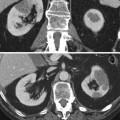
Fig. 1
Renal artery origins from the aorta. Axial contrasted CT with volume-rendering reconstruction shows the anterolateral origin of the right (arrow) and the posterolateral origin of the left renal artery (open arrow)
When the kidney has a typical anatomic configuration, the main renal artery divides into dorsal and ventral rami that run posterior and anterior to the renal pelvis. The anterior and superior aspects of the kidney are supplied by the larger ventral division. The posterior and inferior portions of the kidney are supplied by the smaller dorsal division. In the region of parenchyma where these ventral and dorsal divisions in the renal parenchyma meet, there is a relatively avascular plane (Brodel’s line). This line is the preferred track of placing percutaneous nephrostomies and should be considered when performing biopsies of a native or transplanted kidney.
Segmental renal artery branches arise from the dorsal and ventral rami and course along the infundibula before dividing into interlobar arteries. These interlobar arteries course between the pyramids toward the outer surface of the kidneys. At the pyramidal bases, they then branch into arcuate arteries which course parallel to the bases of the pyramids. Interlobular branches arise from the arcuate arteries and supply the outer cortex of the kidneys.
2.2 Venous Anatomy
The renal hilar venous anatomy courses anterior to the renal arterial anatomy. Accessory renal veins are more common on the right than the left. The left renal vein typically courses anterior to the aorta to the inferior vena cava. Left renal vein variants include the circumaortic and retroaortic renal veins. Knowledge of these venous anomalies can affect surgical planning, IVC filter placement, and renal or adrenal vein sampling. The circumaortic renal vein represents persistence of the posteriorly located left supracardinal vein and a midline supracardinal anastomosis between right and left vessels. This anomaly has been reported in 2–16 % of patients, based on anatomic and angiographic studies. The retroaortic left renal vein occurs somewhat less frequently. Reed et al. reported from a CT series that a single retroaortic renal vein is present in 1.8 % of patients (Reed et al. 1982). Renal vein variants can have clinical importance. In a recent study by Karazincir et al., the incidence of retroaortic left renal vein was found to be significantly higher in patients with varicocele compared with control patients (Karazincir et al. 2007). This may be secondary to extrinsic compression of the venous outflow as it courses posterior to the aorta.
The left renal vein receives drainage from the inferior phrenic, capsular, ureteric, adrenal, and gonadal veins. In the most common variant in patients with a left-sided IVC, the left common iliac vein continues cranially as the left IVC drains into the inferior aspect of the left renal vein and then to the right-sided suprarenal IVC. The right renal vein is shorter than the left and courses obliquely into the IVC. The right renal vein receives capsular and ureteric veins; however, the right inferior phrenic and gonadal veins enter directly into the IVC. Valves may be present within the renal veins with marked variation in the reported incidence.
Renal vein varices may be secondary to renal vein thrombosis or portal hypertension or may be idiopathic. Like varicoceles, renal varices are more common on the left than the right. The “nutcracker” phenomenon results from compression of the left renal vein between the superior mesenteric artery and the aorta and may lead to left renal vein hypertension, hematuria, and varix formation. It is important to remember that a mildly distended left renal vein may be seen in 51–72 % of the normal population by CT, MR, or ultrasound (Buschi et al. 1980). Therefore, measurement of a pressure gradient between the IVC and the left renal vein is needed before renal vein compression should be diagnosed. Color Doppler may provide noninvasive evidence of renal vein compression when collateral veins are demonstrated. In cases of renal vein thrombosis, collateral pathways through the inferior phrenic, adrenal, gonadal, and ureteric veins may develop with left renal vein thrombosis, while only the ureteric vein forms collaterals with the right renal vein.
Venous anomalies may also affect the ureter, such as a circumcaval or retrocaval ureter, which are very rare. A circumcaval ureter occurs more commonly in men than women and is usually an incidental finding. Persistence of the right subcardinal vein traps the ureter behind the IVC. The ureter passes posterior to the IVC and then crosses anteriorly around the medial border of the cava to partially encircle the IVC. On CT, the IVC will have a more lateral location than normally seen, usually lying lateral to the right pedicle of the third lumbar vertebral body, and the course of the opacified ureter can be followed around the IVC.
3 Arterial Disease
3.1 Renovascular Hypertension
The vast majority of hypertensive patients have essential hypertension unrelated to the renal vasculature. Only a small percentage of hypertensive patients have a renovascular etiology. Renovascular hypertension is more common in patients younger than 20 years of age or older than 50 years of age. In contrast, the onset of essential hypertension is usually between 30 and 50 years of age, and there is usually a family history of hypertension. Rapid acceleration or severe hypertension and severe hypertensive retinopathy also suggest a renovascular etiology. An abdominal bruit on clinical exam of a hypertensive patient should likewise suggest a vascular etiology.
Renovascular hypertension is renin mediated and occurs as a physiologic response to renal ischemia. Renin, an enzyme produced in the juxtaglomerular apparatus of the kidney, acts on the circulating serum protein angiotensinogen to produce the inactive hormone angiotensin I, which is converted to the active hormone angiotensin II. Angiotensin II increases blood pressure by stimulating aldosterone secretion from the adrenal cortex and causes arteriolar vasoconstriction. This process exerts antidiuretic and antinatriuretic effects on the proximal renal tubule by promoting sodium reabsorption.
The afferent arteriole, which acts as a baroreceptor, is the most important factor governing renin release. The transmural pressure across this arteriole may decrease as a result of reduced perfusion pressure or increased compliance of the arteriole. The hypertension in patients with renovascular hypertension is dependent on the high circulating levels of angiotensin II. Therefore, an angiotensin II antagonist or the converting enzyme inhibitor, captopril, may be used to control the hypertension.
Even though many different processes may cause stenosis of the main renal artery, the most common etiologies are atherosclerosis and fibromuscular dysplasia (FMD). Less common etiologies include congenital narrowing, arterial hypoplasia, embolic disease, Takayasu’s arteritis, middle aortic syndrome, irradiation, trauma, or an association with neurofibromatosis. Hypertension may rarely be related to parenchymal abnormalities such as pyelonephritis, glomerulopathies, ureteral obstruction, trauma, and renal mass lesions. Reninoma is a renin-secreting tumor of the juxtaglomerular cells which more frequently occurs in patients under 20 years of age and is more common in females (Dunnick et al. 1983).
3.1.1 Atherosclerosis
Approximately two-thirds of cases of significant stenosis of the main renal artery are related to atherosclerosis. Blood pressure does not rise until the degree of stenosis is 60 % or greater relative to the adjacent arterial segment. The stenotic lesion usually occurs at the origin or within the first 2 cm of the renal artery and is usually circumferential but may be eccentric. Bilateral renal artery stenosis is frequently encountered and may be suggested by clinical worsening after administration of ACE-inhibitor therapy. Atherosclerosis is more common in men than women and is accelerated by smoking. Additional risks for atherosclerotic renovascular disease include long-standing hypertension, diabetes, and dyslipidemia. The onset of hypertension secondary to atherosclerosis occurs at a considerably later age than in patients with FMD.
3.2 Renal Artery Stenosis (RAS)
Potential clinical criteria used to select patients who should be imaged to evaluate for RAS include the following:
1.
Age extremes, usually younger than 20 or older than 50 years
2.
Recent onset of hypertension (less than 1 year)
3.
Rapid acceleration of hypertension
4.
Malignant hypertension
5.
Abdominal or flank bruit
Renal Doppler ultrasound offers distinct advantages as the initial screening tool for RAS. These advantages include lack of ionizing radiation, lack of potentially nephrotoxic intravenous contrast, and lack of potential risk of nephrogenic systemic fibrosis (NSF) in patients with renal insufficiency. NSF is a rare debilitating and occasionally fatal skin disorder, which has recently been associated with intravenous gadolinium contrast administration. In patients with significant renal insufficiency, ultrasound now has become the safest imaging modality for detection of RAS (Broome et al. 2007; Thomsen 2006) with a high rating in the ACR Appropriateness Criteria for evaluation of renovascular hypertension (Brown et al. 2013).
Ultrasound imaging of the renal vasculature can be challenging due to the deep location of the renal vessels, overlying bowel gas, and the large body habitus of many patients. Proper training in the performance and interpretation of the ultrasound examination, as well as a strong-quality control program, are critical to good study quality and diagnostic accuracy. In trained hands, the sensitivity and specificity of renal Doppler ultrasound for RAS are up to 95 and 90 %, respectively (Bokhari and Faxon 2004). Renal Doppler ultrasound technique, however, is an operator-dependent imaging modality and not routinely performed at all clinical programs.
The two main methods for RAS detection are direct visualization of the narrowing and indirect evaluation of the downstream effects of the stenosis on the segmental renal arteries. For direct criteria, it is important to visualize the entire main renal artery at ultrasound. Turbulent flow may suggest RAS. Increased velocities at the point of stenosis may appear as Doppler color aliasing, which should prompt further evaluation with spectral Doppler. A peak systolic velocity (PSV) of greater than 200 cm/s has been suggested as the threshold for Doppler diagnosis of 60 % diameter reduction of the renal artery (Fig. 2) (Olin et al. 1995; Pellerito 2002). Another common criterion is a PSV ratio of the renal artery relative to the aorta greater than 3.5. Although studies have validated both criteria, a recent meta-analysis showed PSV as the best predictor of RAS, with sensitivity and specificity of 85 and 92 %, respectively (Williams et al. 2007). Due to a variety of factors, it may not be technically possible to demonstrate the entire length of the main renal artery. This may create an exam that is indeterminate by direct criteria. In these cases, another tool that can be used is evaluation of the intrarenal arterial waveforms (Stavros et al. 1992). Increased segmental artery acceleration time and loss of early systolic peaks in the segmental arteries should raise suspicion for RAS. Spectral Doppler may show a dampened waveform with spectral broadening and blunting of the systolic upstroke—the tardus-parvus waveform morphology (Fig. 3) (Downey 1998; Kliewer et al. 1993). However, it is important to remember that the absence of the tardus-parvus waveform does not exclude RAS. Vessel compliance may be reduced in patients with atherosclerotic disease, making the tardus-parvus waveform morphology less obvious (Demirpolat et al. 2003).
Fig. 2
Renal artery stenosis. (a) Duplex Doppler shows turbulent flow within the right main renal artery with elevated peak velocity 352 cm/s, far above the 2 m/s threshold. (b) Peak aortic velocity is 46 cm/s, yielding a ratio of 7.7. (c) Loss of early systolic peak in the segmental artery waveforms helps support the diagnosis. (d) For comparison, the left renal artery has normal systolic acceleration and early systolic peak (arrow). (e) Coronal MRA confirms high-grade stenosis of the right renal artery (arrow)
Fig. 3
Renal artery stenosis. (a) On duplex Doppler in a 3-year-old with hypertension, there is delayed systolic acceleration with tardus-parvus waveform morphology. (b) On conventional angiography, renal artery stenosis at the bifurcation of the left main renal artery is clearly visible with associated post-stenotic dilatation, likely related to fibromuscular dysplasia
An additional advantage that renal Doppler ultrasound has over other imaging modalities is its ability to predict which patients may benefit from therapeutic intervention of RAS. In a large prospective study, Radermacher et al. showed that patients with elevated RI of greater than 0.80 will not improve after renal artery stenting (Radermacher et al. 2001). A subsequent study, however, showed that 29 % of patients with renal insufficiency and RI of greater than 0.80 showed improved renal function after revascularization and, perhaps more important, 50 % showed improvement in hypertension (Garcia-Criado et al. 2005).
Continued improvement in multi-detector CT technology has had a profound impact on reconstructed three-dimensional (3D) images that aid in the diagnosis of RAS. Accessory renal arteries are well detected with CTA which is an important advantage of CTA, as many of the false-positive and false-negative results are related to accessory arteries. RAS in either the main or an accessory renal artery are now accurately detected with CTA. The sensitivity and specificity of CTA in detecting RAS of 50 % or more are approximately 90 and 97 %, respectively. The sensitivity is even greater when only stenoses of 75 % or greater are considered (Johnson et al. 1999; Urban et al. 2001). In the absence of renal insufficiency, MRA has the highest rating for evaluation of renovascular hypertension by the ACR Appropriateness Criteria (Brown et al. 2013). MRA techniques used to detect RAS, such as time-of-flight, phase-contrast sequences, and steady-state free precession, may be limited by turbulent blood flow and respiratory motion, but significant improvements have been made in MRA diagnosis of RAS without contrast. 3D gadolinium-enhanced MRA avoids these problems by acquiring a complete data set within a single breath-hold. Contrasted MRA has high sensitivity and specificity for RAS and is better than ultrasound for detection of accessory renal arteries and bilateral disease. CTA and MRA both have the additional advantage of increasing diagnostic accuracy by providing multiple different ways to view the data. These options include multiplanar reconstruction, shaded surface display, and maximum intensity projection techniques.
The role of imaging in detection of renal artery stenosis is now frequently directed by the potential benefit of intervention (O’Neill et al. 2011). Recent studies suggest that renal artery stenting is not always justified. In two recent randomized trials, including the ASTRAL study, there was no benefit with regard to blood pressure or renal function as a result of revascularization of atherosclerotic lesions (Bax et al. 2009; Wheatley et al. 2009).
There is now much controversy in the literature due to the ASTRAL trial results. Recent reviews suggest that there may be a group of hypertensive patients with acute-onset or rapidly accelerating hypertension where parenchymal renal damage has not yet advanced to the level of irreversible hypertension. Evaluation of renal perfusion in cases of renal artery stenosis may assist in determining which patients will benefit from intervention. Recent advances in MR perfusion/diffusion and tissue oxygenation also may offer greater accuracy in predicting potential benefit of intervention.
3.2.1 Fibromuscular Dysplasia
Almost 10–20 % of cases of renovascular hypertension are associated with fibromuscular dysplasia (FMD), the second most common cause of renovascular hypertension. However, it can be present in up to 4.4 % of asymptomatic patients in renal donor studies (Plouin et al. 2007). It typically affects women between 30 and 55 years of age. FMD is classified as intimal, medial, or adventitial, as the process may involve any layer of the renal artery.
Medial dysplasia is the most common type of FMD and represents about 90 % of cases. In this process, smooth muscle is replaced by collagen that forms thick ridges. These ridges alternate with areas of small aneurysm formation and result in the classic “string of beads” appearance (Harrison and McCormack 1971; Luscher et al. 1987), which can be seen with conventional arteriography, CTA, or MRA (Fig. 4). This type of FMD is most commonly seen in women 15–50 years of age and usually responds well to percutaneous transluminal angioplasty. FMD can also be seen in cephalic, visceral, and peripheral arteries. FMD may be seen in the carotid and vertebral arteries but tends to spare the intracranial arteries. Contrasted MRA or CTA show good specificities but poor sensitivities for FMD (Vasbinder et al. 2004). However, each performs better than ultrasound for the diagnosis.
Fig. 4
Fibromuscular dysplasia. Contrasted CTA with maximum intensity projection reconstruction in a 41-year-old female shows beaded irregular appearance of the distal main renal artery with classic appearance of medial fibroplasia
Intimal fibroplasia is a process of concentric accumulation of collagen beneath the internal elastic membrane. This creates a smooth stenosis, usually located in the midportion of the renal artery. This process is more common among children and is progressive. Unifocal stenosis is more typical of intimal FMD than medial FMD.
3.2.2 Takayasu’s arteritis
Takayasu’s disease is a granulomatous arteritis that tends to involve the aorta and its major branches. This disease is seen in patients younger than 35 years of age, with a marked female and Asian predominance. Hypertension is a common complication of this disease and may be caused by narrowing of the aorta or main RAS by the arterial inflammation.
3.2.3 Neurofibromatosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree