3 | Vascular Supply of the Uteroplacentofetal Unit and Techniques for the Examination of Individual Vessels |
Vascular Supply of the Uteroplacentofetal Unit
Uteroplacental Blood Supply
The uteroplacental blood supply is shown schematically in Figure 3.1. The specific arteries supplying the uterus are the uterine aa. and the ovarian aa., which anastomose around the uterus. The blood supply of the uterus from the internal iliac aa. (uterine aa., Fig. 3.2) and directly from the aorta (ovarian aa.) is therefore secure. There are also other possible supply paths, for example, from the external iliac aa. via the round ligaments or more caudally from the internal iliac aa. via the cervical aa. or the vaginal aa.
The uteroplacental vessels in a narrower sense lie in the wall of the uterus. The arcuate aa. are tortuous, forming arcades that anastomose freely, and give rise to radial aa. that pierce the myometrium radially. They give rise to basal aa., which supply the stratum basale, as well as two or more helically wound spiral aa. that open directly into the intervillous space of the placenta (Fig. 3.3).
The musculoelastic layer in the arterial wall of the decidual spiral aa. is destroyed by migrating tropho-blastic tissue, enlarging the lumen at the placental end considerably and preventing its narrowing by any vasomotor stimuli. The uteroplacental blood supply is controlled by regulation of the uteroplacental aa. There are some indications that this regulation is initiated by humoral factors of fetoplacental origin, such as estrogen, even before the trophoblastic invasion.
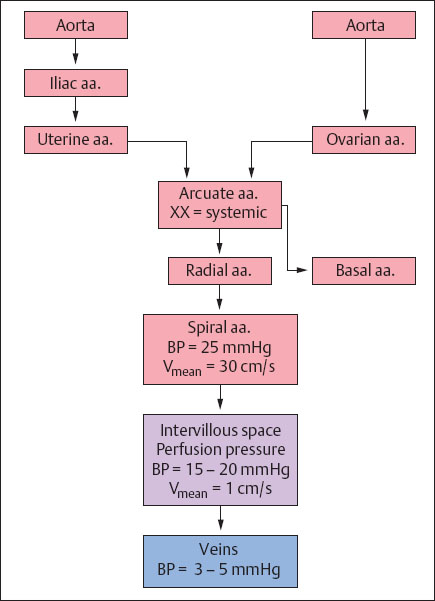
Fig. 3.1 Schematic representation of the uteroplacental blood supply.
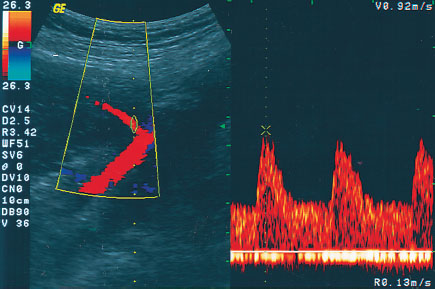
Fig. 3.2 Display of the origin of the uterine a. from the iliac a. with corresponding normal Doppler sonogram.
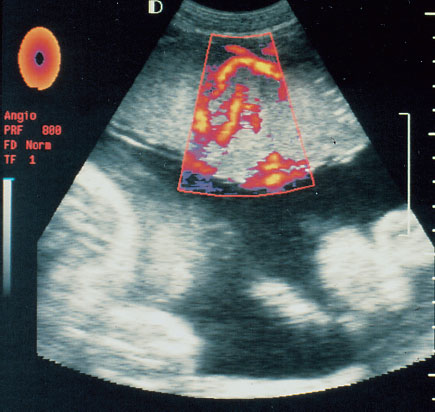
Fig. 3.3 Display of placental perfusion. This type of examination is currently not clinically useful.
Drainage of the intervillous space is assured by veins in the decidual septa and sinuses in the edge of the placenta. Possibly pulsations in the companion arteries and perhaps Braxton Hicks contractions enhance venous drainage. When the inferior vena cava is obstructed, as in the supine position, drainage may continue through the ovarian v.
Every placental cotyledon is supplied by one spiral a. This has led to speculation that the presence of a uterine vessel may induce cotyledon formation. According to this model there are some 40–60 such units combining function and circulation.
The vessels adapt to pregnancy by considerable dilatating. Thus, the diameter of the uterine aa. increases by one and a half to threefold, the retroplacental arcuate aa. tenfold and the spiral aa. thirtyfold. Uteroplacental hemodynamics are further characterized by blood pressure and flow changes in these vessels. Systemic blood pressure remains almost constant as far as the arcuate aa. The blood pressure then declines to 25 mmHg at the mouths of the spiral aa. Hence the perfusion pressure (PP) in the intervillous space is quite low—about 15–20 mmHg. Finally in the veins a pressure of 3–5 mmHg may be expected. In the quiescent uterus about 90% of the blood supply reaches the intervillous space. The mean flow velocity of the blood in the spiral aa. is about 30 cm/s. The intervillous space contains about 150 mL at term, and the blood there moves at a rate of about 1 cm/s. On an average about 600 mL of blood flow through this open space along a pressure gradient of about 15–20 mmHg.
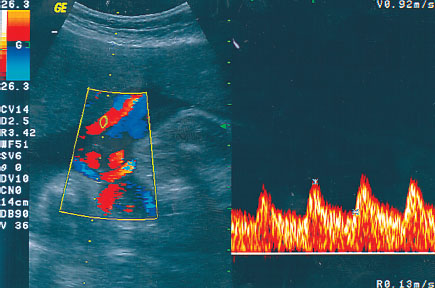
Fig. 3.4 Display of the umbilical vessels by color Doppler and Doppler sonogram.
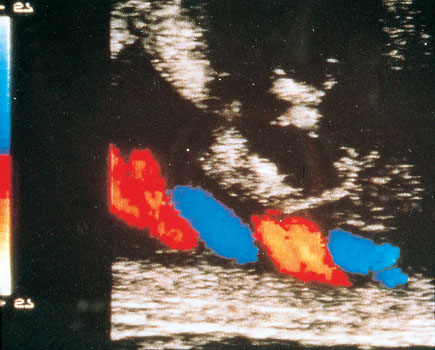
Fig. 3.5 Color Doppler display of the umbilical vessels.
Fetoplacental Blood Supply
In contrast to the uteroplacental vascular bed the fetoplacental bed is closed. To a large extent it lies outside the fetus. The two umbilical aa. (Fig. 3.4) arise from the internal iliac aa. Normally they wind helically over a variable distance of 20–140 cm (50 cm on average) through the amniotic cavity to the surface of the placenta. There they divide into the vessels of the chorionic plate, which in turn divide into the vessels of the villi. These chorionic vessels are characterized by the absence of nerves and elastic coats. On the other hand, they have a strongly developed musculature and swollen epithelial cells. The latter prepare the vessels for rapid occlusion after delivery. It has been theorized that the vessels in the villi provide an arteriolar type of action during pregnancy, reducing pressure and retarding flow before the blood enters the sinusoidally modified capillaries.
The return flow runs to the unpaired umbilical v., parallel to the arterial flow. It then drains intra-abdominally into the portal sinus (sinus venosus), where the flow is divided into the left hepatic a., the left portal vein, and the ductus venosus, which drains into the left lobe of the liver (Fig. 3.5).
Fetal Blood Supply
The fetal circulation (Fig. 3.6) is marked by three major shunts: the ductus venosus (ductus venosus arantii), the foramen ovale, and the ductus arteriosus (of Botalli).
Almost 20–30% of the oxygenated blood from the umbilical v. is shunted past the liver to the heart by the ductus venosus (Fig. 3.7). This well-oxygenated blood then largely bypasses the pulmonary circulation and passes from the venous side directly into the great arteries of the systemic circulation. Clearly this route moves the flow of oxygen- and nutrient-enriched blood preferentially to the heart and brain (streamlining effect) through the ductus venosus, and the foramen ovale.
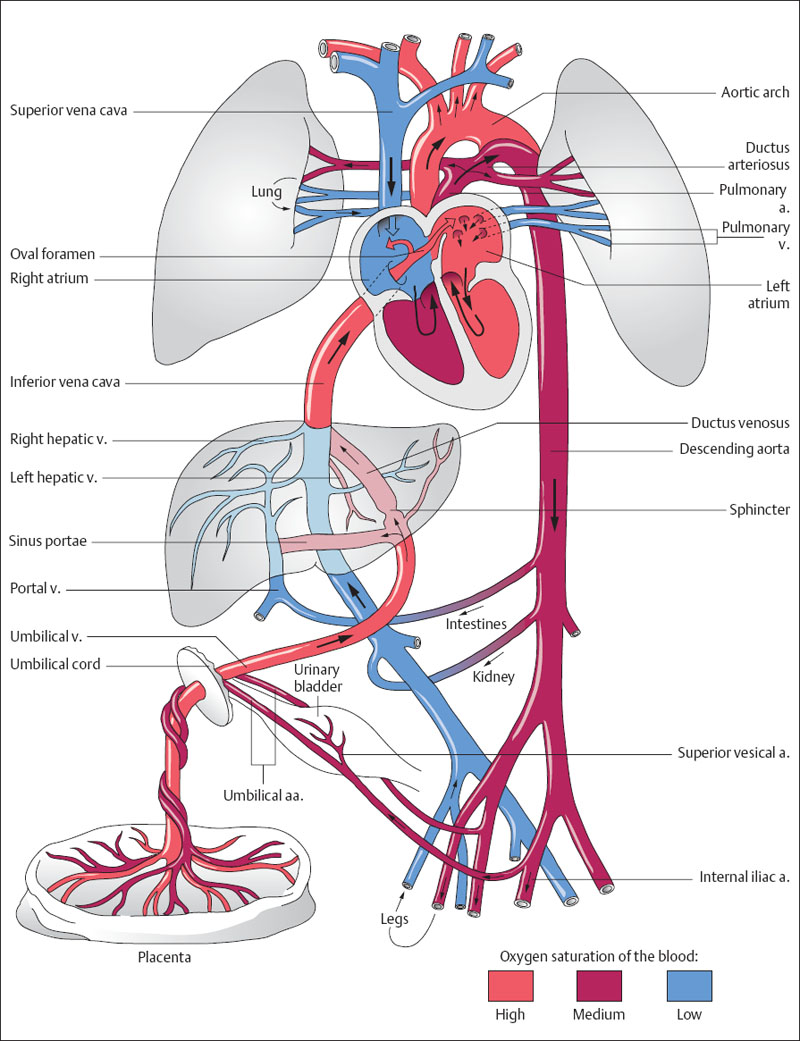
Fig. 3.6 Simplified representation of the fetal circulation. The colors indicate the oxygen saturation of the blood, the arrows the direction of blood flow (after Moore 1996).
The two cardiac circulations flow functionally in parallel with almost complete pressure equalization at the level of the atria. To this end two shunts are provided: The first, the ductus arteriosus, connects the pulmonary a. with the descending aorta. The second is the foramen ovale, which, by connecting the left atrium with the right, assures a shunt to the ascending aorta (Fig. 3.8). The peripheral resistance of the vascular bed supplied by the right heart, which includes the umbilical cord and the placenta, is normally lower than that of the left heart, which preferentially supplies the head, neck, and upper extremities. This probably is the reason for the greater stroke volume ejected by the right heart than the left. The ratio of left to right has been determined to be between 1.3 and 1.8. This ratio may be altered by an increase in the afterload in the descending aorta, leading to a pressure buildup with resulting shunt obstruction or reversal.
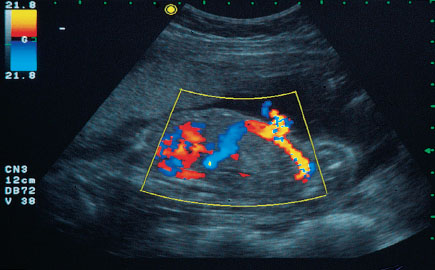
Fig. 3.7 Display of the origin of the umbilical cord and the intra-abdominal course of the vessels. Ascending from the right: the umbilical aa. from the fetal iliac a.; descending from above to the left: the intra-abdominal part of the umbilical cord and the ductus venosus.
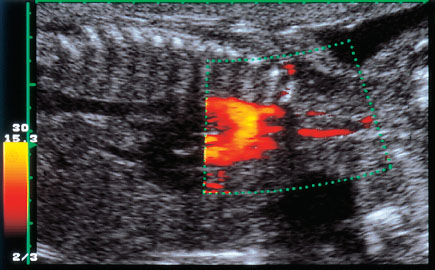
Fig. 3.8 Display of an aortic arch with the vessels ascending from it.
Methods of Examining Specific Vessels
Displaying the Maternal Vessels
The primary examination here is of the two uterine aa. that arise from the internal iliac aa. and divide into smaller uterine branches in the myometrium. The uterine aa. must be examined by color Doppler, since these vessels cannot be adequately defined in black and white.
Examining the Uterine Arteries in the Second Trimester:
 Localization: At the lower pole of the uterus in the myometrium bilaterally.
Localization: At the lower pole of the uterus in the myometrium bilaterally.
 Examination technique: The uterine a. is first located by color Doppler sonography. The transducer is applied above the inguinal region as shown schematically in Figure 3.9. The Doppler window must be placed relatively superficially. First locate the iliac a. and v. with the color Doppler, then redirect the transducer medially to the myometrium. Usually the uterine a. will be located with little difficulty where it runs from its origin from the internal iliac a. (Fig. 3.10) into the myometrium toward the transducer. The transducer may also be moved in the reverse direction, from the amniotic cavity laterally, to display the course of the uterine a. The characteristic Doppler waveform of the uterine a. can then be identified from the Doppler spectrum. The course of the uterine a. can almost always be displayed, while the arcuate branches can as a rule only be displayed as points (Fig. 3.11).
Examination technique: The uterine a. is first located by color Doppler sonography. The transducer is applied above the inguinal region as shown schematically in Figure 3.9. The Doppler window must be placed relatively superficially. First locate the iliac a. and v. with the color Doppler, then redirect the transducer medially to the myometrium. Usually the uterine a. will be located with little difficulty where it runs from its origin from the internal iliac a. (Fig. 3.10) into the myometrium toward the transducer. The transducer may also be moved in the reverse direction, from the amniotic cavity laterally, to display the course of the uterine a. The characteristic Doppler waveform of the uterine a. can then be identified from the Doppler spectrum. The course of the uterine a. can almost always be displayed, while the arcuate branches can as a rule only be displayed as points (Fig. 3.11).
 Significance: Whether the maternal blood supply is sufficient or not after the end of the second trimester is decided following completion of the trophoblast invasion.
Significance: Whether the maternal blood supply is sufficient or not after the end of the second trimester is decided following completion of the trophoblast invasion.
 Flow profile: The course of the vessels can be displayed by swinging the transducer medially from the common iliac A. and V. in color mode (Fig. 3.12). The display shows a moderately steep systolic rise and a continuous decline to end-diastole, as well as poor demarcation between systole and early diastole (Figs. 3.13, 3.14).
Flow profile: The course of the vessels can be displayed by swinging the transducer medially from the common iliac A. and V. in color mode (Fig. 3.12). The display shows a moderately steep systolic rise and a continuous decline to end-diastole, as well as poor demarcation between systole and early diastole (Figs. 3.13, 3.14).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree