Hiroshi Yoshioka, MD, PhD
INTRODUCTION
In recent years, magnetic resonance imaging (MRI) has become a very important modality for diagnosing wrist and hand diseases including osteoarthritis, rheumatoid arthritis (RA), occult fracture, avascular necrosis (AVN), ligamentous/tendinous injuries, impaction syndrome, and nerve entrapment syndrome.1,2 MRI is a noninvasive and nonirradiative imaging tool, and can provide high soft tissue contrast resolution. Thin and contiguous slices are needed for adequate MR imaging of the wrist because even the larger ligaments of the wrist are no greater than 1–2 mm thick.3 New MRI techniques such as 3D volume acquisitions on higher magnetic fields improve signal to noise ratios and visualization of wrist structures in detail with a shorter scan time.4
ANATOMY
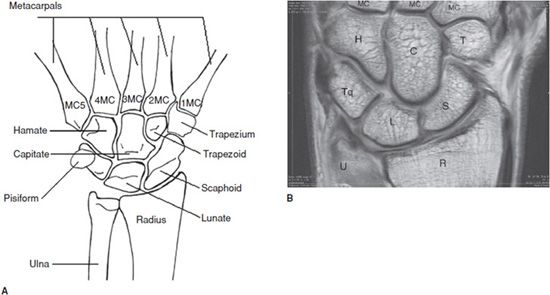
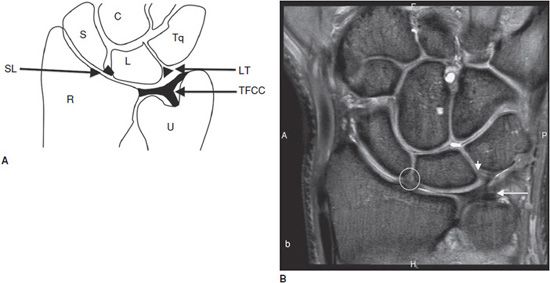
The distal radius and ulna articulate with the proximal row of the carpal bones consisting of the scaphoid, lunate, and triquetrum. The pisiform, a sesamoid bone, is also found in the proximal carpal row and articulates only with the triquetrum. The distal carpal row contains the trapezium, trapezoid, capitate, and hamate, which are articulating with the base of the metacarpal bones and carpal bones of the proximal row (Figure 16-1). The combination of intrinsic and extrinsic ligaments is stabilizing the wrist. Intrinsic wrist ligaments are entirely within the carpus. Extrinsic wrist ligaments have an attachment on the carpus and pass out of the carpus. The strongest ligaments of the wrist are volar extrinsic ligaments, then intrinsic ligaments including the scapholunate (SL) and lunotriquetral (LT) ligaments and the weakest are dorsal extrinsic ligaments. Among these ligaments, the SL and LT ligaments are more important in daily practice since these ligaments are vulnerable to attritional wear. The SL ligament has U shape and the LT ligament has V shape in sagittal plane (Figure 16-2).5–7
Figure 16-1. Wrist anatomy. (A) Schematic drawing and (B) coronal proton density MR image of the wrist show anatomy of carpal bones. U = Ulna, R = Radius, S = Scaphoid, L = Lunate, Tq = Triquetrum, T = Trapezoid, C = Capitate, H = Hamate, MC = Metacarpal bones.
Figure 16-2. Wrist anatomy. (A) Schematic diagram shows triangular fibrocartilage complex (TFCC), scapholunate (SL), and lunotriquetral (LT) ligaments. (B) Coronal proton density with fat saturation MR image of the wrist shows TFCC (long arrow), LT ligament (short arrow) and SL ligament (Circle). U = Ulna, R = Radius, S = scaphoid, L = Lunate, Tq = Triquetrum, C = Capitate.
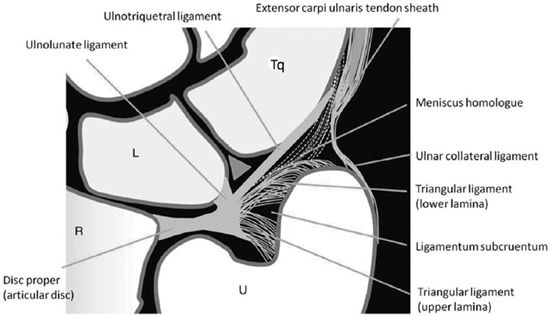
The triangular fibrocartilage complex (TFCC) is located between the ulnar head and the first carpal row (the lunate and the triquetrum). The TFCC has three main roles: (1) stability of the distal radioulnar joint (DRUJ), (2) axial load transmission from the carpus to the ulna, and (3) ulnar-sided carpal stability.8 The TFCC has several components including disc proper, triangular ligament, volar and dorsal radioulnar ligaments, meniscus homologue, ulnolunate ligament, ulnotriquetral ligament, and ulnar collateral ligament (Figure 16-3).6 Given the anatomical complexity of the TFCC, we need to use multiplanar and multisequence MRI for full evaluation. In coronal planes, the disc proper, triangular ligament, meniscus homologue, and ulnotriquetral ligament can be evaluated. In axial planes, the volar and dorsal radioulnar ligaments are better seen.3–4
Figure 16-3. Triangular fibrocartilage complex detailed anatomy. Schematic drawing in coronal plane shows detail of the TFCC components. U = Ulna, R = Radius, Tq = Triquetrum, L = Lunate.
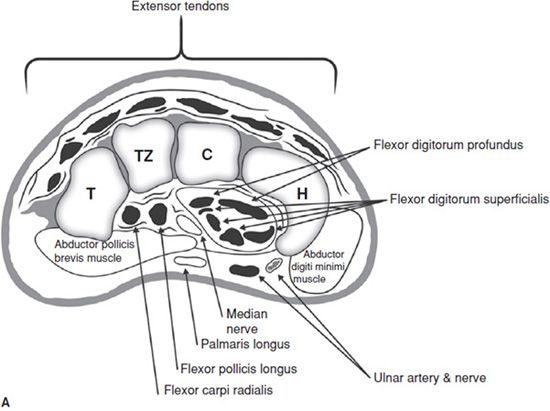
The carpal tunnel is an oval shaped space bounded dorsally, medially, and laterally by the carpal bones, and in volar aspect covered by the flexor retinaculum, also known as the transverse carpal ligament (Figure 16-4). It contains the median nerve, tendons of the flexor digitorum superficialis and profundus tendons, and the flexor pollicis longus tendon. The tendons of both the flexor digitorum superficialis and profundus are lined up side by side in the carpal tunnel. Normal and pathology of the carpal tunnel can be best evaluated in axial sequences.7
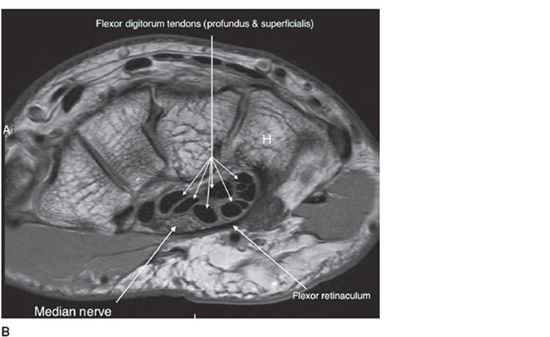
Figure 16-4. Carpel tunnel anatomy. (A) Schematic diagram and (B) corresponding axial fat saturated proton density MR image of the wrist show anatomy of carpal tunnel. H = Hamate, C = Capitate, Tz = Trapezoid, T = Triquetrum.
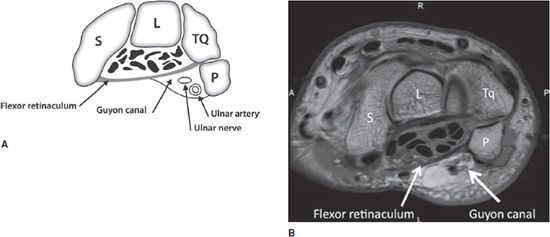
The Guyon canal is a small fibro-osseous, semirigid, triangular tunnel at the medial volar aspect of the wrist and it contains the ulnar nerve, artery, fat, and occasionally veins. The walls of this canal consist of the pisiform medially and the hook of the hamate laterally. The floor is composed mainly of the flexor retinaculum and the origins of the hypothenar muscles and the roof is mainly composed of the pisohamate ligament (Figure 16-5).7,9
Figure 16-5. Guyon canal anatomy. (A) Schematic diagram of Guyon canal with corresponding (B) axial proton density MR image of the wrist shows Guyon canal anatomy. S = Scaphoid, L = Lunate, Tq = Triquetrum, P = Pisiform.
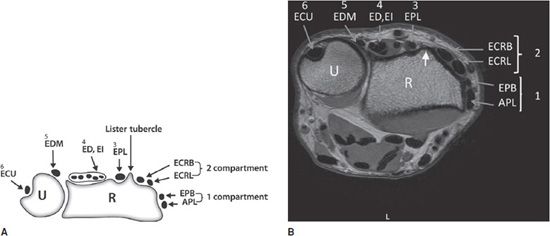
The extensor tendons with synovial sheaths are located in dorsum of the wrist under the superficial dorsal carpal ligament. There are six distinct compartments in dorsum of the wrist (Figure 16-6).5,7
Figure 16-6. Extensor tendon compartment anatomy. (A) Schematic diagram of proximal wrist in axial plane and corresponding (B) axial proton density with fat saturation MR image show the six extensor compartments of the wrist. The Lister tubercle (short arrow in part B) separates the second and third compartment. Compartment 1: abductor pollicis longus (APL) and extensor pollicis brevis (EPB), compartment 2: extensor carpi radialis longus and brevis (ECRL and ECRB), compartment 3: extensor pollicis longus (EPL), compartment 4: extensor digitorum (ED) and extensor indicis (EI), compartment 5: extensor digiti minimi (EDM), and compartment 6: extensor carpi ulnaris (ECU). R = radius, U = Ulna.
PATHOLOGY
 Scaphoid Fracture and Avascular Necrosis
Scaphoid Fracture and Avascular Necrosis
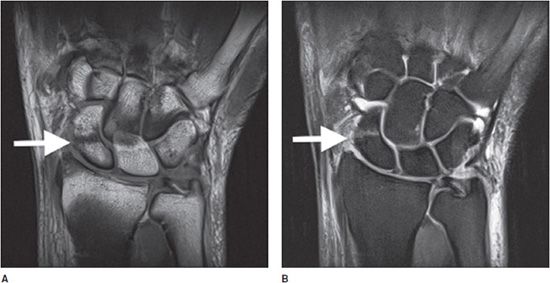
A scaphoid fracture is the most common carpal fracture occurring more in active men. Scaphoid fractures occur in the scaphoid tuberosity, the waist, and the proximal or distal pole. On occasion, a scaphoid fracture is difficult to diagnose on radiograph. MRI of the scaphoid fracture depicts low signal intensity fracture line surrounded by T2 high signal bone marrow edema (Figure 16-7).10 MRI can also detect surrounding soft tissue contusion and hemorrhage. Posttraumatic complications of the scaphoid fracture include AVN and nonunion. The AVN of the proximal scaphoid fracture is known as a frequent complication due to the dedicated vascular anatomy that the main arterial supply of the scaphoid enters through distal half of the bone and there are no vessels entering the proximal scaphoid pole. The AVN demonstrates low T1 and low T2 signal with collapsed proximal fragment due to fibrosis and/or sclerosis. Viability of the proximal fragment in scaphoid nonunion can be better assessed with the use of contrast-enhanced MRI as compared with nonenhanced MRI.11 The lack of bone marrow enhancement usually indicates lack of blood perfusion and therefore ischemia.12
Figure 16-7. Scaphoid fracture. Coronal (A) proton density weighted and (B) fat-suppressed proton density-weighted MR images of the wrist show dark T1 (part A) and bright T2 (part B) line (arrow) through the scaphoid bone consistent with a fracture.
Hyperemic reparative tissue is easy detectable on fat-suppressed T1-weighted images (T1WI) after gadolinium by means of hyperenhancement.
PEARLS
 Kienböck Disease
Kienböck Disease
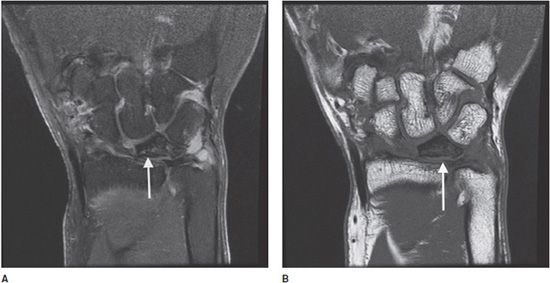
AVN of the lunate is known as Kienböck disease, which is more common in males between ages of 20 and 40. The exact cause of Kienböck disease is not known, but predisposing factors may include repetitive trauma (dominant hand of manual laborers), acute trauma, and negative ulnar variance. Kienböck disease can be classified into four stages. In the first stage, the changes are subtle. However, as disease progresses, the lunate becomes sclerotic and finally ends up with secondary osteoarthritis (stage 4). MRI shows signal changes of the lunate in all stages, but its value is in early detection of AVN on stage 1, where focal or diffuse low signal intensity is seen on T1WI in affected areas of marrow involvement with normal radiograph.8,13 The signal intensity on T2-weighted images (T2WI) varies dependent on stages of edema, fibrosis, or sclerosis (Figure 16-8). A uniform loss of signal intensity in the lunate on T1WI and T2WI is hallmark of AVN on stage 4, where the lunate is severely collapsed and fragmented and secondary osteoarthritic changes are seen in the wrist.
Figure 16-8. Kienböck disease. Coronal proton density with and without fat saturation MR images of the wrist (parts A and B, respectively) show dark signal changes in flattened deformed lunate (arrow) consistent with Kienböck disease (avascular necrosis of the lunate).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree