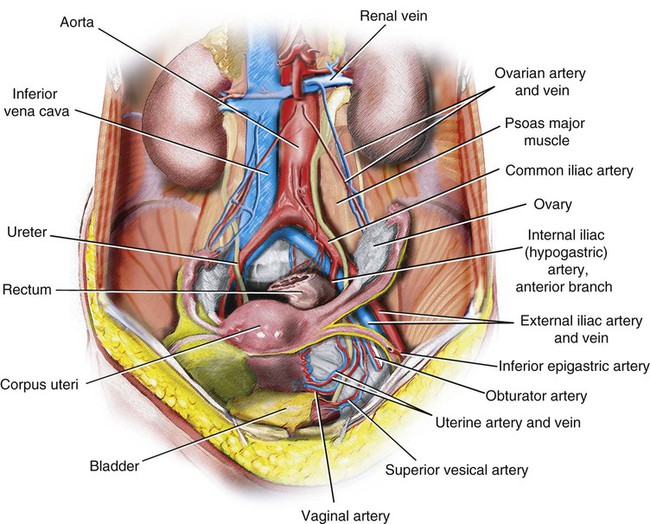
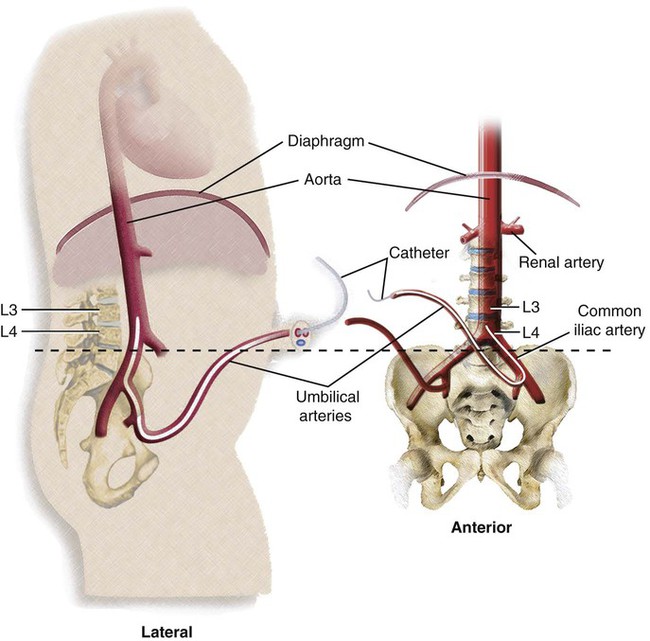
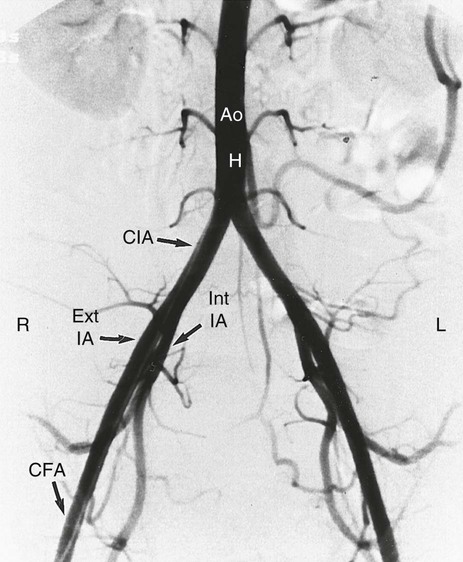
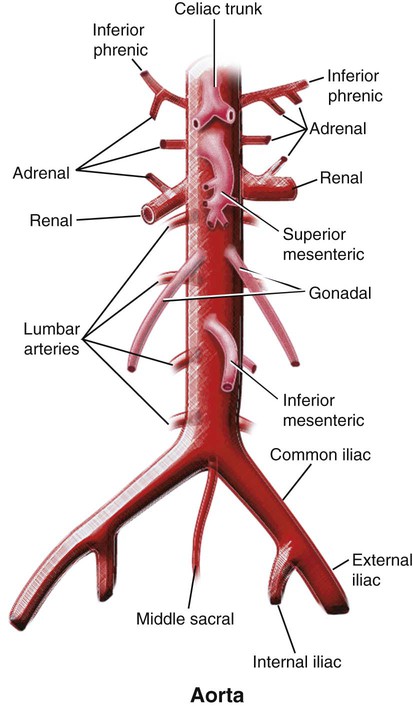
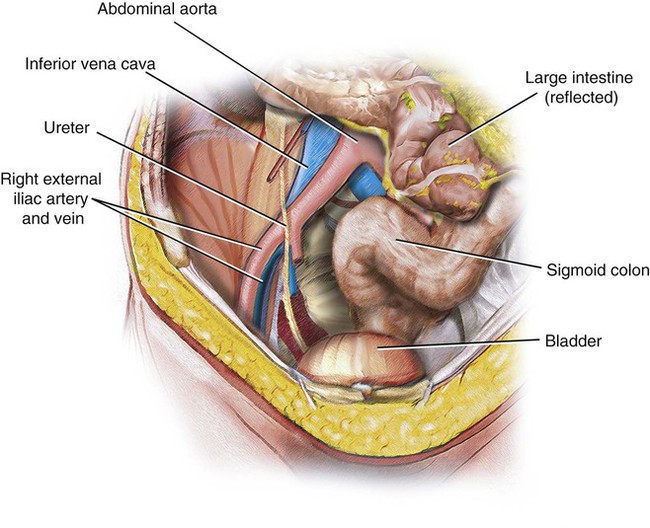
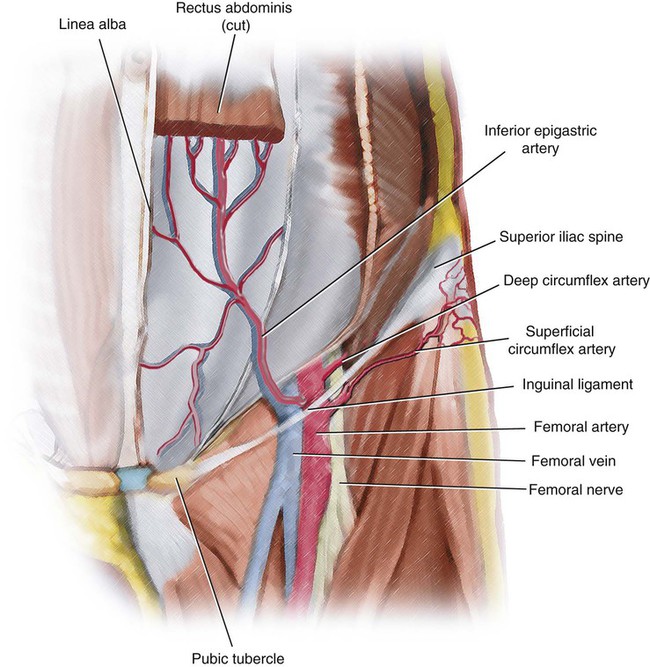
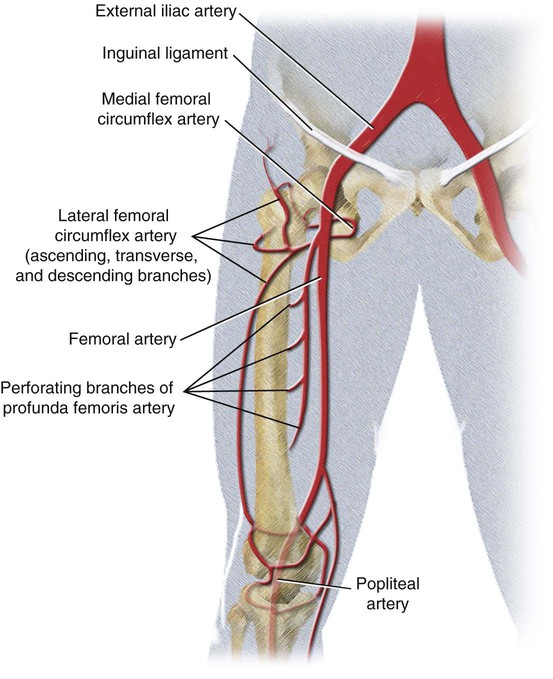
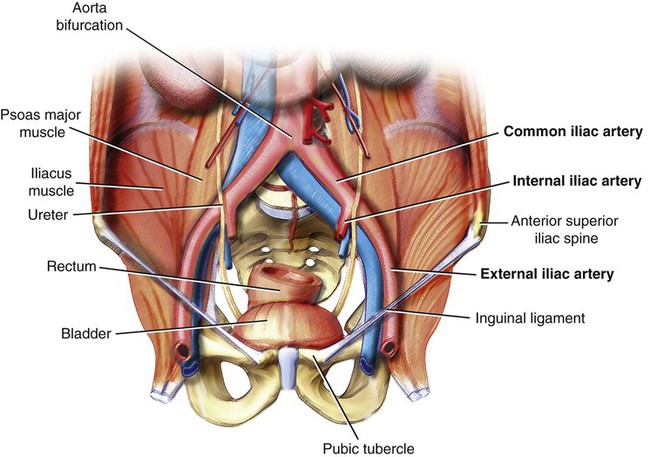
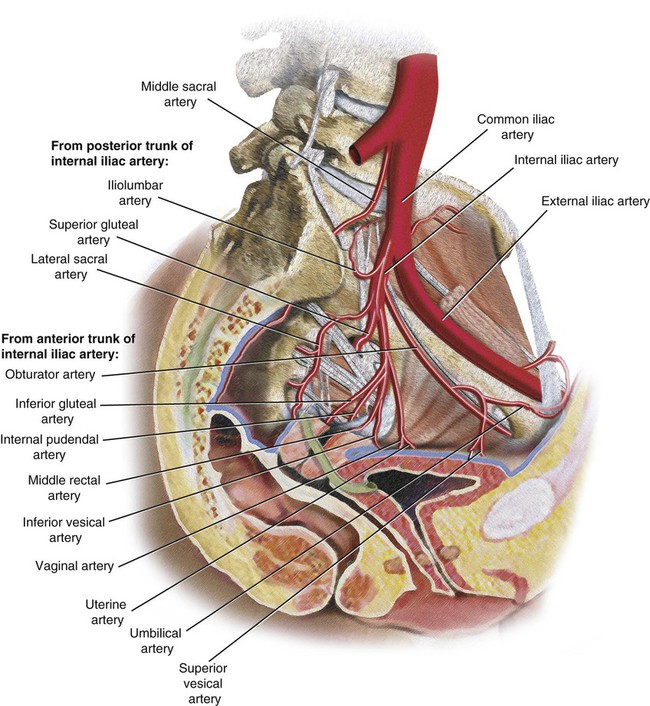
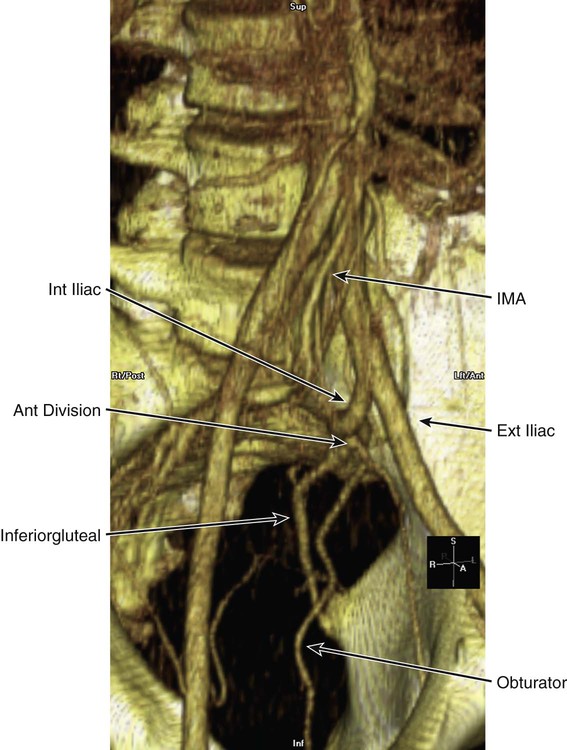
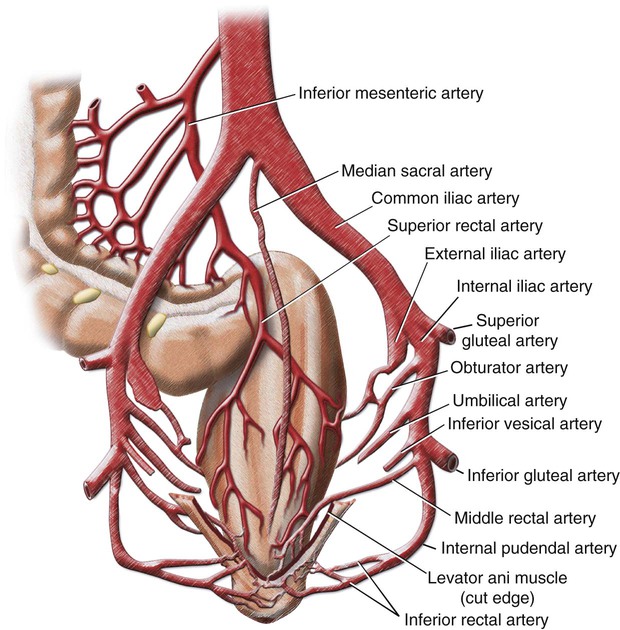
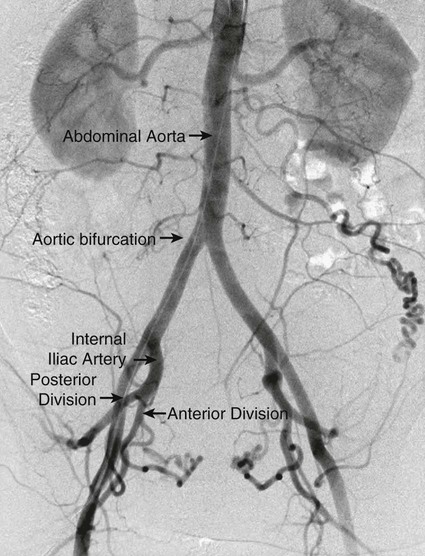
Chapter 75 Elizabeth A. Ignacio, Naomi N. Silva, Nadia J. Khati, Andres Krauthamer, Venkatesh Krishnasamy, Emily J. Timmreck, Emily M. Tanksi and Jordan Ruby The rich vascular supply of the pelvis not only supports the structures contained within it, including the bladder, rectum, and reproductive organs, but also extends to the lower extremities. For a complete understanding of vascular anatomy as it pertains into the endovascular procedures of interventional radiology, it is useful to discuss the vascular structures in sections, from the bifurcation of the aorta and the inferior vena cava to the level of the common femoral arteries and veins. We will also review the anatomy of the iliac vessels, including their branches, common variants, and various collateral pathways (Fig. 75-1). The abdominal aorta terminates at the bifurcation into a right and left common iliac artery. This bifurcation is usually at the lower border of the L4 vertebral body (Fig. 75-2). On physical examination, this site corresponds to a point approximately 2.5 cm below the umbilicus, or at the level of a line drawn between the highest points of the iliac crests. Although the false pelvis (greater pelvis) has its superior border at the S1 level (first sacral vertebral body), it is important to consider the aortic bifurcation in any arterial evaluation of the pelvis (Fig. 75-3). As mentioned, the aorta bifurcates into a right and left common iliac artery. These two arteries pass anterior and slightly to the left of the L5 vertebra and superior sacrum before branching into the right and left external iliac and internal iliac (hypogastric) arteries (Figs. 75-4 and 75-5; also see Fig. 75-3). The external/internal iliac bifurcation occurs above the pelvic inlet of the true pelvis (lesser pelvis). An important pathologic process that can occur at the aortic bifurcation is an associated common iliac vein compression disorder called May-Thurner syndrome or iliac compression syndrome (Fig. 75-6). In brief, this syndrome involves compression of the right common iliac artery on the left common iliac vein against the spine and pelvic brim. This compression may clinically manifest as left lower extremity edema, pain, and/or iliofemoral deep vein thrombosis. The external iliac arteries (right and left) course inferiorly and laterally but remain above the pelvic inlet. The inguinal ligament, found between the two points of the anterior-superior iliac spine (Fig. 75-7) and the pubic tubercle, marks the anatomic boundary of the trunk and lower limb. At this level there are two terminal branches of the external iliac arteries: the inferior epigastric artery and the deep circumflex artery (see Fig. 75-7). These branches provide arterial supply to the inferior abdominal wall. Beyond this point, the external iliac arteries become the common femoral arteries (Fig. 75-8). The internal iliac artery and its branches constitutes the major arterial supply to the pelvic viscera, the wall, and the perineum, including the erectile tissues of the clitoris and penis as well as nerves extending into the gluteal region of the lower limb (Figs. 75-9 to 75-11). The main trunk of the internal iliac artery runs anteromedial to the sacroiliac joint before it divides into the anterior and posterior trunks just above the greater sciatic foramen (Fig 75-12; also see Fig. 75-9). The anterior trunk of the internal iliac artery usually has six major branches, three parietal and three visceral. At this level the branching pattern is subject to many anatomic variations. By the most common order of their origin, these include the umbilical artery, obturator artery (see Fig. 75-10), inferior vesical artery, middle rectal artery (see Fig. 75-10), internal pudendal artery, and inferior gluteal artery (Figs. 75-13 and 75-14). These arterial branches supply the pelvic viscera, perineum, gluteal region, adductor region of the thigh, and in the fetus, the placenta. The uterine artery (see Fig. 75-10) also generally arises from the anterior division of the internal iliac artery, but several variations in its origin have been described in the literature.
Vascular Anatomy of the Pelvis
Arteries
Abdominal Aorta
Aortoiliac Bifurcation
External Iliac Artery
Internal Iliac Artery
Anterior Division
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Vascular Anatomy of the Pelvis