Chapter 10 Vitreoretinal Diseases
Introduction
Vitreoretinal diseases are the most common indication for ultrasonographic imaging of the posterior segment. Although most conditions of the posterior segment can be directly viewed, in situations where there is media opacity, for example due to vitreous hemorrhage, echography allows for evaluation of the vitreous, retina, and choroid that would otherwise be impossible.1,2 Using ultrasonography it is possible to identify, evaluate, and follow up a large number of posterior segment conditions such as retinal tears,3,4 vitreous and retinal detachments,5–8 retinoschisis,9 retinal pigment epithelium (RPE) detachment,10 subretinal hemorrhage,11 and eccentric disciform lesions.12
Methods of ultrasonographic evaluation of the posterior segment are described elsewhere (Chapter 3). It is imperative to conduct a thorough examination of all the quadrants to avoid missing any pathology, and to evaluate the vitreous body, posterior hyaloid, subvitreal space, retina, choroid, sclera, optic disc, and macular region.
Vitreous
Vitreous hemorrhage
The vitreous is an avascular structure. Vitreous hemorrhage (VH) occurs by the extravasation of blood into the space limited anteriorly by the posterior lens capsule, posteriorly by the internal limiting membrane and laterally by the ciliary body and lens zonular fibers. VH can be caused by bleeding from normal, diseased or abnormal new retinal vessels, traumatic insult or extension of hemorrhage from any other source. The incidence of VH in the general population is seven cases per 100 000 per year.13 The most common causes of VH vary based on the population studied, with the two most common causes being posterior vitreous detachment (PVD) with or without retinal tear and proliferative diabetic retinopathy, followed by ocular trauma and neovascularization secondary to retinal vein occlusion.14–17
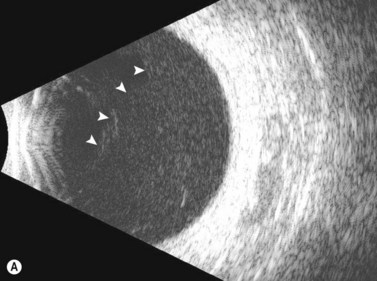
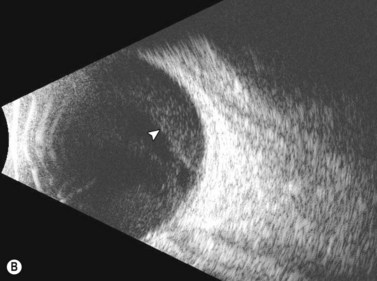
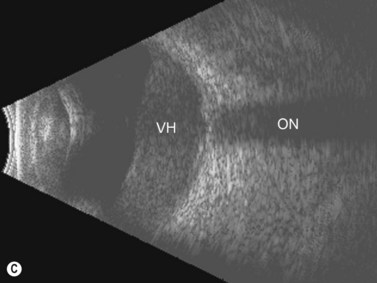
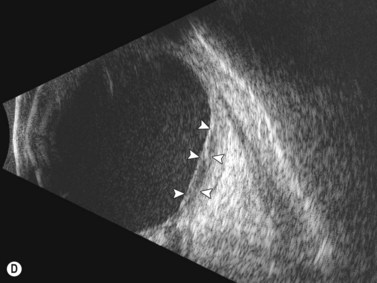
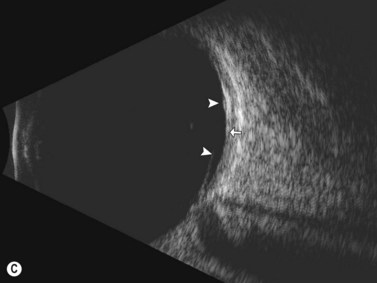
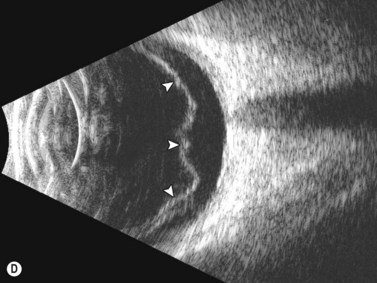
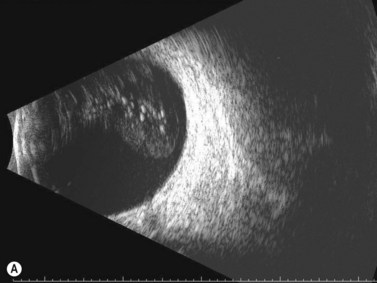
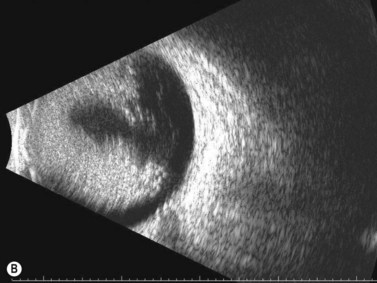
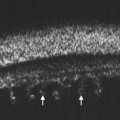
Dynamic A- and B-scan ultrasonographic examinations should be performed to rule out retinal tears, detachment, or other intraocular pathology as the source of vitreous hemorrhage.![]() See Clip 10.1 A fresh vitreous hemorrhage appears as diffuse opacities of low to medium reflectivity on B-scan, with multiple low intensity spikes on A-scan (Figure 10.1A).18 As the blood organizes, it forms pseudomembranous surfaces on B-scan, corresponding to slightly higher intensity spikes on A-scan (Figure 10.1B). Signal intensity on both A- and B-scan directly correlates with the density of the hemorrhage (Figure 10.1C). Layering of blood inferiorly results in very high reflectivity on B-scan and in a static exam may be mistaken for a retinal detachment (RD) (Figure 10.1D).
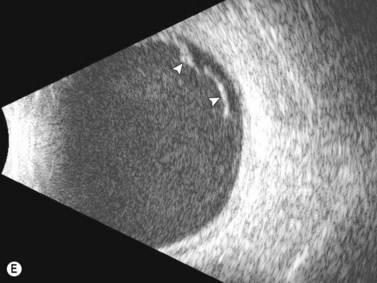
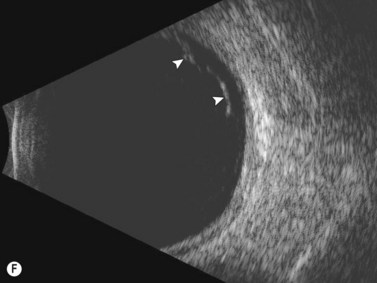
See Clip 10.1 A fresh vitreous hemorrhage appears as diffuse opacities of low to medium reflectivity on B-scan, with multiple low intensity spikes on A-scan (Figure 10.1A).18 As the blood organizes, it forms pseudomembranous surfaces on B-scan, corresponding to slightly higher intensity spikes on A-scan (Figure 10.1B). Signal intensity on both A- and B-scan directly correlates with the density of the hemorrhage (Figure 10.1C). Layering of blood inferiorly results in very high reflectivity on B-scan and in a static exam may be mistaken for a retinal detachment (RD) (Figure 10.1D).![]() See Clip 10.2 In a vitrectomized eye, blood can remain in a liquefied state and often requires the use of high gain settings to visualize the hemorrhage (Figure 10.1E and F).
See Clip 10.2 In a vitrectomized eye, blood can remain in a liquefied state and often requires the use of high gain settings to visualize the hemorrhage (Figure 10.1E and F).
If PVD is absent, a retinal tear or rhegmatogenous retinal detachment (RD) is unlikely and therefore, other causes of the VH must be explored. If a PVD is present and RD is not observed, PVD is most likely not the cause of the VH. However, a small anterior retinal detachment may not be detected by an inexperienced ultrasonographer.19 In addition, presence of a PVD does not exclude other causes of the VH since the PVD may have been present prior to the VH.
Posterior vitreous detachment
Posterior vitreous detachment is a common degenerative process of the vitreous in which the vitreous gel loses its attachment to the internal limiting membrane. The causative factor for PVD can vary, but is most commonly senile degeneration of the vitreous gel. The vitreous is very strongly attached (vitreous base) in a band extending 360° around the anterior limits of the retina (ora serrata) and only weakly adherent to the macula and optic disc; thus the site of detachment is usually located in the posterior pole.20 In nearly half of patients the PVD is incomplete and some portions of the vitreous remain attached to and can exert traction on the retina.21 Retinal tears often occur just posterior to the vitreous base, due to traction placed on the retina as the vitreous pulls away from the retina.
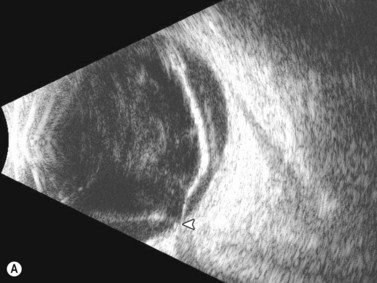
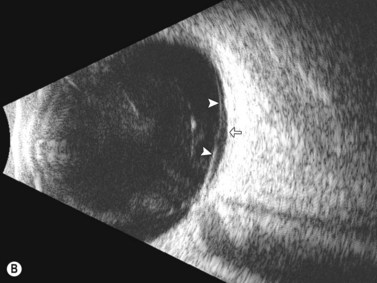
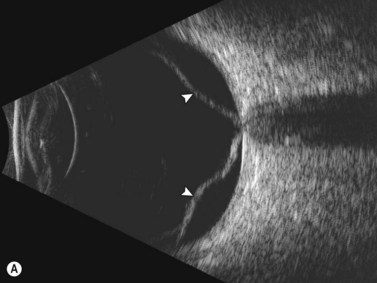
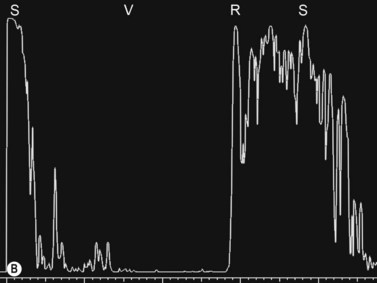
Ultrasonographically, PVD appears as a thin, smooth membrane that may retain its attachment to the retina at the site of retinal tears, areas of neovascularization, optic disc, and/or at the vitreous base. A PVD can mimic a RD on ultrasonography when the posterior hyaloid remains attached to the optic disc; however, there are specific clues that can be used to differentiate these two entities (Figure 10.2A, Table 10.1). A PVD demonstrates significant movement and after movement on dynamic B-scan.![]() See Clip 10.3 In cases of inflammation and trauma, the PVD may be much less mobile. In this situation, it is usually possible to differentiate PVD from a RD based on the reflectivity profiles of the tissues. In the absence of dense vitreous hemorrhage, a PVD appears as a low to medium reflective membrane on both A and B-scan, while a retinal detachment is always highly reflective. A PVD is visible only at high gain settings whereas the retina is visible at low and high gain settings (Figure 10.2B, C). Layering of blood along the surface of a PVD may result in a thickened appearance on B-scan and very high reflectivity on A-scan (Figure 10.2D). Therefore, to differentiate a hemorrhagic PVD from a RD, it is necessary to examine different portions of the membrane for a decrease in reflectivity suggestive of a vitreous membrane. Posteriorly, both the retina and vitreous membranes can appear as highly reflective structures. Anteriorly, however, the retina is much more highly reflective than vitreous membranes.22 In patients with vitreous hemorrhage secondary to proliferative vitreoretinopathy (PVR), localization of focal traction on the retina can be the differential diagnostic indicator.
See Clip 10.3 In cases of inflammation and trauma, the PVD may be much less mobile. In this situation, it is usually possible to differentiate PVD from a RD based on the reflectivity profiles of the tissues. In the absence of dense vitreous hemorrhage, a PVD appears as a low to medium reflective membrane on both A and B-scan, while a retinal detachment is always highly reflective. A PVD is visible only at high gain settings whereas the retina is visible at low and high gain settings (Figure 10.2B, C). Layering of blood along the surface of a PVD may result in a thickened appearance on B-scan and very high reflectivity on A-scan (Figure 10.2D). Therefore, to differentiate a hemorrhagic PVD from a RD, it is necessary to examine different portions of the membrane for a decrease in reflectivity suggestive of a vitreous membrane. Posteriorly, both the retina and vitreous membranes can appear as highly reflective structures. Anteriorly, however, the retina is much more highly reflective than vitreous membranes.22 In patients with vitreous hemorrhage secondary to proliferative vitreoretinopathy (PVR), localization of focal traction on the retina can be the differential diagnostic indicator.
Table 10.1 Ultrasonographic differentiating features between posterior vitreous detachment and retinal detachment.
| Feature | Posterior vitreous detachment | Retinal detachment |
|---|---|---|
| Echogenicity | Low–medium echogenicity | High echogenicity |
| Change with gain (dB) | Disappears with low gain | Visible with low gain |
| Mobility | High mobility | Low mobility |
| Optic disc attachment | Present or absent | Always present |
Asteroid hyalosis
Asteroid hyalosis (AH) is an uncommon, predominantly unilateral, condition that rises in prevalence with age, although a link to systemic diseases has been suggested.23–25 Clinically, it appears as multiple small spheres scattered throughout the vitreous consisting of condensations of calcium and phospholipid. Most patients with AH are asymptomatic. On A-scan, asteroid hyalosis appears as medium to highly reflective spikes that move with the vitreous. There have been a few reports of falsely shortened axial length measurements on A-scan in eyes with AH, but the majority of eyes will show no change in axial length measurement due to AH.26–28 On B-scan, the asteroid bodies appear as both diffuse and focal point-like highly reflective sources with an area of clear vitreous between the posterior border of the asteroid bodies and the retina (Figure 10.3).
Retinal detachment
Retinal detachments occur when the neurosensory retina separates from the underlying retinal pigment epithelium. Retinal detachments are divided into four main types: rhegmatogenous, tractional, exudative (serous), and combined tractional/rhegmatogenous retinal detachment.29
Rhegmatogenous retinal detachment
Rhegmatogenous retinal detachment is the most common type of detachment and is characterized by the presence of a full-thickness retinal tear. There are three prerequisites for the development of rhegmatogenous retinal detachment: liquefaction of the vitreous gel, tractional forces to produce a retinal tear, and a retinal tear that allows fluid access from the liquefied vitreous into the subretinal space.29,30 The annual incidence of rhegmatogenous retinal detachments in the general population of the United States is about 12 cases per 100 000 people (0.01% annual risk). There are about 36 000 cases annually, with anatomic surgical success rates up to 95%.31–33 The major risk factors are high myopia, trauma, cataract surgery, ocular infections, lattice degeneration, and glaucoma.
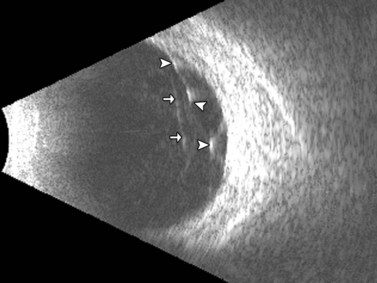
In the setting of media opacity such as a vitreous hemorrhage, differentiating a PVD from a retinal detachment can sometimes be challenging (Table 10.1). Retinal detachments can present with variable mobility, but will always be less mobile than vitreous membranes.34 Retinal detachments are highly reflective with a thickened, rope-like appearance and always have optic disc attachment, while a PVD can retain attachment to the optic disc or be completely detached (Figure 10.4A). On A-scan, the retina demonstrates close to 100% reflectivity (Figure 10.4B).
Tractional retinal detachment
Tractional retinal detachments (TRD) are the second most common type of retinal detachment.32 TRDs can occur due to PVR, penetrating trauma, retinopathy of prematurity, and severe diabetic retinopathy. TRDs occur due to vitreoretinal adhesions that cause mechanical separation of the retina from the underlying RPE causing a retinal detachment. The detachment has a tent-like configuration that does not extend to the ora serrata. On B-scan TRDs demonstrate reduced mobility compared to rhegmatogenous retinal detachments due to the traction placed on the retina (Figure 10.5).![]() See Clip 10.435
See Clip 10.435