Chapter 33 Vascular imaging of the head and neck
Common indications for vascular examination
Cerebral aneurysm
This is the most common indication for cerebral angiography. Aneurysmal rupture occurs in 6–12 per 100 000 population and the presence of asymptomatic aneurysms is thought to be in the region of 2% of the population.1 A ruptured aneurysm presents the commonest cause of subarachnoid haemorrhage (SAH) in adults. The most common type is the saccular or berry aneurysm. Typically, defects develop due to the pressure of systolic waves causing herniation of the vessel wall.2
The average age of presentation is 40 years. Below this age presentation is more common in men than in women, but this reverses from 40 years upwards.1 Over 90% of saccular aneurysms occur in the anterior circulation at branch points in the carotid supply,3,4 the remaining 10% being in the posterior circulation.1 In the anterior circulation approximately 25% are located in the middle cerebral artery distribution, 35% around the anterior cerebral artery and 30% associated with the internal carotid artery.1,4,5 Cerebral aneurysms can range from 1–2 mm to 1–2 cm,5 with the risk of bleeding generally increasing with size.1,4,6
The clinical presentation of rupture leading to SAH includes:
Arteriovenous malformation (AVM)
AVMs are the second most common cause of SAH in adults. They result from developmental abnormalities of arterial and venous vessels leading to the formation of fragile vascular walls2 as well as the lack of development of a capillary bed.1 Typically they are made up of three parts: a core of dysplastic vessels known as a nidus, arterial feeding vessels and draining veins.10 The associated vessels are hypertrophic and hyperplastic. AVMs are typically 3–4 cm in diameter2 and are usually symptomatic by the age of 40 years.1
Points of note
• A SAH occurs when blood escapes into the subarachnoid space, which is the space between the arachnoid and the pia mater. In this space it mixes with the cerebrospinal fluid
• A subdural haemorrhage is the presence of blood between the dura and the arachnoid mater
• An extradural haemorrhage is a bleed outside the dura mater, between the dura mater and the bony skull
• SAH may arise from a ruptured intracranial aneurysm, a bleeding AVM, or infrequently as a result of trauma. In contrast, subdural and extradural haemorrhages usually occur as a result of trauma
Stroke
The World Health Organization has estimated that, worldwide, there were 5.7 million deaths from stroke in 2005, equivalent to 9.9% of all deaths.11 A first or recurrent stroke is experienced by 110 000 people in England each year,12 and stroke accounts for 11% of all deaths in England and Wales.13 In England there are more than 900 000 people living with the effects of stroke.13
Stroke may be divided into two main categories:
Ischaemic stroke
Haemodynamic ischaemic stroke occurs following:
• a reduction in perfusion for any reason
• dissection of the vessels in the neck particularly following trauma.
Lacunar infarcts occur as a result of occlusion of small penetrating arteries, usually around 1–15 mm in size, in subcortical areas or in the brainstem.15
Imaging methods
Digital subtraction angiography (DSA)
Technique
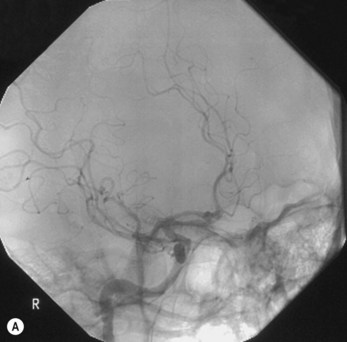
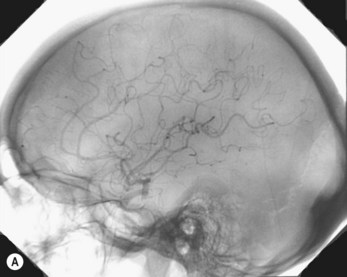
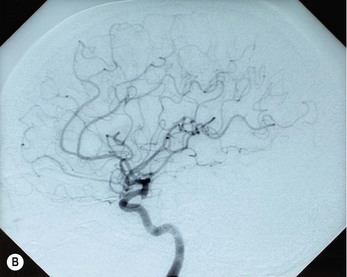
Internal carotid artery (Figs 33.1A,B, 33.2A,B, 33.3A,B)
Typical standard projections are shown in the following table.
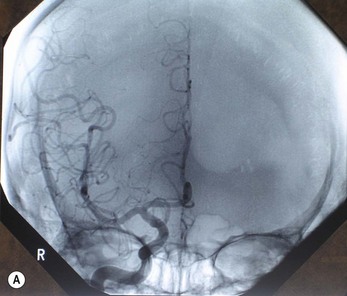

Figure 33.1 OF projection following injection into the right internal carotid artery: (A) unsubtracted; (B) subtracted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree