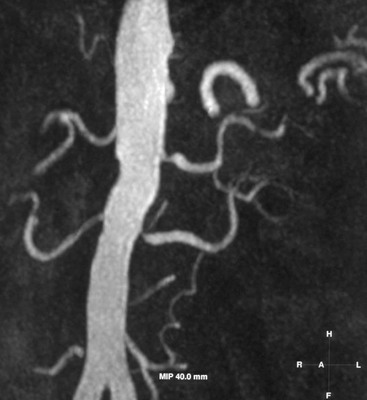
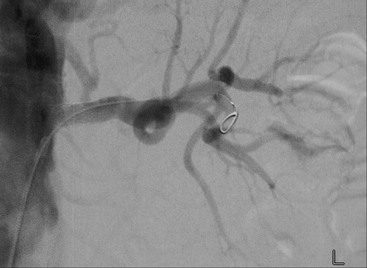
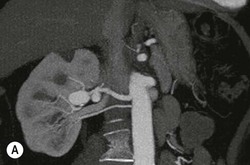
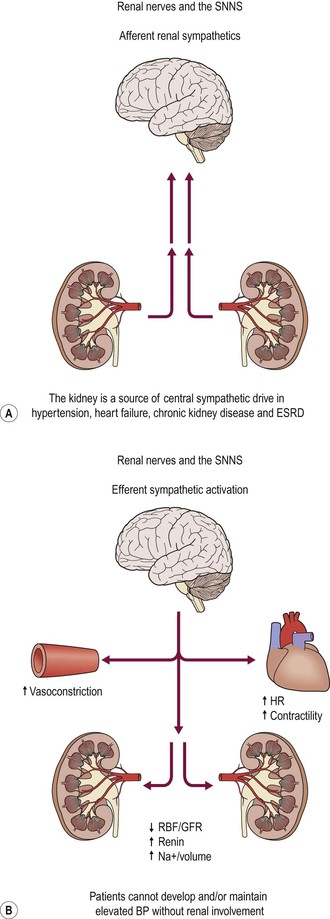
Jonathan G. Moss, Reddi Prasad Yadavali Stenosis of the renal artery (RAS), which is usually focal, can cause a cascade of ischaemic-driven events in the kidney plus other potential insults such as cholesterol embolisation. This can lead to clinical consequences, which include secondary hypertension, impaired renal function and fluid retention (flash pulmonary oedema). Much interest has focused on correcting the anatomical abnormality, initially with angioplasty and latterly with stents in an attempt to reverse or halt the clinical manifestations. In Western populations, atherosclerosis is the leading cause in over 90% of cases. However, in younger age group, the non-atheromatous arteritides should be considered (Table 90-1) particularly in the non-Caucasian individual. Once suspected clinically, the optimal imaging modality is contrast-enhanced magnetic resonance angiography (MRA) (Fig. 90-1). However, due to a small number of reported cases of nephrogenic systemic fibrosis linked to gadolinium contrast media exposure, guidelines suggest caution if the e GFR is <30 mL/min and is contraindicated when <15 mL/min. Other imaging options include computed tomographic angiography (CTA) and newer MRI sequences, avoiding contrast media altogether. Although Doppler ultrasound and functional nuclear medicine scans can be used, they have largely fallen out of favour in recent years. Despite this, they may still play a limited role specific circumstances, however, they similarly selective renal vein sampling is seldom used nowadays. ARVD is by far the commonest cause of RAS and usually develops as part of a systemic inflammatory atheromatous syndrome with disease in other vascular beds (coronary, peripheral). There is a strong correlation with both smoking and type 2 diabetes. Anatomically over 90% of ARVD involves the renal ostium as a result of encroaching aortic plaques. Many patients are asymptomatic and the condition is often detected whilst investigating other symptoms, e.g. lower limb ischaemia. Others present with hypertension, impaired renal function or ‘flash pulmonary oedema’. The latter is a poorly understood condition where there are recurrent attacks of fluid overload with normal or near normal cardiac function but the kidney’s ability to excrete fluid is impaired. Treatment of the global atherosclerotic burden should be addressed with smoking cessation, aspirin, statins and optimising blood pressure control. Although intuitively contraindicated, ACE inhibitors should be given with careful monitoring of renal function. There is some evidence that this ‘package of medical treatment’ can stabilise atheromatous plaque and even induce regression. Revascularisation of the stenotic artery has evolved over the years. Initially performed by open surgical repair, percutaneous transluminal angioplasty (PTA) gained rapid acceptance in the 1980s. However, high restenosis rates due to elastic recoil from the aortic plaques led to disappointing anatomical and clinical results.1 The introduction of metallic stents in the early 1990s led to a resurgence in endovascular activity and the mechanical limitations of renal PTA were overcome with a significant reduction in restenosis.2 Almost overnight renal stenting became the dominant strategy for ARVD. However, although stenting clearly led to improved patency it was often difficult to clearly link this with clinical benefit, e.g. blood pressure reduction or improvement in renal function. It was often said that the ‘rule of thirds’ applied with one-third showing some improvement, another third static and the final third deteriorating. This continuing uncertainty triggered several randomised trials which spanned both the PTA and stenting era. The early trials3–5 pre-dated stents and focussed on blood pressure outcomes. The later trials used stents exclusively and focussed on renal function.6,7 None of these trials with meta-analyses of over 1000 patients have been able to prove any clear benefit of either PTA or stenting over medical treatment alone.8,9 These trials, including the largest (ASTRAL n = 806), have all been criticised and the debate continues. A large ultrasound (US) trial (CORAL) is due to report in 2014 and may provide more information.10 Routine renal stenting for hypertension or impaired renal function is therefore difficult to justify in view of the lack of evidence. However, not all patients entered these trials and possible but unproven indications for renal stenting may include the following: • Intractable hypertension on maximum medical treatment; • Rapidly deteriorating renal function; • A single kidney with a critical stenosis (>90%); Careful individualised patient evaluation is necessary as complications can occur in 5–10% of procedures. These are mostly minor, e.g. groin haematoma, but can include damage to the renal artery, cholesterol embolisation and occasional loss of the kidney. Very rarely a patient will present with acute renal failure and an occluded single renal artery; stenting in these circumstances is worthwhile and can restore renal function with little to lose (Fig. 90-2). The angle from which the renal artery leaves the aorta will help decide between a femoral and an arm (brachial or radial) approach. Over 90% are approachable from the femoral artery. Similarly the angle at which the renal artery ostium lies in the coronal plane will determine the correct angle to place the ‘C-arm’, in order to project the origin of the renal artery clear of the aorta. Careful perusal of the baseline imaging is essential. Advances in guidewire and catheter technology have meant most operators now use the so-called ‘low platform’ systems, which use a 3–4F catheter with 0.014–0.018 guidewires. Delivered through a 6–7F guiding catheter, they are less traumatic than the old 0.035 guidewire systems. Having accessed the renal artery ostium and placed a guide catheter, the lesion is crossed and angioplastied with an appropriate sized balloon. Intraoperative heparin and a proprietary antispasmodic should be given. When dealing with non-atheromatous lesions angioplasty is usually sufficient (Fig. 90-3) but atheromatous lesions are almost always stented to overcome elastic recoil. The procedure is similar to PTA and again uses a ‘low platform’ stent. The lesion is crossed as above and the stenosis pre-dilated to 3 mm and then the stent placed. Accurate C-arm positioning is critical to ensure accurate stent placement with 2–3 mm protruding out into the aorta. Most operators use balloon-expandable rather than self-expanding stents because they are easier to place accurately at the renal artery ostium (Fig. 90-4). In the West, fibromuscular disease accounts for 10% of all cases of RAS. Although it is most frequently found in the renal arteries (60%) other major vessels such as the carotid, viscerals and coronaries can be involved. There are at least five different pathological types but the most common is medial fibroplasia where there are alternating areas of stenosis and aneurysmal dilation leading to the classical ‘string of beads’ appearance (Fig. 90-5). A much rarer type leads predominantly to aneurysm formation (Fig. 90-6) and requires a different management strategy. The typical presentation is a young person, commonly female, with new onset hypertension. Renal function is usually normal and although the lesion may progress, complete vessel occlusion is rare. Although initial management with drugs is usual there is a strong case for angioplasty as the lesions respond well and there is often a good chance of ‘cure’ or significant improvement in blood pressure control.11 The epidemiology of RAS is different in the Indian subcontinent and the Far East, with vasculitis, including Takayasu arteritis, said to be responsible for up to 60% of RAS cases. Although PTA can be used, this inflammatory condition can be resistant to dilation. Steroids are often successfully used to suppress the inflammatory component. This rare congenital condition is known to cause a myriad of symptoms and signs. Less well recognised is the involvement of vessels, commonly the renal arteries. The pathology is usually one of stenosis and aneurysmal dilatation. Although PTA can be utilized, the lesions are often resistant to dilatation and in this young patient group surgical reconstruction of the vessel may be a better option. This rare congenital condition presents in childhood. Although the renal arteries are commonly involved there is almost always aortic hypoplasia and the extent to which angioplasty and stenting can help is very limited. Essential hypertension is extremely common in Western societies where approximately one-third of adults have high blood pressure. With an ageing population, Westernisation and increasing obesity and diabetes, the prevalence of hypertension will only increase. In the USA in 2011, 69% of first heart attacks, 77% of first strokes and 74% with congestive cardiac failure had a blood pressure higher than 140/99 mmHg.12 The costs to the global healthcare system are huge. There is a direct correlation between high blood pressure and cardiovascular risk. Although many patients can be controlled with antihypertensive drugs there is a cohort who do not achieve good control despite multiple medications. This group is estimated to be as high as 30% although in specialist centres, with drug optimisation and having excluded poor compliance and secondary causes, the figure is more likely to be 5%. In this significant minority, until very recently, there was little to offer that was effective. The idea of renal denervation is not a new one. Since the 1920s open radical surgical sympathectomy had been practised mainly for malignant hypertension. Although a very invasive procedure it clearly reduced blood pressure and observation studies of over 2000 patients have been reported.13 Carried out into the 1960s the introduction of modern antihypertensives such as beta-blockers ultimately relegated the procedure to the history books. It was not until the 1990s that interest was renewed with initially rhizotomy in rats and then selective renal denervation using an endovascular approach in pigs. The first reports of successful renal denervation in humans appeared in 2009 with a multicentre ‘proof of principle’ study.14 The kidneys receive an efferent sympathetic supply from preganglionic brain fibres via the thoracic and lumbar sympathetic trunks, which run through the major visceral ganglia before providing postganglionic supply to the kidneys. Efferent stimulation of the kidneys results in activation of the renin–angiotensin–aldosterone system and leads to water and sodium retention and reduced renal blood flow. In addition, the kidneys have an afferent sympathetic output from both mechanoreceptors and chemoreceptors responding to stretch and ischaemia, respectively. Via the dorsal root ganglia these afferent fibres travel to the cardiovascular centres in the brain (Fig. 90-7). Afferent activation leads to antidiuretic hormone and oxytocin secretion and also plays a role in modulation of systemic vascular resistance. Surrogate markers such as noradrenaline spillover and microneurography have demonstrated sympathetic overactivitiy in essential hypertension and this has a myriad of effects described above, all of which ultimately increase blood pressure. Both the afferent and efferent sympathetic fibres run within the adventitia of the renal arteries and this is where they are targeted by the RDN procedure. This technology is evolving rapidly and at the time of writing only one device is CE marked for clinical use. However, at least another six devices are at various stages of development and will be soon arriving on the market. The current device (Medtronic Inc, USA) uses a small steerable radiofrequency probe placed into the lumen of the renal artery through a guiding catheter from a transfemoral approach (Fig. 90-8). Several pulses (5–7) of energy deployed in a spiral fashion are used to heat up and destroy both the afferent and efferent renal sympathetic nerves lying in the adventitial layer. The procedure is repeated in both kidneys. Although performed under local anaesthesia the procedure is relatively painful and an analgesic protocol is required. A regimen similar to that needed for fibroid embolisation is suggested. The procedure is commonly carried out as a day case admission. The precise indications for RDN are not yet fully developed. The reader is directed to the recent guidance issued by the Joint UK Societies Consensus Statement and NICE in 2012.15 Broadly speaking, patients should have a sustained blood pressure of ≥ 160 mmHg (≥ 150 mmHg in type 2 diabetes) on three or more medications. Ambulatory blood pressure measurements should be used. As the procedure is evolving other potentially beneficial effects are being reported. These include reduced insulin resistance, and improved renal and cardiac function. Further research is ongoing in these patient groups. The early results have been very promising and a randomised controlled trial (Symplicity HTN-2) reported in 2010 showed a mean reduction in blood pressure of 32/12 mmHg in the active group compared to 1/0 mmHg in the control group.16 This was a highly significant difference p < 0.0001. There were no serious procedure-related or device-related complications and occurrence of adverse events did not differ between groups. At the time of writing, further trials are underway (Symplicity HTN-3) and longer term follow-up on both safety and efficacy is needed. NICE have produced guidance for the UK, stating the procedure can be undertaken with ‘special arrangements for clinical governance, consent and audit or research’. Intervention for renal tumours is essentially limited to the control of haemorrhage. Preoperative embolisation to facilitate surgical excision although popular in the past is rarely undertaken nowadays with improvements in surgical management. Benign renal tumours are rare. Oncocytomas are often indistinguishable from malignant tumours when small and even differentiation at pathology can be challenging. Bleeding is rare but there are case reports in the literature of embolisation being used. Angiomyolipomas are much more common and present a challenge to the interventional radiologist. Although the majority are isolated there is a well-known link with tuberous sclerosis where they are said to be the commonest cause of death. It is in this syndrome and when lesions are > 4 cm in size that the risk of bleeding increases significantly. Spontaneous bleeding occurs in 50–60% when > 4 cm and up to a third of patients present with shock.17 Embolisation is the procedure of choice and controls bleeding in over 90% (Fig. 90-9). Embolic agents include particles, alcohol and coils, often in combination. Although there is a potential risk of loss of renal function, this is rare or minimal. Re-bleeding is reasonably common but can be treated with repeat embolisation. Complications are uncommon but include aneurysmal rupture. The angiomyogenic component of the tumour is more sensitive to embolisation than the lipomatous elements and it is the former that is thought to bleed.18 This group essentially consists of renal cell carcinoma. Spontaneous haemorrhage is not uncommon and indeed may be the initial presentation often with a history of trivial trauma. Usually hypervascular (85%) these tumours are very amenable to embolisation. Provided the other kidney is normal, embolisation of the entire kidney is the simplest approach. Although placing coils in the main proximal renal artery is tempting and easy, a more distal embolisation should be performed as parasitic supply from other vessels, e.g. lumbar arteries, is common and these in turn may need to be embolised. A careful eye should be kept for connections with other vessels such as colic arteries, particularly if liquid embolic agents are contemplated. The choice of embolic agent includes particulate matter (e.g. polyvinyl alcohol), liquids (e.g. alcohol), histoacryl glue or Onyx. When using alcohol, temporary balloon occlusion of the main renal artery will considerably reduce the peri-procedural pain. Renal arteriovenous malformations are abnormal connections between the intrarenal arteries and veins. They are either congenital or acquired (often iatrogenic). Acquired lesions are often termed A-V fistula and are dealt with in the section ‘Trauma Embolisation’. AVMs are either detected coincidentally or present with haematuria and a renal mass. Patients are commonly hypertensive and occasionally there may be so much shunting that high output cardiac failure ensues (Fig. 90-10A). The more common cirsoid lesion has multiple feeding arteries and draining veins with a definite mass. The less common cavernous type consists of a single artery feeding a dilated chamber draining through a single vein. Embolisation has almost completely replaced surgery for these lesions and the results are good with cure being a realistic expectation. However, embolisation of any AVM is always complex and should only be undertaken by those with adequate experience and training. Referral to a tertiary centre is frequent. Embolisation is almost always from the arterial side and it may be necessary to use temporary occlusion balloons to reduce blood flow to control the embolisation process (Fig. 90-10B). Alcohol, histoacryl glue, Onyx and particles have all been used and each has their advocates.
Vascular Genitourinary Tract Intervention
Kidney
Renal Artery Stenosis
Background
Aetiology and Pathology
Diagnosis of RAS
Atheromatous Renovascular Disease (ARVD)
Clinical Presentation of ARVD.
Treatment of ARVD.
Renal Revascularisation Trials.
Technique for Renal Angioplasty and Stenting
Renal Angioplasty.
Renal Stenting.
Fibromuscular Disease.

Takayasu Arteritis.
Neurofibromatosis.
Williams Syndrome.
Renal Denervation (RDN)
Background
History of Sympathectomy
Pathophysiology
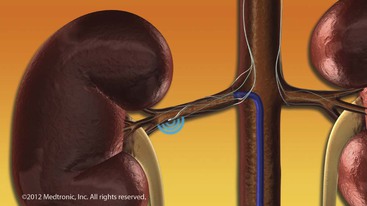
Technique
Indications
Results
Renal Tumours
Benign
Malignant
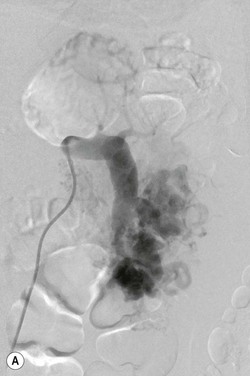
Renal Arteriovenous Malformation (AVM)