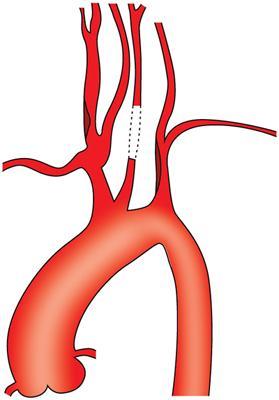
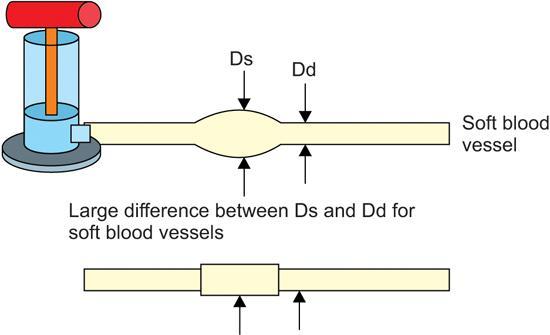
CEREBROVASCULAR DISEASE – UNDERLYING PATHOPHYSIOLOGY Arun Kinare The term cerebrovascular refers to blood flow in the brain. When an area of the brain is temporarily or permanently affected by ischemia or bleeding and one or more of the cerebral blood vessels are involved in the pathological process, it is called as a cerebrovascular disease or cerebrovascular accident. Abnormal hemodynamic involving the extracranial carotid and the vertebral arteries due to atherosclerosis, fibromuscular dysplasia, arterial dissection, arteritis and cystic medial necrosis leading to an aneurysm (rare) could be the underlying pathology. Atherosclerosis heads the list of the underlying pathological conditions. This chapter will deal with pathologies of the carotid and the vertebral arteries in the extracranial location. According to Global Burden of Disease Study 2016, ‘there were 80.1 million (74.1–86.3) prevalent cases of stroke globally in 2016 with 41.1 million (38.0–44.3) prevalent cases in women and 39.0 million (36.1–42.1) prevalent cases in men. Of the total number of prevalent strokes, 84.4% (82.1–86.4) were ischaemic. There were 13.7 million (12.7–14.7) new stroke cases and stroke was the second largest cause of death (5.5 million [95% UI 5.3–5.7] deaths) after ischaemic heart disease’. According to Factsheet: ‘Cardiovascular diseases in India’ by the World Heart Federation, noncommunicable diseases (NCDs), including cardiovascular diseases (CVDs), are estimated to account for 60% of total adult deaths in India. CVDs contribute 26% of these deaths. The risk of CVD deaths in Indian population at early age is more common than in Western countries. In Western population, only 23% of CVD deaths occur before the age of 70 years, whilst in India it is 52%. The main arteries supplying the brain are the internal carotid and the vertebrals. Internal carotids take care of the anterior part, whilst the vertebrals take care of the posterior part. Often an ischemic stroke is the result of the blockage of a carotid artery and a haemorrhagic stroke is due to rupture of an artery in or on the surface of the brain causing bleeding and associated damage to the brain cells, aneurysm and arteriovenous malformations being the frequent underlying causes. External carotids supply the face, neck and skull base. The general pathology of cerebrovascular disease begins with the narrowing of arteries by a process of deposition of cholesterol followed by altered wall morphology, weakening of the walls and narrowing of the lumen. Atherosclerosis, inflammatory, noninflammatory, nonatherosclerotic conditions and trauma are the different conditions leading to cerebrovascular disease or accidents. The details of the same are elaborated in subsequent paragraphs. Stroke is the most frequent end result of these conditions. Fig. 3.40.1.1 describes various types of stroke. Carotid bifurcation is the commonest site for the atheroma formation. Atherosclerosis causes wall thickening and plaque formation in the arteries supplying the brain. These plaques composed of lipids, cholesterol deposits and necrotic cells block the lumen or reduce the diameter of the arteries resulting in ischemia. There can be plaque rupture leading to attraction of platelets and fibrin. This leads to embolus ending in stroke in the distal arterial territories through artery-to-artery embolic mechanism. Plaque ulceration due to the erosion of its surface directly exposes the contents of the plaque to the flowing blood. This is another source of microemboli. Underlying pathological process involves accumulation of inflammatory cells and proteolytic enzymes. Atherosclerosis is an aging process. It begins in the childhood and progresses as the age advances. Structural changes in the form of wall thickening and plaque formation are evident only in the later age groups unless there is a familial factor. Intima media thickness (IMT), morphology of plaque in the carotid arteries and carotid plaque surface characteristics in the form of surface irregularities or ulceration play important role in evaluating structural alterations and development of atherosclerosis to predict arterial damage in other vascular territories. Various studies prove the vital role of carotid IMT and risk for myocardial infarction, stroke, death from coronary artery disease or a combination of these events. Carotid wall stiffness or elasticity studied using various techniques offers valuable information about the functional status of the carotid wall. Stiffness assessment is getting popular as early intervention prior to the stage of structural abnormality yields favourable prognosis. Cervical artery dissection is the most common nonatherosclerotic cause of stroke. Carotid artery dissection is a condition in which the layers of the carotid artery spontaneously separate compromising blood flow to certain areas of the brain leading to a stroke (Fig. 3.40.1.2). This condition occurs when a trauma in the intimal layer of the carotid artery allows blood to flow between the layers of the vessel wall and form a hematoma. Further blood flow in this lumen causes stenosis which may lead to eventual complete vascular occlusion or thrombus formation. This process may lead to a stroke or transient ischemic attack. If the vessel ruptures intracranially, it may lead to a subarachnoid haemorrhage. Also, a pseudoaneurysm (Fig. 3.40.1.2) may result from a carotid dissection. Fibromuscular dysplasia is a condition that causes one or more arteries in the body to have abnormal cell development in the artery wall. Excess deposition of fibrous connective tissue which replaces the media is the most frequent event in the carotids. Progress of the pathology is known to be very slow. This may result in narrowing (stenosis), aneurysms (Fig. 3.40.1.2) or tears (called dissections). A decrease in blood flow through the artery may result in symptoms. Condition is more common in middle age group and women are affected more. However, any age group or sex can get affected. Arteritis refers to the inflammation of blood vessels which subsequently reduce the blood flow to the organs. The two types of arteritis discussed below are Takayasu arteritis and giant cell arteritis (GCA). Takayasu arteritis (Fig. 3.40.1.3) is an inflammation of the larger arteries and can lead to wall thickening, fibrosis, stenosis and thrombus formation. More acute inflammation can lead to an aneurysm. A study of 79 patients with Takayasu arteritis suggests neurovascular manifestations. The common carotid arteries were seen to be affected the most followed by the internal carotid arteries and the intracranial vasculature. Intracranial manifestations of Takayasu arteritis can closely resemble those of primary CNS vasculitis. Stroke of undetermined aetiology as mentioned in the Toast classification is an entity where imaging does not offer any help and the cause may remain a mystery. GCA is an immune-mediated vasculitis of large- and medium-sized vessels affecting aortic arteries in particular superficial temporal artery. It generally affects the elderly persons aged greater than 50 years. Histological features of GCA differ from primary central nervous system vasculitis. The vertebral artery is a common site of extracranial and intracranial involvement. Vertebral Basilar Circulation (VBC) is a common form of stroke affecting 20%–40% patients with stroke. There are two categories of patients with VBC. In the first category, there is an acute basilar artery occlusion and exhibits more rapid onset, whilst in the second category disease progresses with nonspecific symptoms and early warnings of VBC which can be related to ischemic events in the entire posterior circulation vessels. An article by Caplan et al. summarizes the possible pathology of VBC as predicted by different researchers. These pathologies suggest that atherosclerotic disease occurs throughout the vertebral artery. Atheromas can be localized at the vertebral origin, the mid-vertebral artery, the proximal, basilar and the posterior and cerebral arteries. These atheromas in the vertebral can develop a thrombus that can embolize. Since the vertebral arteries are smaller than the carotids, plaques produce more stenosis in the vertebrals than in the carotids and vertebral plaques are less ulcerated than in the carotid arteries. Various studies prove the vital role of carotid IMT and risk for myocardial infarction, stroke, death from coronary artery disease or a combination of these events. Risk factors contributing to increased incidence of cerebrovascular disease can be broadly classified into nonmodifiable risk factors and modifiable risk factors. Nonmodifiable risk factors for stroke include age, sex, race ethnicity and genetics, whereas modifiable include hypertension, diabetes mellitus (DM), atrial fibrillation and atrial cardiomyopathy, dyslipidaemia, sedentary behaviour, diet/nutrition, obesity, metabolic syndrome, alcohol consumption and smoking. Data suggests hypertension to be the most prevalent risk factor for stroke in about 80% of patients. It is known that chronic hypertension worsens atherosclerosis and causes pathological changes in the arteries and arterioles. The structural and morphological changes like microaneurysm formation, lipohyalinosis and microatheroma increase vascular resistance and may predispose cerebral ischemia by weakening vasodilator responsiveness. Apparently, this results in either rupture or occlusion of the diseased vessel causing intracerebral haemorrhage or infarction. The WHO guidelines for the management of hypertension suggest the need for more research to establish the relevance of arterial stiffness (Fig. 3.40.1.4) as independent prognostic factor. In this regard, a study by Kubozono suggests the definite association between arterial stiffness, including carotid-femoral and brachial-ankle pulse wave velocity (PWV) and cardio-ankle vascular index and cardiovascular disease, specifically stroke. The study also highlights the stiffness responses of muscular arteries to be different from those of elastic arteries and that conclusions drawn depend on the region in which the measurement is taken. Another study on carotid arterial stiffness in overweight and obese Indian children concludes that PWV can be considered an important marker for evaluation of early functional changes of the carotid artery in children and adolescents. Thus, identifying children at risk for atherosclerosis at an early age may allow judicious intervention to reduce the atherosclerotic process thereby preventing or delaying the occurrence of cardiovascular disease in adulthood. Patients with DM are at a four times higher risk of stroke. India being the world capital of type 2 diabetes, Indians are more prone to the vascular complications. It is found that patients with diabetes suffer more often from an ischaemic stroke and lacunar infarcts compared to haemorrhagic strokes. The increased oxidative stress in hyperglycaemia leading to inhibition of the action of glyceraldehyde 3-phosphate dehydrogenase (GADPH) which further triggers a series of pathogenic pathways contributing to endothelial dysfunction is one of the prime mechanisms involved in DM associated stroke. Epigenetic changes in nuclear factor-κB (NF-κB) within endothelial cells due to increased reactive oxygen species and subsequent expression of inflammatory genes also suggest a substantial impact on endothelial dysfunction. Study by Giacco et al. (2010) describes how insulin resistance leads to progression of atherosclerotic lesions. A review by Yaghi et al. (2015) gives a detailed insight about the relationship between various lipids in the body and cerebrovascular diseases. The study suggests that there is a very strong direct relationship between cholesterol levels (mainly total cholesterol and low-density lipoprotein), the atherosclerotic disease and ischemic stroke. The high risk of ICH even exists at low cholesterol levels. The risk of small vessel disease exists in spite of low lipid. Imaging plays a crucial role in the evaluation of the cerebrovascular diseases and subsequent sections have covered this topic. Author would like to acknowledge the technical writing services of Dr Arati Ranade in drafting and compiling of this manuscript. ANATOMY OF CAROTID AND VERTEBRAL ARTERY AND COLLATERAL PATHWAYS S. Shivram The colour Duplex examination of Carotid circulation includes examination of both carotid and vertebral arterial pathways. The principle arteries of head and neck are the two common carotid arteries on each side of the neck. The left common carotid artery arises from the highest point of aortic arch and has a thoracic and a cervical portion. Its origin cannot be seen by ultrasound scanning of neck. The right common carotid artery begins at the bifurcation of the innominate artery behind the right sterno-clavicular joint and is confined to neck. Its origin can be seen by ultrasound examination of neck (Fig. 3.40.2.1A). The common carotid arteries ascend on each side in a cleft bordered by the cervical vertebrae along with its muscular attachments posteriorly, by the sterno-cleidomastoid anterolaterally and by the trachea, larynx and oesophagus medially. The common carotid artery bifurcates at the upper border of thyroid cartilage at the C4 vertebra into the external and internal carotid arteries (Fig. 3.40.2.2). The ICA is generally the larger and postero-lateral to the ECA which is relatively the smaller and medial in position. Occasionally the CCA may be tortuous in course. The average diameter of common carotid artery is approx. 6.5 mms in males and 6.1 mms in females (Fig. 3.40.2.3). Anatomical Variations of common carotid artery: The common carotid bifurcates into the external and internal carotid arteries at the level of upper border of thyroid cartilage (the bifurcation level is although variable). From its origin, it takes a slightly curved course upwards. The ECA branches just above the bifurcation and gives the superior thyroid, ascending pharyngeal and lingual arteries below or around the level of angle of mandible. At the level of neck of mandible, it inclines backwards where it passes into the substance of parotid gland dividing into the superficial temporal and internal maxillary arteries (Fig. 3.40.2.5). The external carotid artery is relatively easier of the two branches of common carotid to identify by ultrasound. At its origin, the ECA lies anterior and medial to the ICA and adjacent to the internal jugular vein, whereas higher up it is situated lateral to the internal carotid artery. In adults, its luminal diameter is slightly less than that of the internal carotid artery and ranges between 4.2 and 5.3 mms being more in males than females (Fig. 3.40.2.6). Begins at the bifurcation of the common carotid artery where it usually presents a localized dilatation known as the carotid sinus or carotid bulb. The extra- and intracranial course of the internal carotid artery has four segments: The Standard Doppler examination of Carotid-Vertebral system includes only the cervical segment of internal carotid artery. The ICA ascends to the base of skull and enters the cranial cavity through the carotid canal of temporal bone. It is relatively superficial at its commencement in the carotid triangle, but after passing deep to the posterior belly of digastric muscle, it lies in a deeper plane. The internal jugular vein and vagus nerve lie lateral to it. The external carotid artery at first lies anterior and medial to the internal carotid artery, but after leaving the carotid triangle lies superficial to it. It is always the more posterior of the two branches and does not have any visible branches in neck. If there are no early branches from ECA, it may be difficult to differentiate it from ICA. Also if the carotid bifurcation is very high, the two arteries may not be seen on ultrasound. The variations (Fig. 3.40.2.7) result mainly because of elongation of the ICA due to either of the following: The vertebral arteries originate (V0 segment) as the first branch of subclavian arteries. In a relatively small percentage of population (approx. 6%), the left vertebral artery arises directly from the aortic arch. The vertebral arteries ascend posterior to the internal carotid artery and have a variable diameter ranging from 3 to 5 mms. Its course is divided into four segments (Fig. 3.40.2.8): Atherosclerosis affecting the carotid arteries has been related to stroke, cognitive impairment and dementia. The presence of good collateral circulation significantly modifies the risk of stroke. A good collateral circulation is a favourable prognostic factor and its absence is considered an unfavourable prognostic indicator both in acute and chronic settings for patients with symptomatic carotid artery disease. The clinical manifestations are also resultantly varied ranging from incidental detection of occluded carotid artery to devastating stroke with complete infarction. Blood pressure is the main driving force that leads to formation of collateral circulation. When a main artery from aortic arch is occluded, the blood pressure in the distal segment can be much lower than adjacent arteries. As a result, blood flow in adjacent arteries may be drawn reversely to the distal segment. This phenomenon is called ‘steal’, with subclavian steal syndrome as an example. When CCA is occluded, the blood pressure in ipsilateral ICA can be obviously lower than ipsilateral ECA. As a result, ICA ‘steals’ blood from ECA – Carotid/ICA steal. A study by Wang et al. describes four collateral circulation pathways of ‘ICA steal’ by DSA and CTA, as shown in the schematic diagram (Fig. 3.40.2.9). The circulation is maintained by flow from the following (Fig. 3.40.2.10): NORMAL CAROTID AND VERTEBRAL DOPPLER SONOGRAPHY Aman Gupta The main indication of ultrasound examination of the extracranial carotid and vertebral arteries is the detection and characterization of atherosclerotic disease and stenosis; however, as per recent published practice parameters for the performance of an ultrasound examination of the extracranial cerebrovascular system of American Institute of Ultrasound in Medicine, in association with the American College of Radiology, the Society for Paediatric Radiology and the Society of Radiologists in Ultrasound, indications for an ultrasound examination of the extracranial carotid and vertebral arteries include evaluation of patients with the following: Triplex Doppler, a combination of the B-mode imaging, colour Doppler and spectral analysis, is now an established noninvasive diagnostic technique for effective and accurate assessment of extracranial carotid and vertebral arteries. Anatomy and characteristics of the carotid and vertebral arteries are recorded first with grey-scale imaging using B-mode; colour Doppler imaging is then used to discover the regions of abnormal blood flow followed by Doppler spectral analysis for quantification of flow characteristics. For ultrasonographic assessment of extracranial carotid and vertebral arteries, one of the two approaches is used for the relative position between the patient and the examiner. The first is overhead position, wherein the examiner sits towards the end of the examination table, beyond the patient’s head (Fig. 3.40.3.1A). The advantages of this position are that an easy access can be obtained to the neck. Second and more commonly practiced position is the usual lateral sitting position (Fig. 3.40.3.1B). The patient is made to lie supine on the couch with the head resting on a pillow. The neck is exposed, slightly hyperextended and the head rotated 45 degrees away from the side being examined. In some patients, slight elevation of shoulders may help. In emergency and I.C.U. settings, if the patient has difficulty in breathing, it may be necessary to scan the patient in semisupine or more upright position. High-frequency linear transducers are used for carotid sonography and higher frequencies (>7 MHz) are ideal for the assessment of the intima-media thickness and plaque morphology, whereas for Doppler assessment, lower frequencies (<7 MHz) are preferred. As per practice parameters of AIUM, the examination of the extracranial cerebrovascular systems should use the highest clinically appropriate frequency, realizing that there is a trade-off between resolution and beam penetration. Almost all modern ultrasound systems have examination presets available that are suitable for the majority of carotid examinations, but it may be necessary to optimize machine parameters depending on patient body habitus, course of vessels and to enable the detection of low-velocity flow when differentiating carotid artery occlusion from a subtotal occlusion. Grey-scale imaging, both in longitudinal and transverse planes, of the common carotid artery (CCA), its bifurcation, the internal carotid artery (ICA) and external carotid artery (ECA) should be performed first. Three probe positions are used in longitudinal plane (Fig. 3.40.3.2): In transverse plane, proximal carotid is scanned from anterior/lateral position, whereas distal carotid and bifurcation is scanned from lateral/posterior position. Grey-scale scanning is usually started at the base of the neck, in transverse plane. Origins of CCA, subclavian and vertebral arteries are first visualized. Transducer with small foot print may be used. The CCA is then scanned along its whole length up to the bifurcation, and along the ICA and ECA as high up the neck as can be seen. This allows to ascertain the level and orientation of the carotid bifurcation. The CCA is now imaged in longitudinal section, beginning at the base of the neck. In order to adequately visualize the carotid arteries, and its bifurcation, a range of longitudinal scan planes should be used. In relatively few cases only, the bifurcation, ECA and ICA appear in the same plane; in majority, the ECA and ICA will not be seen in the same plane and need to be imaged individually using small oblique probe movements. Scanning technique need to be modified depending on patient body habitus and tortuosity of vessels with all scanning planes being utilized. Complete assessment of the accessible portions of common carotid artery, its bifurcation and both the internal and external carotid arteries should be performed using grey-scale both in longitudinal and transverse planes. Caudad angulation of the transducer in the supraclavicular area and cephalad angulation at the level of the mandible may aid analysis. Whilst scanning in longitudinal, transverse or oblique planes, medial to lateral motion of transducer is done to optimally image all vessel walls. Gain should be optimized to detect the vessel wall, plaque and other abnormalities. Grayscale images must be obtained at least at the following levels: (Fig. 3.40.3.3) In cases where abnormalities are detected, the following additional images must be taken: On grey-scale imaging, a normal carotid vessel has smooth regular walls with lumen devoid of any internal echoes. The optimal grey-scale image of the carotid artery wall shows two bright interfaces, the inner bright line is the interface between the blood and intima and the outer bright line is the interface between the media layer and adventitia layer. The distance between the two bright lines represents the intima-medial thickness (Fig. 3.40.3.4A). Intima-medial thickness (IMT) is measured on a two-dimensional grey-scale image using electronic callipers. Nowadays, many vendors provide an automated tool for measuring the IMT (Fig. 3.40.3.4B). IMT should be measured preferably on the far wall of the CCA within 1 cm proximal to the carotid bulb. IMT of the CCA has better reproducibility than ICA or carotid bifurcation due to its proximity and relative parallel course to the skin surface. The IMT should be measured on a segment without any focal lesion with carotid artery parallel to the probe surface to minimize the overestimation of the IMT from the diagonal measurement. The six values of IMT (three on each side) are obtained and averaged to get mean IMT. Carotid artery atherosclerosis as measured by carotid intimal medial thickness is an independent risk factor for stroke and myocardial infarction. An IMT of >1 mm is usually considered abnormal although there are authors who propose an IMT value of >0.8 mm as abnormal. Colour flow imaging: Having located the three vessels and observed any evidence of disease in the B-mode image, colour flow is then switched ‘on’. Colour Doppler displays the flow information in real time over the entire patent vascular lumen in the sampled area. The main advantages of colour flow imaging are easy identification and tracking of the vessels, fast recognition of flow abnormalities associated with stenosis, areas of filling defects due to the presence of atheroma and the absence of flow due to occlusion. Colour flow imaging greatly aids in selecting areas that require close investigation with the spectral Doppler. Overall colour Doppler improves confidence in diagnosis, shortens examination time and improves the reproducibility of spectral Doppler results. Colour flow imaging parameters must be optimized so as demonstrate wall-to-wall filling of the normal vessel lumen and/or flow disturbances associated with stenosis. Low velocity scale settings will result in aliasing, whereas high gain settings may result in artefacts with bleeding of colour into the walls (Fig. 3.40.3.5). Colour Doppler images must be obtained at least at the following levels:
3.40: Vascular imaging of head & neck
Introduction
Prevalence
Blood flow to the brain
Pathophysiology of CVD
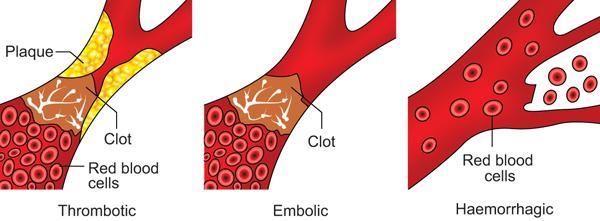
Atherosclerosis
Screening for atherosclerosis
Carotid artery dissection
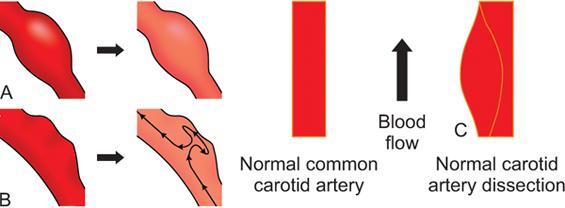
Fibromuscular dysplasia
Arteritis
Vertebral basilar circulation
Risk factors of CVD
Modifiable risk factors
Hypertension and arterial stiffness
Diabetes mellitus
Dyslipidaemia
Acknowledgements
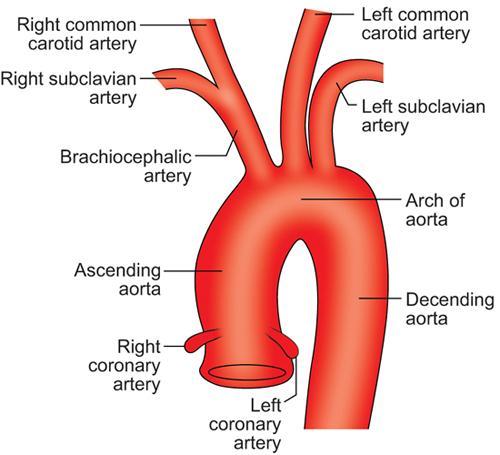
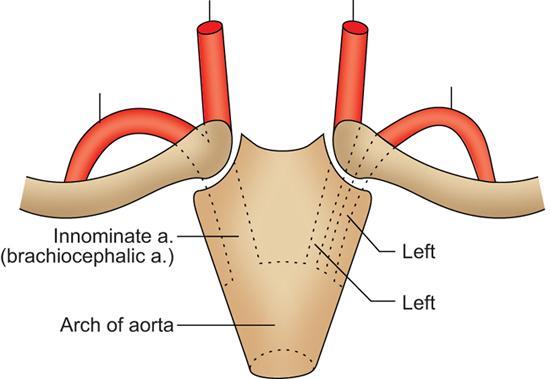
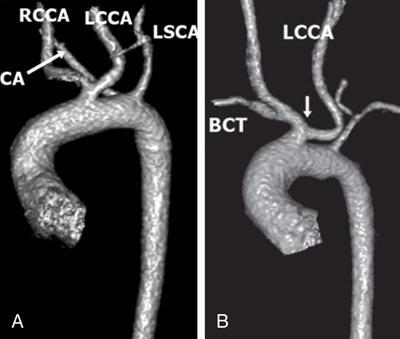
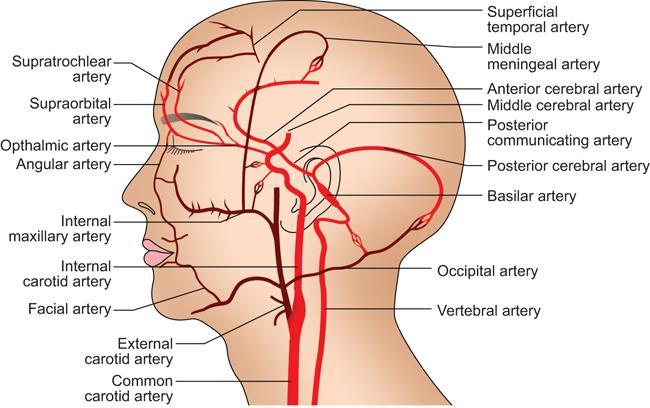
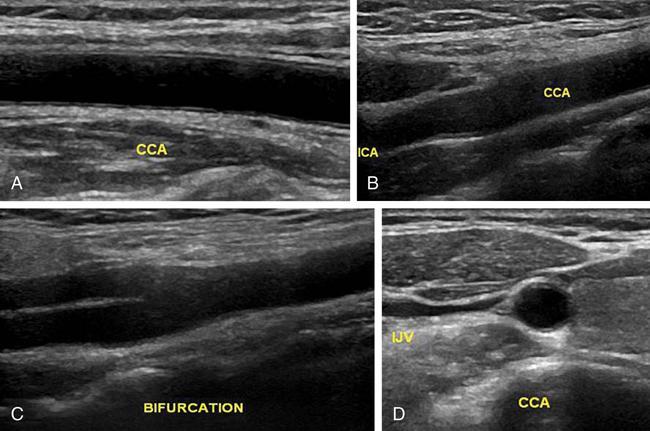
Common carotid artery
Anatomy and course
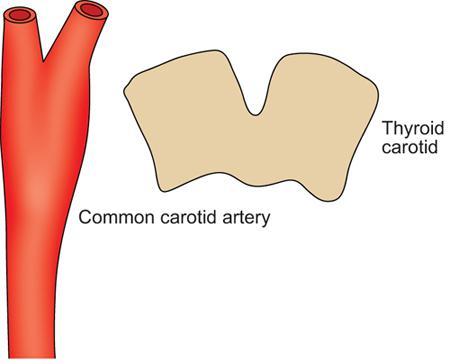
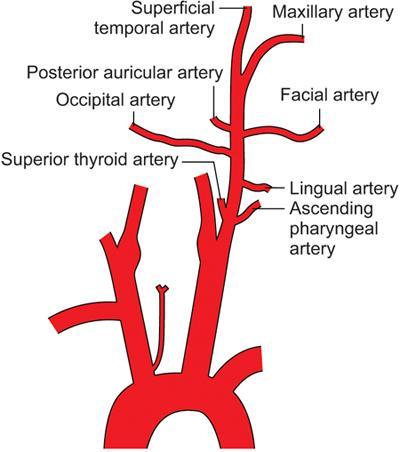
External carotid artery
Anatomy and course
Internal carotid artery
Anatomy and course
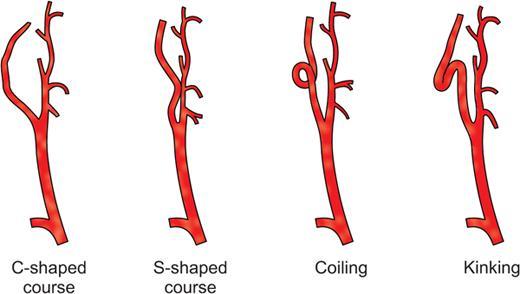
Anatomical variations of internal carotid artery
Vertebral artery
Anatomy and course
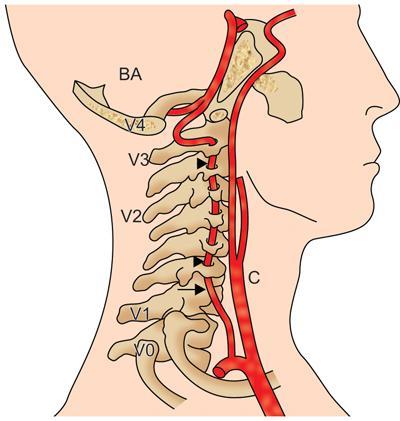
Anatomical variations of vertebral artery
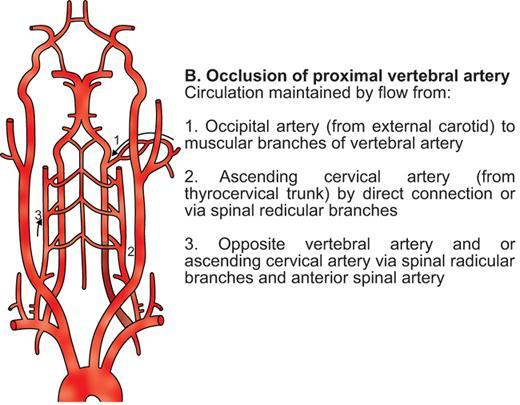
Collateral pathways
Carotid occlusion
Occlusion of proximal vertebral artery
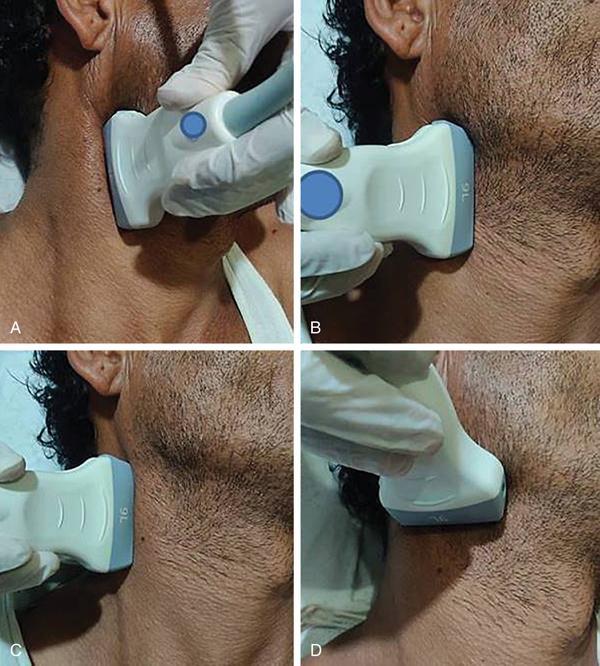
Examination protocol
Patient positioning

Transducer
Presets
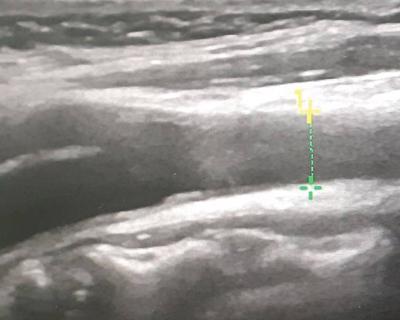
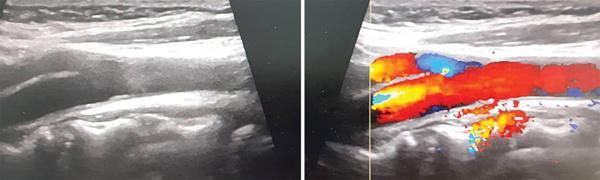
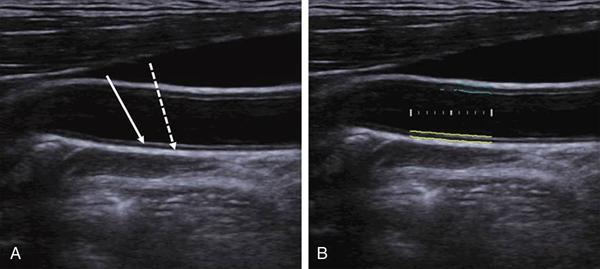
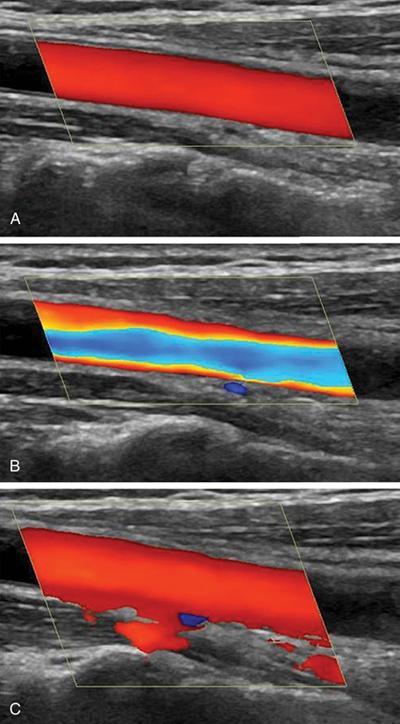
Scanning technique
Ultrasound assessment of the carotid arteries
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







