- •
CMR can detect myocardial ischemia using exercise and pharmacologic stressors with accuracy comparable to nuclear and echocardiography.
- •
Accuracy of CMR wall motion stress testing for ischemia may be limited in patients with left ventricular hypertrophy, resting wall motion abnormalities, and severely reduced resting left ventricular systolic function. Addition of stress and rest perfusion protocols to wall motion assessment may improve the accuracy in these clinical situations.
- •
The prognostic value of CMR pharmacologic wall motion stress testing is well established.
- •
Further studies are needed to validate the prognostic implications of exercise wall motion CMR stress testing.
- •
Additional studies are needed to elucidate the diagnostic and prognostic values of combined wall motion–perfusion CMR stress testing.
- •
Myocardial scar and/or infarct assessment by late-gadolinium enhancement imaging from combined wall motion–perfusion CMR stress testing may provide additional prognostic implications.
- •
CMR wall motion stress testing is a suitable alternative for ischemia and viability assessments in patients with contraindications to gadolinium-based CMR perfusion stress testing as in moderate to severe kidney disease.
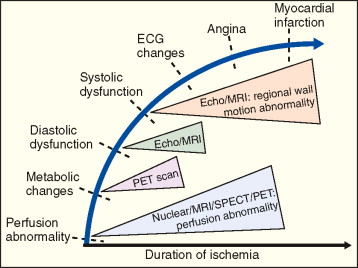
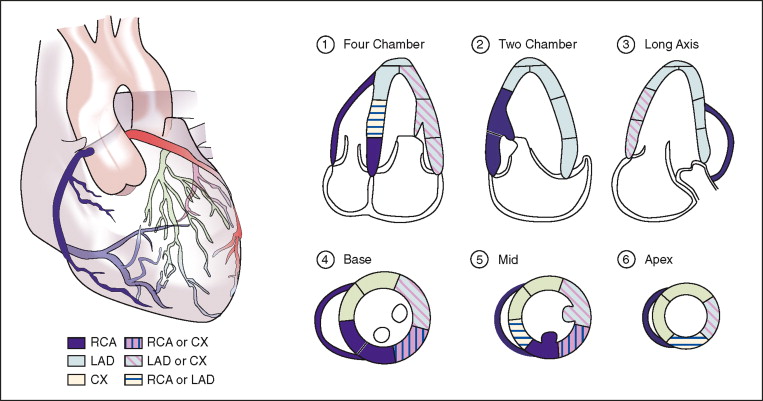
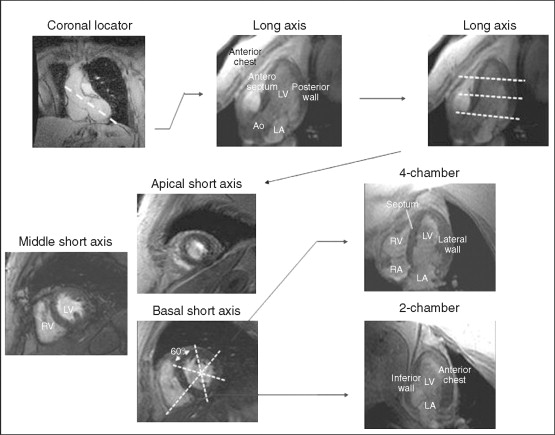
Cardiovascular magnetic resonance (CMR) has emerged as a viable alternate method of evaluating for myocardial ischemia, by the detection of stress-induced systolic wall motion abnormalities ( Figure 18-1 ). Standardized myocardial nomenclature is used for segment and vascular territory identification ( Figures 18-2 to 18-4 ).
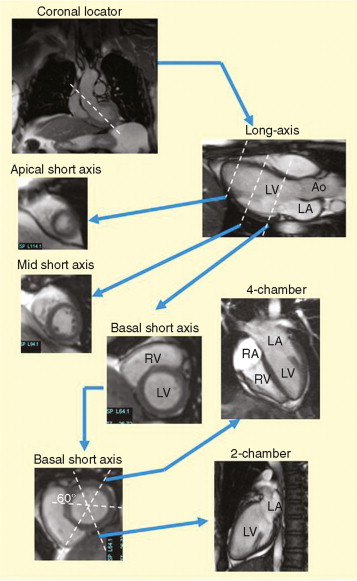
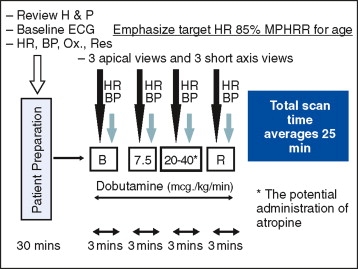
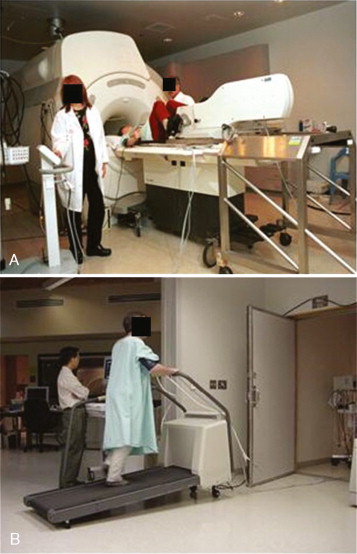
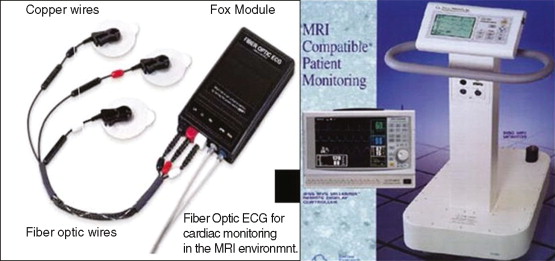
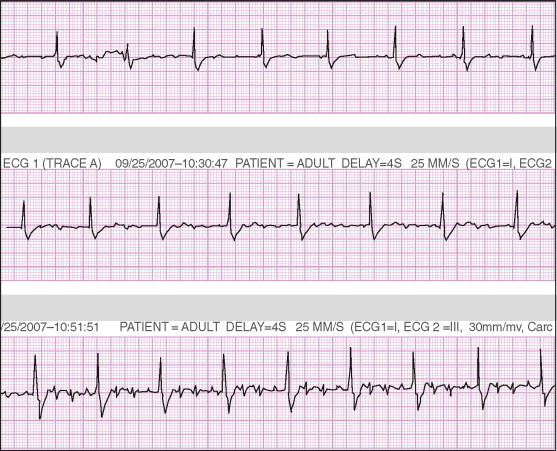
CMR stressors used for wall motion stress tests include exercise, and pharmacologic agents (i.e., dobutamine and vasodilators such as adenosine and dipyridamole). Dobutamine ± atropine is the most common stressor used for assessment of inducible wall motion abnormalities ( Figure 18-5 ). Performance of wall motion stress CMR requires standardized protocol, real-time display of wall motion, and safety protocols ( Figures 18-6 to 18-9 ). Intraprocedural ECG tracing is mainly used for rhythm monitoring and not ischemic ST changes because of distortion of segments by CMR ( Figure 18-10 ).

This chapter presents case studies of clinically available CMR methodologies using wall motion for the detection of myocardial ischemia.
A 63-year-old woman with end-stage renal disease (ESRD) secondary to diabetic nephropathy and on maintenance hemodialysis presented for preoperative evaluation for renal transplantation. She underwent dobutamine stress cardiac magnetic resonance (DSCMR) for further preoperative cardiovascular risk stratification.
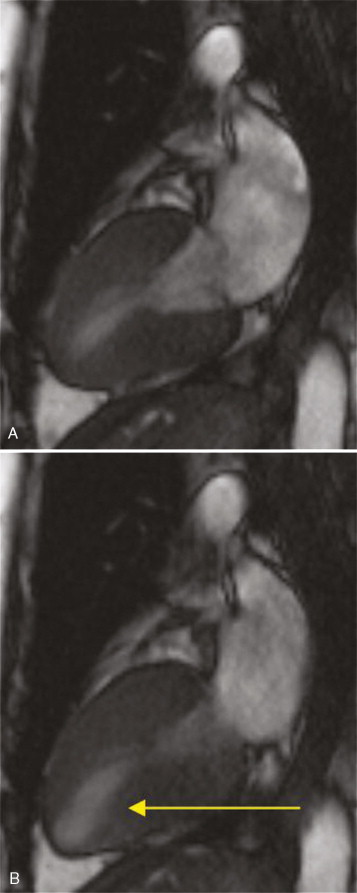
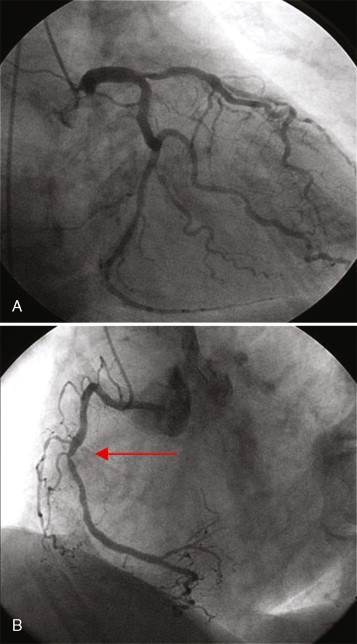
DSCMR revealed evidence of inducible ischemia in the apical inferior and inferolateral walls ( Figure 18-11 ). A cardiac catheterization demonstrated significant three-vessel disease ( Figure 18-12 ), necessitating a successful three-vessel CABG. She subsequently underwent a successful kidney transplant with an uneventful postoperative clinical course.
Comments
Wall motion stress test by CMR is considered an appropriate test for risk-stratifying patients with chest pain syndromes with intermediate pretest probability of coronary artery disease. Recent ACC/AHA guidelines on preoperative care before noncardiac surgery have also recommended stress test risk stratification among patients with at least three clinical risk factors (ischemic heart disease, compensated or prior heart failure, cerebrovascular disease, diabetes mellitus, renal insufficiency), poor functional capacity (less than 4 METs), and those undergoing vascular surgery.
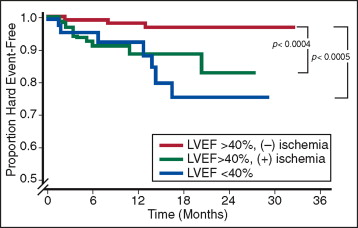
DSCMR provides diagnostic accuracy and prognostic significance comparable with established tools such as nuclear imaging and echocardiography ( Figure 18-13 ). DSCMR is also suitable in patients with contraindications to vasodilators such as adenosine and dipyridamole or in situations such as ESRD, in which administration of CMR contrast for perfusion is contraindicated.
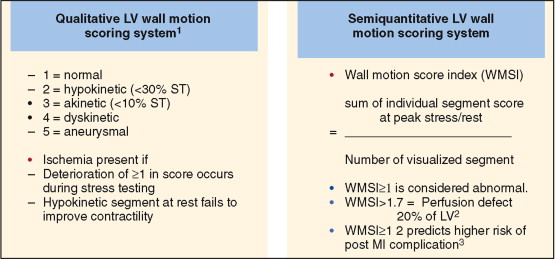
DSCMR has sensitivity and specificity of 83% to 96% and 80% to 87%, respectively, for identifying significant epicardial coronary artery stenoses (=50% luminal stenoses). The interpretation scheme for wall motion stress CMR is similar to stress echocardiography ( Figure 18-14 ).