The current classification of vascular anomalies into vascular tumors and vascular malformations and their subtypes has been used by the International Society for the Study of Vascular Anomalies (ISSVA) since 1996 ( Table 51-1 ). This classification is based on the biologic and clinical behavior of these anomalies, including physical characteristics, natural history, and cellular features. Vascular tumors manifest in early infancy. Infantile hemangiomas are the most common type and during growth show increased endothelial cellularity and lumenized capillary-like structures. Vascular malformations are different and are congenital lesions, present at birth and resulting from errors in morphogenesis of vascular channels (capillaries, veins, arteries, and lymphatics) with normal endothelial cell turnover.
| Vascular Tumors | Vascular Malformations |
|---|---|
| Infantile Hemangioma Superficial Deep | Low Flow Single channel Capillary malformation (CM) Venous malformation (VM) Lymphatic malformation (LM) Combined channel Capillary-lymphatic malformation (CLM) Capillary-venous malformation (CVM) Venous-lymphatic malformation (VLM) |
| Congenital Hemangioma Noninvolutionary congenital hemangioma (NICH) Rapid involutionary congenital hemangioma (RICH) | High Flow Arteriovenous malformation (AVM) Arteriovenous fistula (AVF) |
| Kaposiform Hemangioendothelioma (KHE) | Complex Combined (Syndromic Low Flow) Klippel-Trenaunay syndrome Maffucci syndrome Proteus syndrome |
| Tufted Angioma (TA) | Complex Combined (Syndromic High Flow) Parkes Weber syndrome PTEN gene mutation–related |
| Pyogenic Granuloma |
The nomenclature and biologic classification of vascular anomalies are shown in Table 51-1 . This classification is extremely useful because it promotes a clear understanding of these disorders, allows radiologists to establish the correct diagnosis, and enables patients to be managed correctly with appropriate treatments undertaken and inappropriate treatments avoided. This classification, for example, allows radiologists to distinguish between infantile hemangiomas with a significant high-flow component from arteriovenous malformations (AVMs), which are also high-flow lesions without a parenchymal tumor component. A few patients, however, have exceptions to this classification. Some with vascular malformations are not evident until later in life because of either location or progressive expansion.
The interventional radiologist is pivotal to the success of any vascular anomalies program. That patients with these disorders are best treated by a multiprofessional team combining the skills and expertise in medicine, surgery, and radiology needed to diagnose and care effectively for these sometimes complex disorders is well recognized. Having a clear understanding of these conditions and their imaging features, an awareness of treatment options and when best to treat, skills in vascular interventions needed for these procedures, and a knowledge of potential complications and their management allows the interventional radiologist to become a clinical specialist in managing these patients.
Because misdiagnoses are not uncommon in some patients with these disorders, either clinically or on imaging, some patients receive inappropriate treatments. The radiologist is therefore well suited to ensuring the delivery of appropriate care for patients with vascular anomalies.
Imaging
Not all patients with vascular anomalies require imaging to confirm the diagnosis because most (even up to 90%) of these anomalies can be diagnosed from clinical history and physical examination. For example, most babies with infantile hemangiomas do not need imaging, although close clinical follow-up is required. When imaging is undertaken to confirm the diagnosis and or to evaluate the anomaly fully, ultrasound and magnetic resonance imaging (MRI) are the most useful modalities because of their high tissue specificity. For most patients, magnetic resonance angiography (MRA) sequences are not needed to establish the diagnosis. In patients with high-flow lesions, however, MRA is useful for mapping the affected vascular anatomy. Ultrasound has limitations when lesions are extensive or deeply located, but it can be useful in selected patients to provide a rapid bedside diagnosis and to assess potential local complications that can sometimes be seen (e.g., superficial blood clots). Plain radiography and computed tomography (CT) are not required in most patients (these imaging techniques have low tissue specificity). However, they may be required when abnormalities of skeletal growth occur, such as in selected large facial malformations and extremity overgrowth in Klippel-Trenaunay syndrome (KTS).
Conventional venography and catheter angiography are not required in most patients. Venography is occasionally undertaken in KTS to assess anomalous veins and the deep venous system, for which magnetic resonance venography (MRV) may be inadequate. Catheter angiography is done in selected patients with high-flow vascular anomalies when catheter-directed treatments are undertaken. Direct percutaneous puncture venography of venous malformations (VMs) is required only during injection sclerotherapy. Nuclear medicine has no role in imaging of these disorders.
Vascular Tumors
Infantile Hemangiomas
Hemangiomas are the most common tumors of infancy. They occur in the skin approximately 2 weeks after birth and are often found in the head and neck area. Twenty percent of babies have multiple lesions. When these tumors are internal, they can be present in the liver, gastrointestinal (GI) tract, and brain. Infantile hemangiomas have a characteristic three-phase life cycle, with tumors showing progression through three distinct phases. The first phase, the proliferative phase, occurs within the first 12 months of life with rapid tumor growth and tumor angiogenesis. During this phase, tumors are hypervascular, have prominent feeding arteries and veins, show high vascular flow, and can have intralesional vascular shunting. The second phase, the involuting phase, occurs between the ages of 1 and 5 to 7 years and is characterized by slow tumor involution, reduced angiogenesis, and reduction in overall size. During this phase, tumors show reduction in vascular flow and some fibrofatty replacement. Finally, the third phase, the involuted phase, occurs after 5 to 7 years, with resultant fibrofatty residue, small capillaries, and draining veins. After involution, lesions do not recur, and approximately half of all patients have nearly normal looking skin at the site of the lesion.
Clinically, tumors involving the superficial dermis manifest as red, raised lesions ( Fig. 51-1 ). Ulceration and bleeding can be seen in large superficial tumors with rapid growth. Tumors in the lower dermis and subcutaneous tissue appear bluish or cause no alteration in color of the overlying skin. During involution, the color of the tumor fades, and a central pale area may be seen.

Congenital hemangiomas are rare and are distinct from infantile hemangiomas. They occur antenatally, are fully developed at birth, and do not usually exhibit postnatal tumor growth, in contrast to the more common infantile hemangiomas. The two types are the rapidly involuting congenital hemangioma (RICH) and the noninvoluting congenital hemangioma (NICH). Clinically, these lesions are quite different. RICHs are often impressive protuberant masses ( Fig. 51-2 ), whereas a NICH tends to be a flat to slightly raised, rounded skin lesion, with telangiectasias and a pale surrounding halo ( Fig. 51-3 ). RICHs regress spontaneously usually by 12 to 14 months of postnatal life, whereas NICHs persist throughout life. Both are hypervascular tumors. Significant arteriovenous (AV) shunting can occur in the RICH before tumor regression and can potentially lead to cardiac failure. An accurate history and physical examination can establish the diagnosis in 90% of patients.


Infantile hemangiomas can be mistaken for capillary malformations (CMs), and deeper (i.e., subcutaneous) hemangiomas can be mistaken for venous or lymphatic malformations because of the bluish discoloration through the skin. Hemangiomas showing high flow may be mistaken for AVMs, but the age at onset, growth pattern, and presence of tumor parenchyma in hemangiomas distinguishes these two lesions. Congenital hemangiomas can potentially be confused with vascular malformations, although their clinical features provide clues to the diagnosis.
The location of the infantile hemangioma may be associated with specific problems during the proliferative phase when the tumor is rapidly increasing in size. Airway obstruction, visual impairment, GI bleeding, high-output congestive heart failure from vascular shunting within large or multiple hemangiomas, (particularly in the liver), and tissue necrosis can potentially occur.
Hepatic Hemangiomas
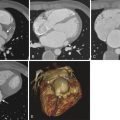
Infantile hepatic hemangiomas (IHHs) have a pattern of involution similar to that of cutaneous hemangiomas. The classic presentation with heart failure, anemia, and hepatomegaly is rare, and certainly not all hepatic hemangiomas are life-threatening. Three predominant IHH forms exist: focal, multifocal, or diffuse ( Fig. 51-4 ). Focal lesions are single, often large, and manifest antenatally. They do not grow after birth and are thought to represent RICH-type lesions, with regression in the first 12 to 14 months of life. Like RICH lesions, macrovascular shunts can result in high-output cardiac failure. Multifocal hepatic hemangiomas are similar to typical cutaneous infantile hemangiomas with similar three-phase life cycles. Small lesions, even if multiple, can be asymptomatic. Some IHHs with macrovascular shunts can lead to cardiac failure. In the diffuse type, most of the liver parenchyma is replaced by tumor, which typically causes massive hepatomegaly, abdominal compartment syndrome, and respiratory compromise. The diffuse type of IHH can lead to severe hypothyroidism until tumor involution occurs because the tumor produces type 3-iodothyronine deiodinase, which inactivates circulating thyroid hormones.

Imaging of Hemangiomas
In infantile hemangiomas, the imaging features depend on the phase of the life cycle of the tumor at the time of imaging ( Fig. 51-5 ). During the proliferative phase, ultrasonography demonstrates a solid parenchymal mass with high vessel density and fast flow. MRI shows a lobulated solid mass of intermediate signal intensity on T1-weighted sequences and hyperintense signal on T2-weighted sequences. Enlarged inflow arteries and draining veins can be seen. Flow voids are present. During the involuting phase, the vascularity is reduced, and the tumor becomes smaller. MRI shows decreased flow voids, and the mass becomes more lobular, with evidence of fatty changes and less parenchymal enhancement.

During imaging, RICH can be confused with AVM because of AV shunting. However, a parenchymal tumor mass present in RICH is not present in AVM (see Fig. 51-2 ). Ultrasound studies of NICHs show subcutaneous hypervascularity in these relatively flat lesions (see Fig. 51-3 ). Because RICHs and NICHs are vascular tumors, the tumor parenchyma on MRI is hypointense on T1-weighted sequences and hyperintense on T2-weighted sequences and shows contrast enhancement. Calcification can be present in congenital hemangiomas. Catheter angiography is done in only a minority of infants with hemangiomas, such as at the same time as embolization, to close shunts to improve cardiac failure as in hepatic hemangiomas ( Fig. 51-6 ), to devascularize challenging lesions in patients with kaposiform hemangioendothelioma ( KHE) and Kasabach-Merritt phenomenon (KMP) if medical therapy is ineffective, and in selected patients preoperatively.

Treatment of Hemangiomas
Most infantile hemangiomas do not require specific treatment other than observation and reassurance to the family. Previously, approximately only 10% of infantile hemangiomas were treated because they were “endangering” by virtue of their location or functional risks (e.g., airway compromise or heart failure). With current treatments readily available, more infants with hemangiomas are treated. Regular follow-up by a dermatologist is essential.
Patients with infantile hemangiomas are treated usually with angiogenesis inhibitors, mainly corticosteroids (oral prednisone), often up until 10 to 12 months of age; the response rate is between 80% and 90%. Intralesional corticosteroid injection can be administered and is indicated for hemangiomas that cause local deformity or ulceration. Ultrasound guidance can sometimes be helpful to target the injection into the solid tumor component. Oral medication with the beta-blocker propranolol is gaining popularity as an alternative or as an adjunctive drug to prednisone. Systemic low-dose, high-frequency vincristine may be considered in challenging cases.
In selected patients, other options such as surgery with excision and debulking can be offered. Surgical resection is considered during the involuting phase in early childhood for large infantile hemangiomas and for NICHs. Laser therapy remains controversial in the treatment of infantile hemangiomas. Flash-lamp pulse dye laser must not be used because most cutaneous hemangiomas are deeper and are not affected by this laser. The neodymium:yttrium-aluminum-garnet (Nd:YAG) laser, however, can be useful for lesions in certain locations. Life-threatening large hemangiomas, especially in the liver with significant vascular shunting, require angiographic embolization (sometimes performed as staged procedures) to manage high-output cardiac failure by closing vascular shunts ( Fig. 51-7 ). These often extremely sick infants require intensive care support throughout this life-threatening period.

Tufted Angioma and Kaposiform Hemangioendothelioma
These sometimes aggressive and invasive vascular tumors are often present at birth, although they can manifest later. KHE is usually more extensive than tufted angioma (TA). The tumors are often located on the trunk, shoulder, thigh, or retroperitoneum. TA appears as a red skin plaque and KHE as violaceous skin lesion ( Fig. 51-8 ).

Tissue biopsy is not always required; however, percutaneous image-guided needle biopsy can be helpful. Histologic examination reveals infiltrating sheets of slender endothelial cells with positive staining for lymphatic elements.
Kasabach-Merritt Phenomenon
KMP is associated with KHE and TA. Typically, profound thrombocytopenia (platelet count usually <10 × 10 9 /L), coagulopathy (with reduced fibrinogen levels and elevated prothrombin and partial thromboplastic times), and bleeding are evident. Treatment is medical because the tumor is large and extensive. Low-dose intravenous vincristine and oral corticosteroids are usually given. In KMP, the mortality rate is between 20% and 30%. These tumors show proliferation into early childhood, with eventual incomplete regression, even though patients are otherwise asymptomatic.
Vascular Malformations
Vascular malformations are classified according to the type of vascular channel affected (capillaries, lymphatics, veins, and arteries) or combinations of such channels. Clinical phenotypes include focal and diffuse forms, and although most of these malformations occur sporadically, inheritance is observed in familial cases. Complex forms can be associated with soft tissue and skeletal abnormalities.
Investigators have proposed that vascular malformations result from genetic mutations leading to dysfunction in the regulation of endothelial proliferation. Mutations in the following causative genes have been identified in patients with inherited phenotypes; the RASA-1 gene (in CM-AVM and Parkes Weber syndrome), the glomulin gene (in glomovenous malformation), and the angiopoietin/ TIE2 receptor gene (in mucocutaneous VMs). Autosomal dominant inheritance patterns have been identified in hereditary hemorrhagic telangiectasia (HHT) and in the PTEN hamartoma tumor syndrome, in which AVMs are seen.
Lymphatic vessels are thought to develop from preexisting veins and express a unique receptor for vascular endothelial growth factor (e.g., VEGF-3). Posterior cervical lymphatic malformations are seen in several sporadic chromosomal syndromes including trisomy 13, 18, and 21, as well as in Turner and Noonan syndromes.
Occasionally, vascular malformations exhibit enlargement and sometimes endothelial hyperplasia, triggered by clotting, ischemia, or partial resection. These features account for their propensity for recurrence after certain treatments.
Capillary Malformations
CMs are commonly called port-wine stains. CM is the most common vascular malformation and is present at birth as a flat, pink-red cutaneous lesion ( Fig. 51-9 ). The skin stains are commonly located as focal lesions in the head and neck area. They can be localized or extensive. On histologic examination, cutaneous CMs have dilated capillary to venule-size vessels located in the dermis that slowly dilate over time, thus resulting in a darker color and nodular appearance. CMs do not fade and are permanent throughout life.

Syndromic CMs occur more rarely, such as in Sturge-Weber syndrome (in which the CM affects the first and second trigeminal dermatomes and is associated with ipsilateral leptomeningeal vascular malformations and cerebral atrophy) and in complex combined vascular malformations such as KTS.
The diagnosis of CM is clinical, and no imaging is required. In patients with syndromic CMs, imaging with MRI is done to evaluate the associated underlying anomalies (e.g., in patients with Sturge-Weber syndrome, MRI reveals intracranial pial vascular enhancement and gyriform calcifications).
Treatment of CMs is for cosmesis, and flash-lamp pulse dye laser therapy is the treatment of choice. Multiple treatments are needed. Up to 70% of patients will show lightening of the skin stain.
Lymphatic Malformations
Lymphatic malformations (LMs) are defined as macrocystic LMs (maximum cyst diameter, >1 cm), microcystic LMs (maximum cyst diameter, <1 cm), or mixed macrocystic and microcystic LMs. This classification better describes these lesions, and older terminology such as cystic hygromas and lymphangiomas should no longer be used because they do not describe the components of the LM.
Clinical Features
LMs often manifest as localized masses, sometimes infiltrative ( Fig. 51-10 ), although they can also manifest with fluid leakage such as chylous fluid in body cavities or weeping from skin vesicles. LMs are usually noted at birth; however, they can be seen at any age, including prenatally on imaging. Although skin and soft tissues are most commonly affected, LMs can involve subcutaneous tissues, muscle (along the fascial planes), bone, and, more rarely, viscera such as the GI tract and lungs. The axilla, thorax, cervicofacial region. mediastinum, retroperitoneum, buttock, and anogenital regions are commonly affected. Soft tissue and skeletal hypertrophy can occur in patients with LMs. Macrocystic LMs appear as soft, compressible masses. Slight blue skin discoloration result from intralesional bleeding. Lymphedema can occur with diffuse infiltration of subcutaneous tissues. Infection and intralesional bleeding can occur in LMs and sometimes lead to alarming expansion of the lesion.

The problems associated with LMs can often be related to their location (e.g., proptosis from periorbital LMs, airway obstruction in cervicofacial LMs, protein-losing enteropathy in GI tract disease). LMs of the extremities can be associated with overgrowth and limb length discrepancy. In Gorham syndrome (soft tissue and skeletal LMs leading to progressive osteolysis), pathologic fractures and vertebral instability can occur.
Imaging
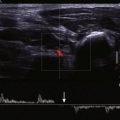
LMs are best characterized by ultrasonography and MRI ( Figs. 51-11 and 51-12 ). MRI better documents the full extent of deeper, larger, and more complex LMs. Cystic components on ultrasound and MRI are easily seen when cysts are larger than 1 cm in diameter. Microcystic LMs have cysts ranging in size up to 1 cm in diameter and often appear as predominantly solid lesions with no identifiable cysts on imaging. On MRI, LMs are hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging (because of high water content). Macrocystic LMs show septal contrast enhancement. Microcystic LMs may show either no contrast enhancement or ill-defined enhancement of the entire lesion. Fluid-fluid levels in cysts result from layering of protein or blood. Enlarged or anomalous venous channels can sometimes be seen in close proximity to LMs. Contrast lymphangiography can identify abnormal lymphatic channels and leaks in those lymphatic anomalies of the thoracic duct and chylous effusions.