Vasculitis
The vasculitides are a diverse group of diseases characterized by inflammation within and around blood vessel walls. This inflammatory process can affect large and mediumsize vessels as well as small vessels and capillaries that are below the resolution of computed tomography (CT). Behçet syndrome, Hughes-Stovin syndrome, Takayasu arteritis, and giant cell arteritis tend to affect the large and medium-size arteries, whereas Wegener granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome, Goodpasture syndrome, cryoglobulinemia, Henoch-Sch ˝onlein purpura, connective tissue diseases, and drug-induced vasculitis tend to involve small pulmonary vessels and capillaries. The vasculitides can also be classified according to histologic patterns. For example, giant cell infiltrate is seen in giant cell arteritis and Takayasu arteritis; granulomatous infiltrate in Wegener granulomatosis, microscopic polyangiitis, and Churg-Strauss syndrome; leukocytoclastic infiltrate in cryoglobulinemia, Henoch-Sch ˝onlein purpura, and Behçet syndrome; and lymphocytic infiltrate in connective tissue, Behçet syndrome, and drug-induced vasculitides. Good-pasture syndrome, Wegener granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome, and systemic lupus erythematosus are all possible causes of the pulmonary-renal syndrome. The most common respiratory symptom of the pulmonary vasculitides is hemoptysis, which can be life-threatening. This chapter summarizes the pulmonary vasculitides and illustrates the imaging findings.
 Behçet Syndrome
Behçet Syndrome
 Behçet syndrome is a chronic multisystem vasculitis characterized by recurrent oral and genital ulcers and uveitis.
Behçet syndrome is a chronic multisystem vasculitis characterized by recurrent oral and genital ulcers and uveitis.
 It occurs most commonly in Turkey and Southeast Asia and is associated with human leukocyte antigen B51 and with Staphylococcus aureus, Prevotella, Chlamydia, and hepatitis C infections.
It occurs most commonly in Turkey and Southeast Asia and is associated with human leukocyte antigen B51 and with Staphylococcus aureus, Prevotella, Chlamydia, and hepatitis C infections.
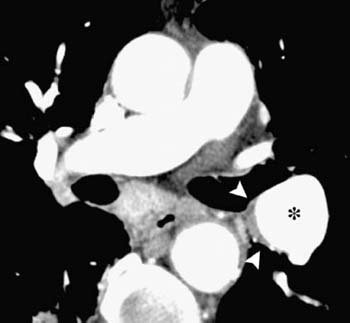
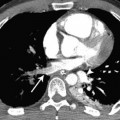
 Thoracic manifestations include arterial aneurysms (Fig. 7.1), vascular thrombosis, pulmonary infarction, hemorrhage, organizing pneumonia, lymphadenopathy, and pleural effusion.
Thoracic manifestations include arterial aneurysms (Fig. 7.1), vascular thrombosis, pulmonary infarction, hemorrhage, organizing pneumonia, lymphadenopathy, and pleural effusion.
 The pulmonary artery aneurysms in Behçet syndrome may regress with immunosuppressive therapy. However, embolization may be necessary.
The pulmonary artery aneurysms in Behçet syndrome may regress with immunosuppressive therapy. However, embolization may be necessary.
Fig. 7.1 Behçet syndrome in a 50-year-old man with hemoptysis. CT scan shows aneurysmal dilatation of a left interlobar pulmonary artery (*) with medial mural thickening (arrowheads). (Reproduced with permission from author and publisher: Castañer E, Gallardo X, Rimola J, et al. Congenital and acquired pulmonary artery anomalies in the adult: radiologic overview. Radiographics 2006;26(2): 349–371.)
 It is important that pulmonary vasculitis is not mistaken for pulmonary thromboembolic disease because fatalities have occurred shortly after the initiation of anticoagulation.
It is important that pulmonary vasculitis is not mistaken for pulmonary thromboembolic disease because fatalities have occurred shortly after the initiation of anticoagulation.
 Hughes-Stovin syndrome may present with recurrent thrombophlebitis and pulmonary artery aneurysm formation and rupture. It is considered by some to be a forme fruste of Behçet syndrome.
Hughes-Stovin syndrome may present with recurrent thrombophlebitis and pulmonary artery aneurysm formation and rupture. It is considered by some to be a forme fruste of Behçet syndrome.
 Takayasu Arteritis
Takayasu Arteritis
 Takayasu arteritis is a chronic, progressive systemic arteritis of unknown cause that classically involves the aorta and its branches.
Takayasu arteritis is a chronic, progressive systemic arteritis of unknown cause that classically involves the aorta and its branches.
 It is most common in East Asia, affecting women of child-bearing age.
It is most common in East Asia, affecting women of child-bearing age.
 Pulmonary vascular involvement occurs in 50 to 80% of cases.
Pulmonary vascular involvement occurs in 50 to 80% of cases.
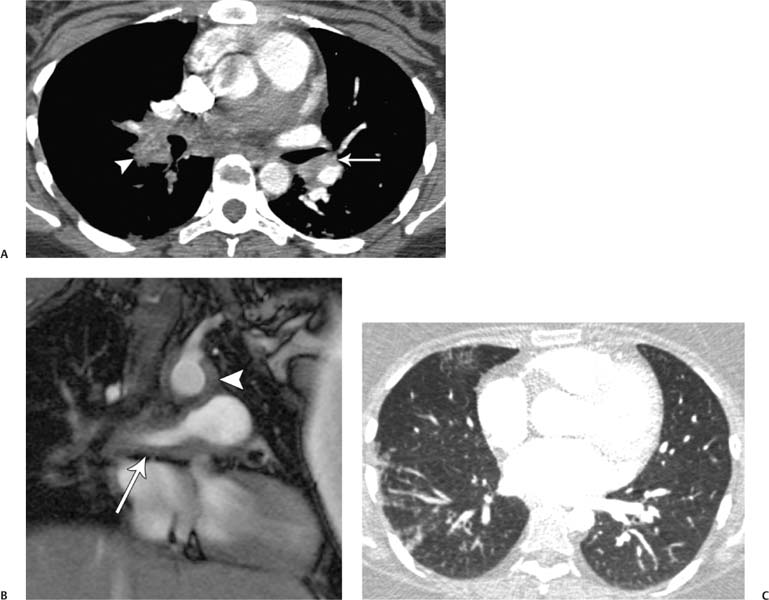
 Pulmonary vascular changes include wall thickening, in situ thrombosis, stenosis, occlusion (Fig. 7.2), and pulmonary hypertension.
Pulmonary vascular changes include wall thickening, in situ thrombosis, stenosis, occlusion (Fig. 7.2), and pulmonary hypertension.
 Organization of thrombosis and recanalization occur; the new vessels are often vasa vasorum that are branches of the bronchial artery.
Organization of thrombosis and recanalization occur; the new vessels are often vasa vasorum that are branches of the bronchial artery.
 Mosaic attenuation and peripheral lung nodules (Fig. 7.2C) have been described, indicative of involvement of small pulmonary arteries and adjacent lung tissue.
Mosaic attenuation and peripheral lung nodules (Fig. 7.2C) have been described, indicative of involvement of small pulmonary arteries and adjacent lung tissue.
 Giant Cell Arteritis
Giant Cell Arteritis
 Giant cell arteritis is an idiopathic vasculitis that involves large arteries, predominantly the extracranial carotid branches and the aorta; it rarely involves central pulmonary arteries.
Giant cell arteritis is an idiopathic vasculitis that involves large arteries, predominantly the extracranial carotid branches and the aorta; it rarely involves central pulmonary arteries.
 The classic clinical picture is a woman older than 50 years with polymyalgia rheumatica, headache, systemic illness, and a high erythrocyte sedimentation rate.
The classic clinical picture is a woman older than 50 years with polymyalgia rheumatica, headache, systemic illness, and a high erythrocyte sedimentation rate.
Fig. 7.2 (A–C) Takayasu arteritis in a 28-year-old woman. (A) CT demonstrates eccentric enhancing wall thickening of the left lower lobe pulmonary artery (arrow) and occlusion of the right lower lobe pulmonary artery (arrowhead). (B) Contrast material–enhanced magnetic resonance image (MRI) demonstrates wall thickening and enhancement of the right lower lobe pulmonary artery (arrow) just before the obstruction. There is also involvement of the aorta (arrowhead). (C) CT on lung windows shows subpleural and peribronchovascular nodules affecting the right lung.
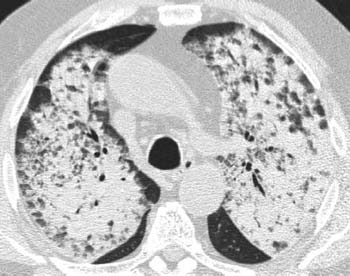
Fig. 7.3 Wegener granulomatosis in an 83-year-old man. High-resolution CT of the upper lobes demonstrates diffuse bilateral consolidation, consistent with diffuse pulmonary hemorrhage.
 The CT features of giant cell arteritis of the pulmonary arteries are similar to those of Takayasu arteritis, with arterial wall thickening, stenosis, and in situ thrombosis.
The CT features of giant cell arteritis of the pulmonary arteries are similar to those of Takayasu arteritis, with arterial wall thickening, stenosis, and in situ thrombosis.
 Wegener Granulomatosis
Wegener Granulomatosis
 It may also affect the joints, eyes, nervous system, heart, gastrointestinal tract, thyroid gland, liver, and breasts.
It may also affect the joints, eyes, nervous system, heart, gastrointestinal tract, thyroid gland, liver, and breasts.
 The mean age at onset is the fifth decade.
The mean age at onset is the fifth decade.
 Notable laboratory findings are positivity for c-ANCA (circulating anti-neutrophil cytoplasmic antibody) and anti-PR3 (anti-proteinase 3) in 90% of cases, with a high erythrocyte sedimentation rate.
Notable laboratory findings are positivity for c-ANCA (circulating anti-neutrophil cytoplasmic antibody) and anti-PR3 (anti-proteinase 3) in 90% of cases, with a high erythrocyte sedimentation rate.
 Several patterns of Wegener granulomatosis can affect the thorax: diffuse alveolar hemorrhage (Fig. 7.3
Several patterns of Wegener granulomatosis can affect the thorax: diffuse alveolar hemorrhage (Fig. 7.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree