Key Points
- ▪
Knowledge of normal and variant anatomy of the upper extremity venous vasculature is critical.
- ▪
A standardized and comprehensive duplex examination protocol is critical.
- ▪
Knowledge of possible diseases/lesions potentially within the upper extremity venous vasculature, and how to maximize their recognition, is critical.
Venous Anatomy of the Upper Extremity
The veins of the neck, which drain blood from the face and head, consist of the anterior jugular vein, the posterior external jugular vein, and the external jugular and internal jugular veins. However, only the internal and the external jugular veins are clearly seen on a typical duplex scan of the neck.
The external jugular vein drains blood primarily from the scalp and face. It contains two valves in the lower portion and runs superficially in the neck parallel to the posterior border of the sternomastoid muscle to terminate in the subclavian vein. No artery accompanies the external jugular vein. The external jugular vein’s size (in the absence of disease) varies inversely in size with that of its internal jugular vein.
The internal jugular vein receives blood from the deep structures of the neck and the brain. It contains two valves, which may or may not prevent regurgitation, 2.5 cm above its terminus. The internal jugular vein runs down in the neck lateral, first to the internal carotid and then the common carotid artery. On the right side, the internal jugular vein crosses the first segment of the subclavian artery and joins the subclavian vein to form the right innominate vein.
The left internal jugular vein, which is usually smaller in caliber than the right internal jugular vein, crosses the common carotid artery before joining the left subclavian vein to form the left innominate vein, which then crosses the innominate artery to form, together with the right innominate vein, the superior vena cava.
The left and right vertebral veins drain blood from the muscles of the neck.
Several veins from the chest wall (the thoracodorsal vein, lateral thoracic vein, pectoral branch of the thoracoacromial vein, and subscapular vein) join the axillary vein between receiving the brachial and cephalic veins. All these veins may play an important role in supplying collateral flow in the presence of subclavian and axillary vein thrombosis.
A study of 127 arm venograms revealed that as a result of the ability of these chest wall veins to reverse flow if required, axillary vein thrombosis was commonly associated with chest wall collateral pathways. The study has demonstrated that subclavian thrombosis was most often bypassed by neck veins, especially by venous arches that connect the left and right external jugular veins.
There are both deep and superficial dorsal and volar veins of the hand. The superficial veins connect via a network of interlacing branches to eventually form the dorsal venous network on the back of the hand. Digital veins extend from a venous plexus on the volar aspect of the hand. The deep and superficial arterial arches of the hand are flanked by the venae comitantes , which form the superficial and deep venous volar arches.
The cephalic vein, a long superficial vein, runs from the lateral aspect of the wrist and continues up to the shoulder to join the axillary vein just below the clavicle, where it is known as the cephalic arch. An accessory cephalic vein arises variably from segments along the main cephalic vein rejoining more proximally. A common anatomic variant is dominance of the upper arm basilic vein, with one or two diminutive cephalic veins.
The median cubital vein connects the cephalic vein just below the elbow with the basilic vein above the elbow. Occasionally, the median antebrachial vein, which drains the palmar aspect of the hand, courses along the ulnar side of the forearm and drains into the basilic vein. The median antebrachial vein may form the median cubital vein or divide and send a branch each to the cephalic and basilic veins, supplanting the median cubital.
On the medial aspect of the wrist arises the basilic vein, another superficial vessel, which courses up the posterior aspect of the ulnar side of the forearm, receives the median cubital vein slightly above the
- ▪
During scanning of the subclavian vein, have the patient take a “sniff” breath to collapse the vein, because manual compression of the vein by the transducer is not possible due to the overlying clavicle.
- ▪
Scan the subclavian and innominate vein from the head of patient because this affords better opportunity for maximum downward angulation and maneuverability of the transducer.
- ▪
When scanning the axillary vein within the axilla, raise the patient’s arm and rest it on the bed at 90 degrees to the body, so that the vein can be followed along its course into the subclavian segment.
- ▪
To establish the location of the proximal subclavian vein on either side, it is useful to scan down from the internal jugular vein and slide into the confluence with the innominate vein, on both sides.
- ▪
When vein mapping before upper extremity arteriovenous fistula creation, consider placing the patient in a steep reverse Trendelenburg (head up) to pool blood in the forearm veins and distend the veins—and in the supine position to scan the subclavian and axillary veins.
- ▪
Use sufficient gel to enable the transducer probe to be offset from the skin to avoid compression of such veins, so that their measurements are true.
The radial and ulnar veins are the venae comitantes of the arteries in the forearm, with the radial vein usually the smaller of the two. These are the continuation of the deep and superficial volar arches, uniting at the elbow to form the brachial veins.
The deep veins of the forearm anastomose freely with both each other and with the superficial veins.
Duplex Evaluation of the Upper Extremity Veins
Purpose
- □
To demonstrate the presence or absence of partial or complete venous obstruction caused by either venous thrombosis or extrinsic compression
- □
To identify other abnormalities recognizable by ultrasound that may be related to the patient’s symptoms (e.g., enlarged and ± compressive lymph nodes, abnormal fluid collection such as a hematoma or abscess, or an abnormal ± compressive solid mass)
Common Indications and Contraindications
Indications
- □
Arm swelling
- □
Arm redness
- □
Palpable cord
Contraindications
- □
Presence of wound dressings
- □
Open wounds
Equipment
- □
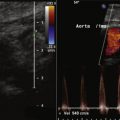
Color duplex imaging system
- □
Higher frequency (e.g., 5- to 17-Hz) linear transducer for superficial imaging
- □
Medium frequency (e.g., 3- to 9-Hz) linear transducer for deeper imaging
- □
Lower frequency (e.g., 2- to 5-Hz) sector/curved array transducer for deep coupling gel
- □
Digital reporting
Procedure
- □
Explain procedure to the patient and answer any questions.
- □
Obtain and document applicable patient history on appropriate forms.
- □
Verify that the procedure requested correlates with the patient’s symptoms.
- □
Obtain an appropriate history. Consider the following questions:
- •
Is there a history of deep vein thrombosis (DVT)?
- •
Is there a history of peripheral or central venous line insertion or of pacemaker or ICD insertion?
- •
Is there a history of trauma?
- •
Is there a recognized thrombophilia?
- •
- □
Perform a limited physical examination of the limbs in question, looking for venous distention, swelling, or a palpable cord.
- □
Review any previous duplex studies available.
- □
Set up the duplex examination:
- •
Select appropriate venous extremity menus and settings.
- •
Select annotation menus that are appropriate for the examination.
- •
- □
Record images.
- □
Complete the technologist’s preliminary report when necessary.
Technique
- □
The patient lies supine with the head flat on a pillow.
- □
The scan is performed from the side and/or top of the bed.
- □
If the patient is symptomatic on one side, the internal jugular vein/subclavian vein on the contralateral side is included.
- □
The patient lies supine with the head flat on a pillow to scan the subclavian and axillary veins and in the reverse Trendelenburg (head raised 45 degrees) to scan the remainder of the arm veins.
- □
As with usual venous scanning technique, transverse views (the order chosen at the technologist’s discretion) are used to follow the anatomy of the venous system distally, and to establish the presence or absence of intraluminal material/noncompressibility. Longitudinal views are used with color Doppler imaging and spectral display of pulsed-wave Doppler interrogation to depict flow, partial obstruction, or complete obstruction.
- □
The following veins are interrogated ( Table 10-1 ):
- •
Internal jugular vein
- •
Subclavian vein
- •
Axillary vein
- •
Brachial vein
- •
Basilic vein
- •
Cephalic vein
- •
Paired veins (radial and ulnar) if the local area is symptomatic
- •