Venous insufficiency is defined as retrograde blood flow in the venous system resulting from incompetence of the venous valves. It is the most common pathologic process affecting the venous system. After the age of 50 years, more than half the human population will have some form of venous insufficiency, which spans a broad spectrum of clinical manifestations ranging from asymptomatic spider veins to symptomatic varicose veins to severe edema with skin inflammation and ulceration ( Figure 50-1 ). Since 2000, the development and refinement of endovenous techniques have revolutionized the treatment of venous insufficiency and have relegated the once gold standard surgical vein stripping to an increasingly historical role.

As is the case with many minimally invasive therapies, achieving durable satisfactory outcomes with modern endovenous treatments depends on accurate diagnostic imaging for preprocedural planning, intraprocedural guidance, and postoperative assessment. Imaging the patient with venous insufficiency is straightforward provided one understands venous anatomy and is familiar with the spectrum of venous disease states and with the appropriate use of available venous imaging modalities. Avoiding the pitfalls of treating these patients requires awareness of the two forces at work in the development of venous insufficiency: valvular incompetence and venous obstruction. Because of the innate variability of the venous anatomy and disease patterns among individuals, errors of diagnosis or management typically arise when the operator fails to assess the patient fully clinically, uses poor technique, or fails to consider possible involvement of more remote venous structures.
This chapter reviews venous anatomy, basic physiology and pathophysiology of venous insufficiency, and the current role of imaging in the evaluation and treatment of the patient with venous insufficiency.
Venous Anatomy
The two venous systems in the lower extremity work concordantly to conduct venous return to the central circulation. The deep venous system consists of a set of large-capacitance veins in the core of the limb. Deep venous components include the following: the paired peroneal, anterior tibial, and posterior tibial veins of the calf; the medial, lateral, and intergemellar (gastrocnemius) and soleal veins; the popliteal, femoral, and deep femoral veins; and the common femoral, external iliac, internal iliac, and common iliac veins of the pelvis. Venous drainage pathways out of the pelvis include the inferior vena cava, retroperitoneal ascending lumbar venous plexus, and gonadal veins.
The superficial venous system is a smaller dermal and subcutaneous network whose components include the great saphenous vein (GSV) and small saphenous vein (SSV), anterior and posterior accessory GSVs, cranial extension of the SSV and intersaphenous vein (vein of Giacomini), and superior accessory GSV. The inferior epigastric veins and external pudendal veins are the most cephalad components of the superficial system. The deep and superficial veins of the lower extremity communicate through up to150 valved perforator veins that normally conduct venous blood in a superficial to deep direction. Historically, lower extremity venous nomenclature was notably inconsistent and confusing. Therefore, in 2001, an international interdisciplinary consensus committee convened in Italy, and the result was the publication of a consensus document that defined the currently accepted nomenclature for lower extremity veins.
Venous Physiology
Both superficial and deep venous systems function to collect the venous blood from the leg to the central circulation. Normally, the deep venous system dominates this process, by carrying 90% of the venous drainage load, compared with the 10% transported by the superficial veins. In the setting of deep venous dysfunction, this ratio shifts, and the superficial veins become the primary collateral drainage pathway. In contrast to the arterial circulation that maintains forward blood flow through an arterial pressure head, venous blood flow is propelled through the veins in the antegrade direction by external compression of the veins by the surrounding musculature (the calf and thigh muscular pumps), as well as by cyclic variations in intraabdominal pressure from respiratory motion. Contraction of the muscular pumps results in forward flow of the blood column, whereas one-way valves prevent retrograde reflux. When the muscular pump relaxes and the veins expand again, intravascular pressure in the deep veins decreases, resulting in a pressure gradient across the perforator vein system that promotes blood flowing from higher to lower pressure in the superficial to deep direction. Valves in the perforator veins prevent reflux of blood from the deep to superficial system during the contraction cycle of the pump. A schematic representation of venous flow dynamics is presented in Figure 50-2 .

Venous Pathophysiology
Development of venous valvular insufficiency is a multifactorial process likely involving genetic predisposition compounded by environmental and lifestyle factors. Secondary venous insufficiency is generally presumed to result from postthrombotic valve destruction, compounded by postthrombotic obstruction to flow that promotes a state of chronic venous hypertension. In contrast, primary venous insufficiency likely results from an intrinsic structural derangement of the vein wall, rather than from valve leaflet damage. Compared with normal veins, primary varicose veins histologically demonstrate proportionally decreased muscle components secondary to increased wall infiltration by collagenous tissue. The abnormal collagen deposits are distributed in a nonuniform pattern and act to separate and disrupt the muscular grid of the vein wall. This process, in turn, results in discontinuous segments of dilatation, wall thinning (blow outs), and secondary expansion of the valve annuli that lead to valvular incompetence.
The mechanism by which venous hypertension incites inflammation and ulceration is a complex process not fully understood, but it seems to involve extravasation of erythrocytes and macromolecules that incite an inflammatory cascade in the dermal perivascular tissues. One theory postulates that venous hypertension causes increase capillary pore size, with resulting extravasation of erythrocytes and fibrinogen and α 2 -macroglobulin into the dermal pericapillary extracellular matrix. This extravasated fibrinogen organizes into fibrin cuff around the capillaries and impairs nutrient and oxygen exchange. White blood cells have also been shown to accumulate in the setting of venous hypertension, and another theory suggests that inflammatory cytokines from red blood cell degradation promote leukocyte accumulation in the capillaries. This process, in turn, results in increased perivascular resistance and upregulation of inflammatory cytokine and proteolytic enzyme release, with consequent tissue damage, inflammation, and ulceration. Reduction of the venous hypertension by leg elevation, compression therapy, and correction of the refluxing circuit reverses this process and promotes healing.
Classification of Chronic Venous Insufficiency
Venous insufficiency may be classified by location as deep, superficial, or perforator reflux. The term axial reflux, applicable to either superficial (e.g., saphenous veins) or deep veins, refers to a continuous reflux column from the common femoral vein level to the knee, as opposed to segmental reflux, which is limited to a short section of vein. Venous insufficiency can also be classified broadly by presumed origin as either primary (developing de novo without an external inciting event) or secondary (from postthrombotic valve damage or venous obstruction). Because the deep and superficial venous structures work in a coordinated and compensatory fashion, prolonged reflux in one part of the system may, over time, overload and incite reflux in other venous structures.
The CEAP classification stratifies venous disorders on the zbasis of four parameters: clinical, etiology, anatomy, and pathophysiology. The clinical groupings range from no evidence of disease (C 0 ) through the spectrum of physical signs of venous insufficiency: telangiectasia or reticular veins (C 1 ), varicose veins (C 2 ), edema (C 3 ), skin changes such as lipodermatosclerosis (C 4 ), healed ulcer (C 5 ), and active ulcer (C 6 ). The etiology is classified as primary (E p ), congenital (E c ), or secondary (E s ). Anatomically, venous disease is divided into superficial (A s ), deep (A d ), and involving perforators (A p ). Pathophysiologically, venous disease is described as the result of reflux (P r ), obstruction (P o ), or both.
Pelvic congestion syndrome (PCS) is a distinct category of venous insufficiency involving the gonadal veins and internal iliac veins. It may occur either alone or in combination with lower extremity venous insufficiency resulting from transmission of venous reflux to the saphenofemoral junction through the external pudendal collateral veins. As is the case with varicose veins elsewhere, pelvic varicosities can result from primary valvular insufficiency or secondarily from more central outflow obstruction. The clinical presentation of PCS includes chronic pelvic pain (CPP) or pressure, which is typically worse when the patient is upright or sitting and relieved by recumbency, dyspareunia and postcoital discomfort, and the presence of vulvar, buttock, or proximal thigh varicosities. An example of thigh varicosities characteristic of PCS is presented in Figure 50-3 .

Imaging of Venous Insufficiency
Duplex Ultrasound
Duplex ultrasound has emerged as the preferred initial imaging modality for evaluation of infrainguinal venous insufficiency, and it provides excellent anatomic detail, as well as localization and quantification of reflux. The study is best performed with a 7.5- to 13.5-MHz linear array transducer, with an ultrasound unit capable of grayscale imaging with both color and spectral Doppler interrogation.
Specific goals of the examination include the following:
- 1.
Defining anatomy, position, and competence of saphenous junctions
- 2.
Assessing the diameter and competence of superficial venous components including the GSV, accessory GSVs, SSV, major tributary branches, and perforators
- 3.
Mapping all major varicosities to their originating source of reflux
- 4.
Confirming status of the deep venous system including assessment for presence of reflux and exclusion of congenital absence, hypoplasia, or thrombotic occlusion of the deep veins
The duplex ultrasound venous reflux examination has two components: a supine examination using both grayscale scanning with dynamic compression and Doppler flow to rule out acute or chronic deep venous thrombus, followed by a reflux examination with pulse wave or color Doppler interrogation of the superficial and deep veins with the patient in the upright position. For the reflux study, the patient is optimally standing with the leg of interest abducted slightly at the hip and with the foot resting fully on the ground but with the weight shifted to the contralateral leg. Calf perforator veins are most easily evaluated with the patient seated on the examining table with the lower leg in a relaxed dependent position. The ultrasound reflux examination includes diameter measurements serially along the length of the GSV and SSV and major accessory saphenous branches, with spectral Doppler assessment for reflux at each point of measurement. Reflux can be elicited by the Valsalva maneuver or by calf compression and release maneuvers.
Figure 50-4 illustrates the typical appearance of a spectral Doppler reflux waveform. The duration of retrograde flow is known as the passive valve closure time and is one quantitative parameter for assessing reflux. Abnormal reflux is defined as follows: greater than 1-second valve closure time at the common femoral, femoral, and popliteal veins; greater than 0.5 seconds for the deep femoral, saphenous, and deep calf veins; and greater than 0.35 seconds for perforator veins. However, the duration of reflux alone does not necessarily correlate with the severity of reflux. A patient with mild venous reflux may have a protracted valve closure time with low-amplitude spectral tracing, whereas a patient with severely incompetent valves may have a relative short duration of reflux of high amplitude as the bolus of blood refluxes across a severely incompetent valve.

The GSV and SSV travel in the saphenous space, which is demarcated by superficial and deep fascial layers that are readily visible sonographically. In cross section, the saphenous veins in the saphenous space have an “Egyptian eye” appearance ( Fig. 50-5 ). When a saphenous vein or a branch passes through the superficial fascia, it becomes a tributary vein.

Potential Pitfalls
- 1.
Failure to stand the patient upright for the reflux examination. The duplex ultrasound examination for venous reflux must be performed with the patient in the upright position to maximize the gravitational effect on the blood column and the pressure gradient across the venous valves and too minimize the likelihood of a false-negative result. No pressure gradient exists in a horizontal vein in the supine position, so one cannot reliably assess the competence of the valves. Varicosities are also engorged in the upright position, thus facilitating visual assessment of disease distribution. To the experienced clinician, the pattern of varicose vein distribution often predicts the source of reflux, but it cannot be reliably assessed when the patient is supine and the veins are flat.
- 2.
Failure to adjust the angle of insonation. Veins are typically branching and often serpiginous structures that change direction of flow as the course of the vessel changes. As the examiner interrogates for reflux along the course of a vein, it is technically important to adjust the angle of insonation constantly to 60 degrees or less to avoid loss of Doppler shift detection. Failure to do so will result in false-negative readings and underdetection of reflux.
- 3.
Failure to trace the major varicosities to their source individually. Venous anatomy is highly variable, so for accurate treatment planning, simply documenting reflux in the saphenous veins is inadequate. All major varicosities of clinical concern should be interrogated sonographically until the exact origin of the reflux is identified. For example, an incompetent midthigh hunterian perforator may give rise to a midthigh varicose vein pattern resembling one resulting from GSV reflux. Thorough duplex examination is especially useful in patients with varicose vein recurrence following earlier vein treatments because the pattern of neovein formation is unpredictable and variable from patient to patient.
Magnetic Resonance Venography and Computed Tomography Venography
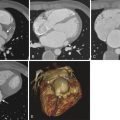
Duplex ultrasound is technically limited for assessment of the calf veins and central pelvic veins, and, in certain situations, additional evaluation by computed tomography venography (CTV), magnetic resonance venography (MRV), or conventional contrast venography may be required. This is especially important in the setting of earlier deep venous thrombosis (DVT) because with obstruction of the deep venous system, the superficial veins become the primary drainage pathway of the lower limb. Removal or ablation of superficial veins is potentially contraindicated and clinically detrimental to these patients. Contrast-enhanced CTV and MRV provide excellent visual resolution of pelvic venous structures, as well as directional flow information, especially with time-resolved imaging of contrast kinetics (TRICKS) MRV sequencing. These imaging modalities are especially helpful in cases of suspected PCS. CTV and MRV also aid in the detection of venous obstruction resulting from extrinsic compression, which can be either benign or malignant.
Two examples of benign extrinsic compression resulting in venous hypertension and reflux include May-Thurner syndrome in which compression of the left common iliac vein by the right common iliac artery results in left lower extremity venous outflow obstruction ( Fig. 50-6 ), and nutcracker syndrome in which compression of the left central renal vein occurs between the superior mesenteric artery and aorta resulting in left renal venous congestion and decompression through gonadal and collateral veins.