CHAPTER 87 Vascular Surgery
CAROTID ENDARTERECTOMY
Indications
Vascular surgeons are particularly stringent about the indications for carotid endarterectomy because this is one of the few prophylactic operations. Indications for carotid endarterectomy are based on two large, multicenter, randomized trials comparing best medical therapy (antiplatelet) and surgical therapy for carotid stenosis. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) examined patients with a previous history of stroke, transient ischemic attack, or amaurosis fugax within 3 months of enrollment.1 During 2 years, the risk of stroke in patients with a 70% to 99% stenosis was reduced from 26% to 9% with carotid endarterectomy. The risk of stroke in patients with a 50% to 69% stenosis was reduced from 22% to 16% during 5 years. Given the less substantial benefit seen with the moderate-grade lesions, most vascular surgeons would recommend carotid endarterectomy to symptomatic patients with 50% to 69% stenosis only if they have a substantial life expectancy and low risk of complications related to the surgical intervention. Finally, subgroup analysis revealed an increased risk of stroke in medically treated patients with contralateral carotid occlusions and ulcerated plaques.
The Asymptomatic Carotid Atherosclerosis Study (ACAS) randomized asymptomatic patients to medical and surgical therapy.2 Carotid endarterectomy reduced the 5-year risk of stroke from 11% to 5% in patients with 60% to 99% stenosis compared with medical therapy. Given an absolute stroke risk reduction of 6% during 5 years, further studies have shown that surgical therapy is most beneficial in patients with 80% to 99% stenosis and in men compared with women. This equates to changing the outcome of approximately 1 in 20 to 30 patients, making the safety and risk reduction in the conduct of intervention for asymptomatic patients of paramount importance. This fact significantly affects the decision-making process regarding carotid imaging for either carotid endarterectomy or carotid stenting. In the ACAS trial, there was a 1.5% risk of stroke from diagnostic angiography alone.
Contraindications
Further studies examined carotid endarterectomy and found that it can be safely performed in patients deemed at high risk, including those 80 years or older and others with significant comorbid conditions, with combined stroke and mortality rates comparable to those found in the NASCET and ACAS studies. Contralateral occlusion was the only predictor for moderately increased perioperative risk of stroke and reduced long-term survival.3
Outcomes and Complications
One rare complication is hyperperfusion syndrome, which is characterized by a severe, unilateral headache occurring 3 to 7 days after endarterectomy. This has been attributed to the sudden restoration of normal arterial pressures in a vascular bed that has not seen pulsatility and normal pressures for a long period, thus leading to atrophy of the arteriolar restrictive mechanisms and impaired ability of the cerebrovascular circulation to autoregulate after the reestablishment of cranial blood flow. MRI may show reversible vasogenic edema similar to that observed in the posterior leukoencephalopathy syndrome.4 Treatment includes control of the hypertension that is frequently associated with this phenomenon to prevent cerebral hemorrhage until cerebral autoregulation is reestablished, typically for a few days to 1 week.
Imaging Findings
Preoperative Assessment
Duplex ultrasonography is the most common technique used to assess patients suspected of having extracranial cerebrovascular disease. B-mode ultrasonography is used to define location of the stenotic lesion, and Doppler examination is used to measure velocities across the stenosis (Fig. 87-1). B-mode ultrasonography not only delineates the location of a stenosis but also describes the characteristics of the plaque itself. Plaque ulceration as well as plaque calcification or hemorrhage may be seen. B-mode ultrasonography can also evaluate plaque echogenicity and the presence of thrombus. Soft, friable plaques on ultrasound examination are typically less stable than echoic plaques are. Mobile thrombus on ultrasound examination has been associated with an increased risk of stroke.
Velocity measurements across a stenosis are the most important aspect of the preoperative assessment for the vascular surgeon because these measurements are directly correlated with degree of stenosis. Strandness5 first reported a sensitivity of 99% and a specificity of 84% with duplex ultrasound criteria for the evaluation of carotid disease compared with conventional angiography (Table 87-1). More recently, it has been observed that diagnostic criteria must be altered in the setting of a contralateral severe stenosis or complete occlusion of the internal carotid artery because of a compensatory increase in carotid blood flow. By use of the criteria of AbuRahma,6 the accuracy of duplex ultrasound measurements can be increased to 96%. No matter which criteria are used, they must be validated by individual vascular laboratories as this technique may be operator and instrument dependent.
TABLE 87-1 Duplex Ultrasound Criteria for Diagnosis of Internal Carotid Artery Stenosis
| Stenosis | Criteria | |
|---|---|---|
| Strandness | AbuRahma | |
| Normal | PSV < 125 cm/sec | PSV < 125 cm/sec |
| No SB | No SB | |
| Flow reversal in bulb | ||
| 1%-15% | PSV < 125 cm/sec | PSV < 125 cm/sec |
| No or minimal SB | Minimal SB | |
| Flow reversal in bulb absent | ||
| 16%-49% | PSV > 125 cm/sec | PSV < 140 cm/sec |
| Marked SB | EDV < 140 cm/sec | |
| 50%-79% | PSV > 125 cm/sec | PSV ≥ 140 cm/sec |
| EDV < 140 cm/sec | EDV < 140 cm/sec | |
| 80%-99% | PSV < 125 cm/sec | PSV > 140 cm/sec |
| EDV > 140 cm/sec | EDV < 140 cm/sec | |
| Occlusion | No flow | No flow |
EDV, end-diastolic velocity; PSV, peak systolic velocity; SB, spectral broadening.
Modified from Strandness DE Jr. Extracranial arterial disease. In Strandness DE Jr (ed). Duplex Scanning in Vascular Disorders, 2nd ed. New York, Raven Press, 1993, pp 113-158; and AbuRahma AF, Richmond BK, Robinson PA, et al. Effect of contralateral severe stenosis or carotid occlusion on duplex criteria of ipsilateral stenoses: comparative study of various duplex parameters. J Vasc Surg 1995; 22:751-761.
CTA has been used to delineate extracranial cerebrovascular and carotid arch anatomy and has the advantages of minimal discomfort for the patient, relatively low radiation doses, and demarcation of calcific plaques in both the carotid arteries and the aortic arch. Recent three-dimensional reconstructions provide the surgeon with a greater ability in preoperative planning (Fig. 87-2).
MRA is another tool of the vascular surgeon and can be particularly useful in patients with an allergy to intravenous contrast material. Time-of-flight MRA has a tendency to overestimate the degree of stenosis because of local blood flow turbulence. Overestimation of time-of-flight MRA can be reconciled with the performance of gadolinium-enhanced three-dimensional MRA.7 Both techniques also demonstrate intracranial vessel anatomy along with patency of the communicating arteries.
Catheter angiography (Fig. 87-3), previously considered the gold standard for the assessment of extracranial cerebrovascular disease, has been used less frequently in uncomplicated patients because of the approximately 1.5% risk of stroke. Catheter angiography is now typically reserved for evaluation of patients in whom results from duplex ultrasonography and either CTA or MRA are discordant.
CAROTID-SUBCLAVIAN BYPASS
Description
Carotid-subclavian bypass may be performed through a remote cervical incision just lateral to the sternocleidomastoid muscle. The jugular vein is reflected medially to expose the common carotid artery. The anterior scalene muscle is then divided to expose the subclavian artery. Once proximal and distal control of each artery is obtained, bypass is typically performed with a prosthetic graft as patency is superior to autogenous conduit in this position.8 On occasion, concomitant disease of the ipsilateral common carotid artery precludes its use as an inflow vessel. In these cases, the contralateral common carotid may be used. The prosthetic graft would then be tunneled across the midline through the retropharyngeal space; this is a more direct path and avoids erosion of the overlying skin or interference with possible subsequent sternotomy or tracheostomy.
Outcomes and Complications
Outcomes from carotid-subclavian bypass are excellent, with 10-year patency rates of 84%.9 Complications range from a 0% to 1% stroke rate to a 0% mortality rate.10,11
Imaging Findings
Preoperative Assessment
Duplex ultrasonography may be used to screen for subclavian stenosis but is limited by the bony structures of the mediastinum. Its usefulness lies in its ability to assess for reversal of blood flow in the vertebral artery with upper extremity exercise (Fig. 87-4) and the adequacy of the common carotid artery for inflow.
