1. Signs and symptoms of raised intracranial pressure (headache, nausea, vomiting, transient visual obscurations, or papilledema)
2. No localizing signs with the exception of abducens (sixth) nerve palsy
3. The patient is awake and alert
4. Normal CT/MRI findings without evidence of venous sinus thrombosis
5. LP opening pressure of >25 cm H2O and normal biochemical and cytological composition of CSF
6. No other explanation for the raised intracranial pressure
Table 2
Friedman and Jacobson Criteria for diagnosing idiopathic intracranial hypertension
1. If symptoms are present, they may only reflect those of generalized intracranial hypertension or papilledema |
2. If signs are present, they may only reflect those of generalized intracranial hypertension or papilledema |
3. Documented elevated intracranial pressure measured in the lateral decubitus position |
4. Normal CSF composition |
5. No evidence of hydrocephalus, mass, structural, or vascular lesion on MRI or contrast-enhanced CT for typical patients and MRI and MR venography for all others |
6. No other cause of intracranial hypertension identified |
Imaging
Computed tomography (CT) or magnetic resonance imaging (MRI) studies show normal or small ventricles and normal brain parenchyma.
MRI typically shows flattening of the posterior aspect of the globes, dilatation of the optic nerve sheathes (Fig. 1), with elevation of the optic disc sometimes visible on axial T2-weighted MRI images, and occasionally an acquired Chiari malformation.
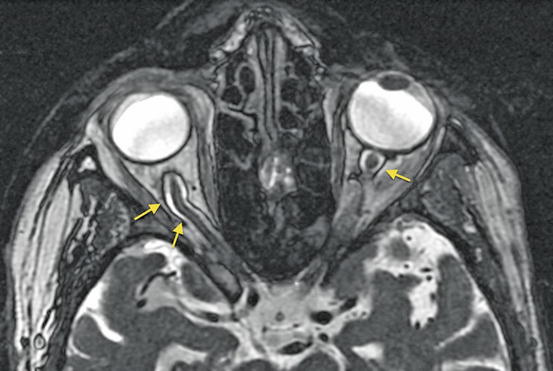
Fig. 1
Dilated optic nerve sheathes seen on thin section T2-weighted FIESTA images in long-standing BIH (arrows)
There must be no mass lesion or any obvious cause for elevated intracranial pressure.
Other features of chronically raised intracranial pressure such as a partially empty sella are frequently present, and cerebrospinal fluid (CSF) leaks are sometimes seen.
MR venography (MRV) shows that venous sinus stenoses are frequently present in patients with BIH.
There has been much controversy as to whether these stenoses are primary and causative or secondary to raised intracranial pressure, or possibly both.
Filling defects due to large arachnoid granulations can also be seen in the transverse sinuses in asymptomatic patients, but it is not correct to assume that such filling defects are always incidental.
Can be done with conventional time-of-flight MRV techniques.
Artifacts due to saturation frequently impair conventional MRV studies leading to artifactual stenoses or disregarding of real stenoses.
Much better studies can be obtained using ATECO (auto-triggered elliptic centric-ordered) techniques utilizing gadolinium contrast enhancement to coincide interrogation of the central part of K-space with peak gadolinium concentration and thereby greatly improve the quality of MRV studies.
Rotating maximum intensity projection images and 3-D modelling allow the cranial venous sinuses to be inspected from almost any angle and the possibility of venous sinus abnormalities can be accurately and noninvasively assessed. Figure 2 shows normal MRV while Fig. 3 shows abnormal MRV.

Fig. 2
Normal ATECO MR Venogram showing exquisite demonstration of venous structures
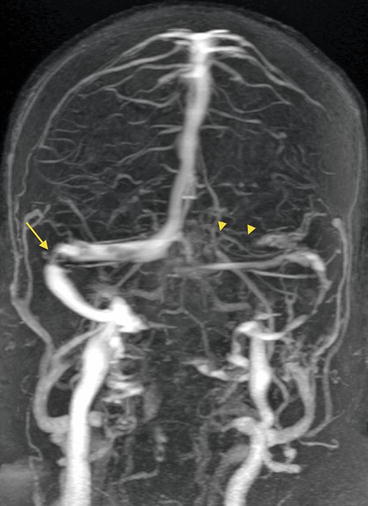
Fig. 3
Abnormal ATECO MR Venogram showing right transverse sinus stenosis (arrow) and atretic left transverse sinus (arrowheads)
Many patients with BIH can be shown to have abnormalities in the venous sinuses. Farb et al. showed that bilateral sinovenous stenoses were seen in 27 of 29 patients with IIH and in only 4 of 59 controls.
Where these patients can be shown to have increased venous sinus pressure above the stenosis by DRCVM, we hypothesize that relief of venous hypertension could increase CSF absorption and thereby decrease intracranial pressure.
The main site of CSF absorption is thought to be the arachnoid granulations (arachnoid villi) of the lateral lacunae and superior sagittal sinus. Davson et al. showed that absorption of CSF depends on a pressure gradient between the subarachnoid space and the venous sinus of approximately 3 mmHg in health. Thus when venous pressure rises, CSF pressure must also rise in order for CSF absorption to continue.
Bateman first proposed that a disordered positive biofeedback mechanism may be present in BIH where elevated CSF pressure compresses the venous sinuses, leading to further venous hypertension and further elevation of CSF pressure.
Bateman and others have also shown that cerebral blood flow is increased in many patients with BIH, and decreases after treatment, raising the possibility that an additional disordered biofeedback loop may be operating leading to increased CSF formation.
If venous sinus narrowing is identified in a patient with persistent symptoms of BIH despite medical management, and venous sinus stenting is being considered, the patient should proceed to DRCVM in order to assess the functional significance of the stenosis identified.
Indications for Treatment, Management Alternatives
Any patient with symptoms should be offered medical management initially, with surgical or endovascular therapies reserved for nonresponders.
The goal of treatment is to preserve vision and manage headache.
Medical Management
Patients with BIH are typically managed with drugs that decrease the rate of CSF formation such as acetazolamide and topiramide (and occasionally furosemide), and are usually advised to lose weight (with the aim of decreasing central venous pressure).
Lumbar puncture with 20–30 ml CSF drainage typically produces immediate relief of symptoms, and this relief may last far longer than the amount of time required for the body to replace the volume of CSF withdrawn.
Repeated lumbar punctures may be required.
Conventional Surgical Management
If not satisfactorily managed, patients may be considered for CSF diversion techniques such as optic nerve sheath fenestration, lumboperitoneal shunting or ventriculoperitoneal shunting, or methods aiming to increase the compliance of the cranial cavity such as subtemporal decompression.
Shunt procedures are frequently associated with technical failures (blockage, kinking, disconnection, or dislodgement) resulting in a need for shunt revision in ≥30 % of patients per year.
Endovascular Therapy, Venous Sinus Stenting
Patients who fulfill diagnostic criteria for BIH and are not satisfactorily managed by medical therapies can be considered for suitability for endovascular treatment as an alternative to surgical CSF-diversion therapies.
Higgins et al. reported the first case in 2002, and since then small case series have been reported, prior to the series of 52 cases reported by Ahmed et al.
Interest is growing in the literature but stenting remains a controversial therapeutic alternative and is not offered in all centers.
Evaluation Prior to Venous Sinus Stenting
All patients with a venous sinus stenosis identified on MRV should have the functional significance of this stenosis evaluated with cerebral venography and pressure measurement studies prior to consideration for stenting.
Some stenoses identified on MRV are not associated with elevated venous pressures or pressure gradients and should not be stented.
Direct Retrograde Cerebral Venography and Manometry
This is an invasive procedure performed in an angiography suite.
The study is usually an outpatient procedure performed under mild conscious sedation after fasting for 4–6 h.
A femoral venous puncture is performed after administration of local anesthesia and a 6 French sheath placed in the common femoral vein.
A 90-cm 6 French guiding catheter (e.g., Cordis Envoy Mod CBL) is placed through the IVC, right atrium, and SVC into the dominant internal jugular vein terminating just below the skull base.
A jugular venogram is performed to exclude extracranial venous obstruction or stenosis.
A large-caliber microcatheter (e.g., Boston Scientific Renegade Hi-Flo) is then manipulated over a 014″ guidewire (e.g., Boston Scientific Transend) through the jugular foramen, sigmoid, and transverse sinus and into the superior sagittal sinus.
The catheter tip is placed as far anteriorly as the coronal suture.
Venograms are then performed using hand injection with a high-pressure 3 cm3 syringe (e.g., Merit Medallion), obtaining right and left oblique frontal, lateral, and oblique lateral projections to demonstrate venous sinus stenoses.
The importance of obtaining multiple oblique projections of the transverse sinuses cannot be overemphasized.
Once adequate venograms have been performed, pressure measurements are obtained at multiple points during catheter pullback using an electronic manometer with the transducer zeroed to room air at the level of the patient’s heart.
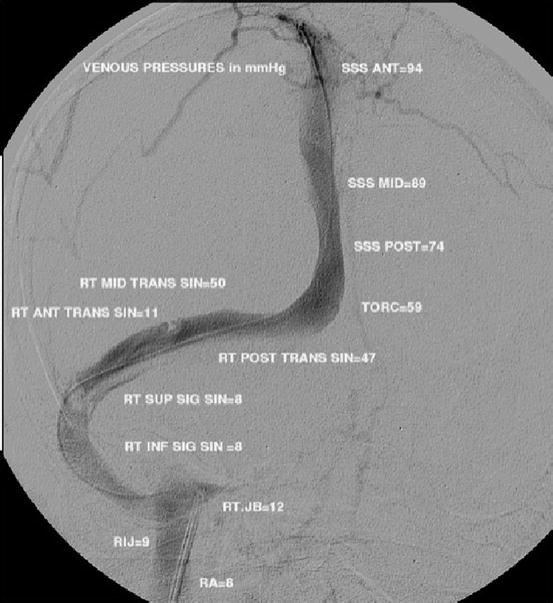
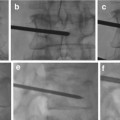
Pressures are recorded on a standardized form (Fig. 4). Continuous recording of pressure waves on a paper chart is useful to recognize the presence of focal pressure gradients (Fig. 5) and mean pressures are annotated on images’ multiple locations (Figs. 6 and 7).
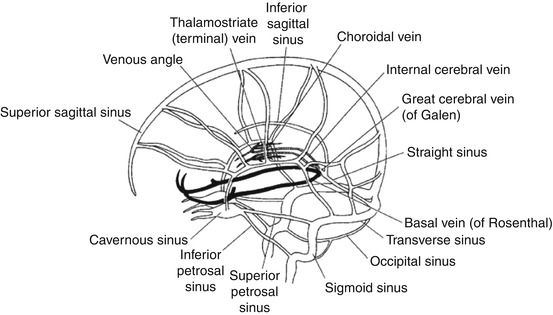
Fig. 4
Standardized pressure-recording form for DRCVM studies. DRCVM direct retrograde cerebral venography and manometry
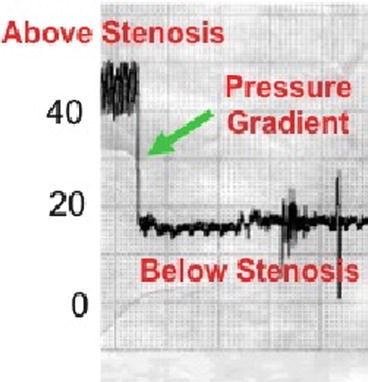
Fig. 5
Pressure trace recorded during catheter pullback across transverse sinus stenosis confirming sharp pressure gradient across stenosis
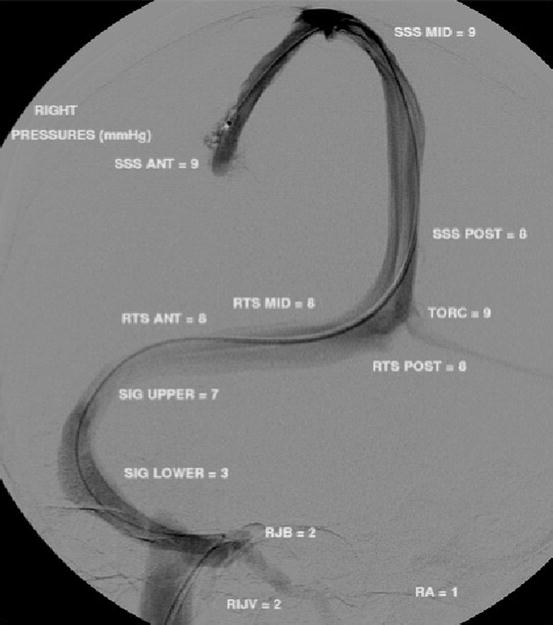
Fig. 6
Normal DRCVM study with normal pressures and no pressure gradient in patients with dominant right transverse sinus and atretic left transverse sinus. DRCVM direct retrograde cerebral venography and manometry