is not unusual to see small collections of contrast along the dorsum of the urethra in an area of postinflammatory stricturing; these are dilated glands of Littré. If the disease has spread proximally to the MU, the normal cone shape of the proximal bulbous urethra becomes asymmetric and narrowed, giving an elongated appearance to the MU (Fig. 17.8). Abnormality of the normal convex cone shape of the proximal bulbous urethra indicates scarring extending into the MU. This radiologic finding is of prime importance to the urologist, because surgical treatment may involve cutting the scar tissue and consequently the distal sphincter, which can result in iatrogenic incontinence. The verumontanum nearly always can be seen on the dynamic retrograde urethrogram. If the cone of the bulbous urethra is distorted, resulting in loss of the distal landmark for identifying the MU, its location can be inferred to be just below the distal end of the verumontanum.
 FIGURE 17.4. Dynamic retrograde urethrogram in a patient with two diverticula (one large) extending posteroinferiorly from the bulbomembranous urethra. |
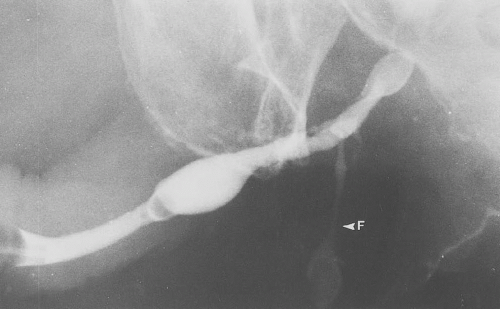 FIGURE 17.5. Dynamic retrograde urethrogram showing irregular scarring in the bulbous urethra with a fistula (arrow) extending from the bulbous urethra to the perineum. |
A voiding cystourethrogram may be useful in defining the proximal extent of a urethral stricture, assuming a catheter can be passed through the stricture to allow filling of the bladder with contrast medium. A 5- or 8-French pediatric feeding tube can be used to pass some strictures. In men with urethral stricture, the bladder capacity may increase to 1,000 mL before the urge to void
is felt. It is wise to instill a further 50 to 100 mL of contrast medium into the bladder after the patient indicates he is ready to void. This usually results in an immediate and good voiding study.
is felt. It is wise to instill a further 50 to 100 mL of contrast medium into the bladder after the patient indicates he is ready to void. This usually results in an immediate and good voiding study.
In the presence of a gonococcal stricture, the voiding study usually shows dilation of the proximal urethra (Fig. 17.9). The dilation may include the MU, even when the dynamic retrograde study indicates scarring extending into the MU. Dilation of a scarred MU indicates softer scarring in the MU than the hard scarring in the bulbous urethra.
The dynamic retrograde and voiding examinations may also indicate other complications of gonococcal urethral stricture. Reflux into prostatic ducts or bulbourethral (Cowper’s) ducts and the development of bladder trabeculation and diverticula are common findings. Reflux into the ejaculatory ducts,
seminal vesicles, and vasa deferentia is uncommon (Fig. 17.10), as is reflux into the prostatic utricle, which may be dilated (Fig. 17.11).
seminal vesicles, and vasa deferentia is uncommon (Fig. 17.10), as is reflux into the prostatic utricle, which may be dilated (Fig. 17.11).
Recent literature has emphasized the use of ultrasound in the assessment of urethral disease. Although ultrasound can give adequate information regarding scarring in the anterior urethra, this procedure is unlikely to indicate bulbous urethral scarring extending into the MU, which is essential for the urologist in the decision regarding operative procedure. Consequently, it appears that dynamic retrograde urethrography is of more value than ultrasound, because the urologist gains more information on the need for a transsphincter urethroplasty. Ultrasound and magnetic resonance imaging (MRI) are used to evaluate the periurethral tissues for abscess formation or for local staging of primary urethral tumors.
Tuberculosis
Usually, genital tuberculosis is a descending infection, and renal tuberculosis is evident. However, in some patients with genital
tuberculosis, the kidneys are normal, indicating the possibility of hematogenous spread directly to the urethra. The prostate is involved in 70% of patients with genital tuberculosis. Prostatic abscesses may rupture into any surrounding structure, resulting in prostatorectal and prostatoperineal fistulae and sinus tracts extending from the posterior urethra. Tuberculous epididymitis and scrotal abscess with fistula formation may also be seen with genital tuberculosis, but fewer than 4% of cases have urethral involvement. When urethral infection occurs, stricturing is followed by periurethral abscesses, producing numerous perineal and scrotal fistulae. The end result is the previously mentioned watering-can perineum.
tuberculosis, the kidneys are normal, indicating the possibility of hematogenous spread directly to the urethra. The prostate is involved in 70% of patients with genital tuberculosis. Prostatic abscesses may rupture into any surrounding structure, resulting in prostatorectal and prostatoperineal fistulae and sinus tracts extending from the posterior urethra. Tuberculous epididymitis and scrotal abscess with fistula formation may also be seen with genital tuberculosis, but fewer than 4% of cases have urethral involvement. When urethral infection occurs, stricturing is followed by periurethral abscesses, producing numerous perineal and scrotal fistulae. The end result is the previously mentioned watering-can perineum.
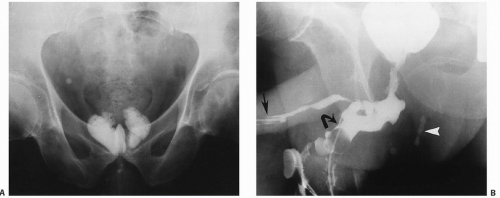
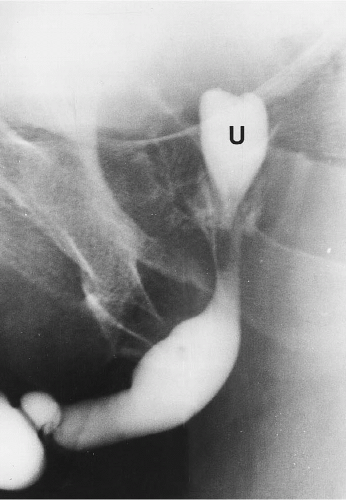 FIGURE 17.11. Dynamic retrograde urethrogram in a patient with multiple anterior urethral strictures. A dilated prostatic utricle (U) is arising from the verumontanum. |
Dynamic retrograde urethrography and voiding cystourethrography typically show an anterior urethral stricture associated with multiple prostatocutaneous and urethrocutaneous fistulae, as well as blind-ending sinus tracts extending from the urethra. It may not be possible to visualize the entire urethra by standard means if most of the contrast medium exits the urethra through the perineal fistulae. It may then be necessary to insert catheters into the perineal fistulae and to inject the fistulae and urethra at the same time to obtain a satisfactory study (Fig. 17.12).
Schistosomiasis
Schistosoma haematobium is the parasite that involves the urinary tract (Chapter 15). Multiple fistulae develop between the urethra and the suprapubic area, the perineum, and the scrotum. Unlike tuberculosis, in which urethral stricture precedes fistula formation, in schistosomiasis, urethral strictures result from fistulous tract formation. These strictures are most common in the bulbous urethra. In patients who have had schistosomal fistulae for more than 4 years, virtually all develop urethral strictures. Radiographic study is the same as described for tuberculous urethral disease.
Iatrogenic Injury
Instrument Strictures in Men
The initial insult to the urethra in iatrogenic stricturing is pressure necrosis resulting from the passage of a straight metallic instrument along an S-shaped urethra that is fixed at two points. These points of relative fixation are the penoscrotal junction, where angulation is caused by the suspensory ligament of the penis, and the MU, which is fixed by the urogenital diaphragm. When a straight, rigid instrument is passed along the urethra, a fulcrum is created at the penoscrotal junction; a second fulcrum is present at the bulbomembranous urethra. If the instrument is of large diameter, is left in the urethra for too long, or is moved in the urethra without appropriate lubrication, pressure necrosis can occur, resulting in tissue necrosis, scar formation, and subsequent stricturing.
IATROGENIC STRICTURES