Preoperative Planning
Once a subclavian stenosis has been identified, preoperative planning may be accomplished with CTA or MRA (Fig. 87-5). Both evaluate the exact location of the lesion as well as assess possible inflow and outflow vessels. Full appraisal of the aortic arch, its branches, and neck extracranial cerebrovascular vessels is necessary to rule out other pathologic processes. Resolution of the aortic arch and these large-caliber vessels with CTA and MRA is excellent, and they may replace standard angiography.
Digital subtraction angiography may be a useful adjunct for preoperative planning before carotid subclavian bypass. Angiography can identify major inflow and outflow vessels as well as important collaterals (Fig. 87-6).
THORACOABDOMINAL AORTIC ANEURYSM REPAIR
Description
Thoracoabdominal aortic aneurysm (TAAA) repair is performed through a retroperitoneal approach combined with thoracotomy. Intraoperative management of patients with thoracoabdominal aneurysms is dependent on the extent of the aneurysmal degeneration of the aorta. Patients with Crawford extent I and II TAAAs generally require either continuous distal perfusion or left-sided heart bypass; these types of aneurysms are associated with the greatest risk of paraplegia (Fig. 87-7). In the thorax, the recurrent laryngeal and vagus nerves are gently retracted off from the aorta. After cross-clamping of the aorta, the proximal anastomosis is sewn in an endoaneurysmal fashion (end-to-end within the aneurysm sac). All large intercostal arteries from T7 to L2 are reimplanted into the graft, followed by the visceral vessels. If stenoses at the origin of these arteries are encountered, an endarterectomy may be performed. Finally, the distal anastomosis is performed in endoaneurysmal fashion to an uninvolved portion of the distal aorta.

 FIGURE 87-1
FIGURE 87-1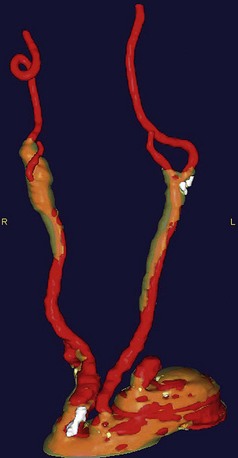
 FIGURE 87-2
FIGURE 87-2
 FIGURE 87-3
FIGURE 87-3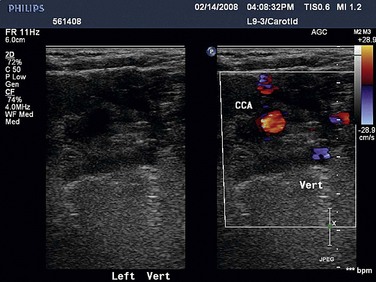
 FIGURE 87-4
FIGURE 87-4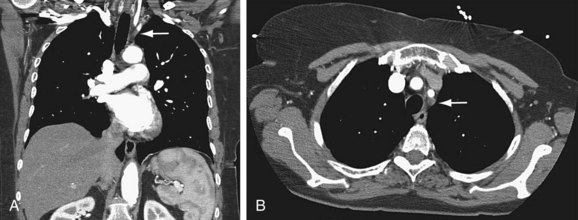
 FIGURE 87-5
FIGURE 87-5
 FIGURE 87-6
FIGURE 87-6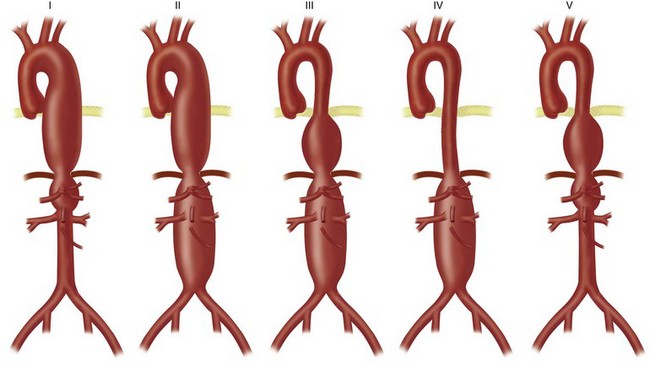
 FIGURE 87-7
FIGURE 87-7


