Jamshid Tehranzadeh, MD
ARTHRITIS
INTRODUCTION
This chapter aims to serve as a basic introduction to the radiographic evaluation of arthritis. There are reference texts and books devoted to the subject, including those from Resnick1 and Brower,2 which serve as excellent references for those readers interested in further study. This chapter is rich in images, focusing on radiographs, with some attention paid to CT and MRI. A brief section on musculoskeletal infection then follows the discussion on arthritis.
 Osteoarthritis
Osteoarthritis
Osteoarthritis is the most common joint disease worldwide, with well over half the elderly population affected. Osteoarthritis is primarily a disease of cartilage, with bony changes representing later sequelae of damaged cartilage. The disease is diagnosed by both radiographic and clinical findings, such as joint pain and stiffness. There are no specific serum bio-markers. Osteoarthritis has traditionally been subdivided into primary and secondary forms based on cause. In primary osteoarthritis, no specific underlying cause for the joint disease is identifiable. When a causative factor can be identified, the term secondary osteoarthritis is used. Any event or disease that causes cartilage loss and destruction can result in secondary osteoarthritis, including trauma or inflammatory arthritides such as rheumatoid arthritis. Often times, the underlying cause in cases of secondary osteoarthritis can be deduced through careful examination for old traumatic deformity or erosions from inflammatory arthritides. Despite the subtype, the radiographic characteristics of asymmetric joint space narrowing, subchondral sclerosis, osteophytosis, and subchondral cyst formation remain the same.
Joint space narrowing, resulting from progressive loss of the articular cartilage, is nonspecific to osteoarthritis but helps classify disease severity. In most osteoarthritic joints, cartilage loss is not uniform, with regions of the joint responsible for weight-bearing or exposed to abnormal forces most significantly narrowed. With progressive cartilage loss, the subchondral bone is exposed to abnormal forces that result in remodeling, manifested as sclerosis radiographically. Subchondral cysts or geodes may form, which are areas of focal subchondral bone resorption. One explanation for the formation of these cysts in osteoarthritis is that as fissures or pits form in the articular cartilage, synovial fluid is extruded through these defects into the subchondral bone, forming a cyst. Subchondral cysts, or geodes, are not unique to osteoarthritis. Other arthropathies that can lead to geodes include rheumatoid arthritis, calcium pyrophosphate deposition disease, and hemophilic arthropathy. Osteophytes form at the margins of degraded articular cartilage and act to increase the surface area and provide stability to a damaged joint. As the disease progresses, the osteophytes increase in size.
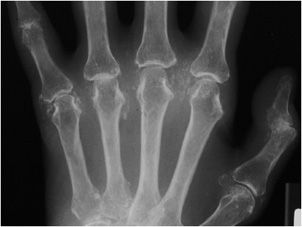
Osteoarthritis of the hand (Figure 6-1) typically involves mostly the distal interphalangeal (DIP) joints and to a lesser extent the proximal interphalangeal (PIP) joints as well as the joints at the base of the thumb (Figure 6-2), including the first carpometacarpal (CMC) joint (so-called trapezium–trapezoid first metacarpal joint), and scaphoid–trapezium–trapezoid (STT) joints. The more proximal joints of the hand and wrist are typically spared. Again, the triad of joint space narrowing, osteophyte formation, and subchondral sclerosis in this distribution should be sought. The physical exam findings of Heberden and Bouchard nodes, which are firm enlargements at the DIP and PIP joints, respectively, correspond to the osteophytes formed at these joints.
Figure 6-1. Osteoarthritis. PA view of the right hand in a 73-year-old female shows osteophyte formation and joint narrowing predominantly at the distal interphalangeal joints with “gull-wing” appearance (arrow).
Figure 6-2. Osteoarthritis. PA view of the left hand in a 65-year-old male shows osteophyte formation, joint space narrowing and subchondral sclerosis (arrows) at the first carpometacarpal joint, a favored site of primary osteoarthritis.
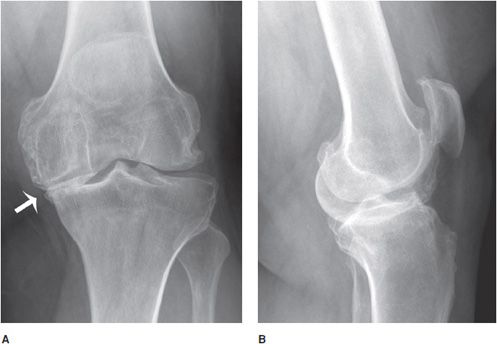
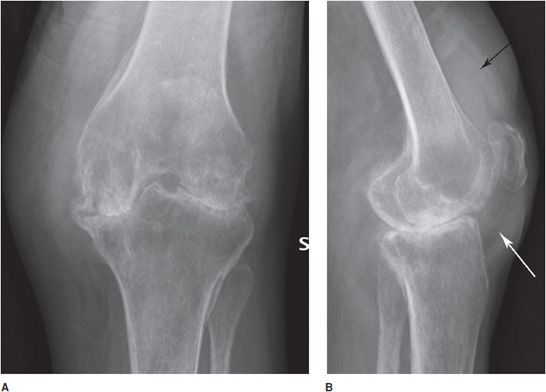
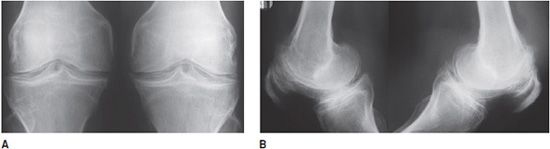
The medial tibiofemoral joint space is typically most severely affected in osteoarthritis of the knee. With progressive disease, there is involvement of the patellofemoral and lateral tibiofemoral joints as well. Non–weight-bearing views often underestimate the severity of joint space narrowing. Accurate quantification of joint space narrowing is best obtained with standing anteroposterior (AP) views (Figure 6-3A,B), or Rosenberg posteroanterior (PA) view of both knees (this view is obtained with slightly flexed knees with 15° of caudal angulation of the X-ray beam). Varus deformity may be evident given the asymmetric narrowing of the medial compartment. The earliest MRI findings include an increased T2 signal in the articular cartilage secondary to increased water content and increased T2 signal in the subchondral bone marrow reflective of edema. Disease progression is manifested by fibrillation and thinning of the cartilage. In severe end-stage disease, there is bone-on-bone articulation with obliteration of the cartilage and menisci. It is not uncommon for a suprapatellar effusion to be evident on lateral radiographs.
Figure 6-3. Osteoarthritis. Standing AP (A) and lateral (B) views of the left knee in a 54-year-old male show osteoarthritis with significant narrowing of the medial aspect of the femorotibial joint due to loss of articular cartilage. The lateral view shows joint effusion with femoropatellar joint narrowing and osteophyte formation.
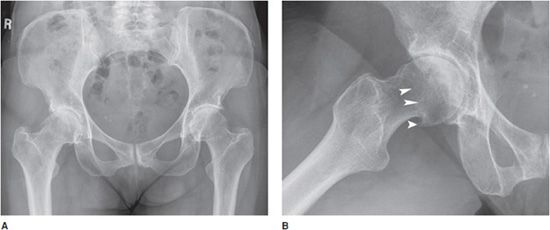
The weight-bearing superior aspect of the hip typically demonstrates the greatest degree of narrowing (Figure 6-4A,B), with superior migration of the femoral head considerably more common than medial migration. Osteophytes are typically seen at the lateral acetabulum. On the frog-leg lateral view of the hip, small osteophytes may be seen as a ring around the border of the articular surface of the femoral neck (“apron osteophytes”). Sclerosis is usually at the roof of the acetabulum and along the subchondral surface of the femoral head.
Figure 6-4. Osteoarthritis. AP (A) and lateral (B) radiographs of the right hip in a 56-year-old female showing osteoarthritis of the right hip with narrowing predominantly at the superolateral aspect of the joint space with marginal and apron osteophytes (arrowheads). Note subchondral sclerosis of the acetabulum and femoral head.
Joint space narrowing is not unique to osteoarthritis, and it is critical to differentiate other causes of joint space narrowing, such as the inflammatory arthritides, from osteoarthritis.3 This distinction may be complicated because as cartilage in the joint space is lost due to any cause, be it trauma or other arthropathy, secondary degenerative or osteoarthritic changes will occur. Thus, in cases where the radiographic appearance or joint distribution of osteoarthritis is atypical, it is important to evaluate for an underlying cause because this may impact treatment and management.
PEARLS
 Erosive Osteoarthritis
Erosive Osteoarthritis
Erosive osteoarthritis is considered a subtype of primary osteoarthritis that affects the hands of females, predominantly during the fifth decade around menopause.4 This entity is unique in that it mixes features seen in osteoarthritis with those of inflammatory arthritis. The joints involved are similar to those in primary osteoarthritis, namely the DIP, PIP, first CMC, and STT joints of the hand (Figure 6-5A,B). The MCP joints may also rarely be involved. The radiographic pattern of erosive osteoarthritis includes centrally located erosive changes. This central erosion differs from the marginal erosions seen in inflammatory arthritides such as rheumatoid or psoriatic arthritis. In the DIP and PIP joints, this pattern of erosion may result in the radiographic finding called the “gull-wing” sign. In addition, coexistent proliferative changes such as osteophyte formation and subchondral sclerosis, typical in erosive osteoarthritis, are unusual in inflammatory arthropathies unless there is superimposed secondary osteoarthritis. Clinically, the involved joints can be inflamed, with palpable synovitis and limited range of motion. Exam findings are similar to rheumatoid arthritis but involving a different distribution of joints. Heberden and Bouchard nodes may be present similar to osteoarthritis; however, erosive osteoarthritis may lead to even greater deformity with subluxation of the interphalangeal (IP) joints creating a “Z-shaped” deformity.4
Figure 6-5. Erosive osteoarthritis. PA (A) and lateral (B) views of the hand in a 80-year-old male show erosive changes of the distal interphalangeal joints with the characteristic “gull-wing” appearance. There is narrowing of the both proximal and distal interphalangeal joints and osteophyte formation. Note erosion (arrowhead).
 Rheumatoid Arthritis
Rheumatoid Arthritis
Rheumatoid arthritis is a symmetric polyarthritis predominantly affecting the small synovial joints, although any synovial joint can be involved. Rheumatoid arthritis is a disease of the synovium. The underlying cause is not known; however, predilection for the disease is impacted by genetic and environmental factors. The prevalence of disease is approximately 1% of adults, with onset typically ranging between 35 and 50 years old. The disease is more common in women, with females affected three times more often than men.
Rheumatoid arthritis diagnosis is based on a combination of clinical, laboratory, and radiographic findings. Patients with the disease present with joint pain, swelling, and decreased range of motion, predominantly affecting the PIPs, MCPs, wrists, knees, ankles, metatarsophalangeal (MTP) joints, and cervical spine. Patients will characteristically complain of morning stiffness lasting greater than 1 hour that improves with progressive joint use. Deformities of the fingers are common as the disease progresses. “Swan neck deformity” involves MCP flexion, PIP extension, and DIP flexion. Boutonnière deformity is characterized by PIP flexion and DIP extension. Ulnar deviation can be seen, in which the fingers are displaced medially (toward the ulna) at the MCP joint. Extra-articular manifestations are also common, involving the lungs, cardiovascular system, skin, and eyes. Rheumatoid factor, an anti-IgG antibody, is found in greater than 80% of patients with rheumatoid arthritis, although titers do not necessarily correlate with disease severity. Rheumatoid factor is also nonspecific for rheumatoid arthritis, and is seen in other autoimmune disease such as systemic lupus erythematosus, Sjögren’s syndrome, chronic inflammation, and uncommonly in asymptomatic individuals. Anti-cyclic citrullinated protein antibody (anti-CCP) has similar sensitivity as rheumatoid factor, but greater specificity. Additional laboratory findings include elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), and a positive antinucleic acid (ANA), although this is seen in less than 20% of patients.
The disease is characterized by inflammatory synovial hypertrophy, or pannus formation. The radiographic manifestations of rheumatoid arthritis ultimately derive from the effects of this pannus on the underlying bone and cartilage. One of the earliest radiographic findings is periarticular soft tissue swelling, which corresponds to pannus formation and joint effusion. Hyperemia of the synovium leads to periarticular osteoporosis. Proteases released by the pannus destroy the underlying bone leading to marginal erosions (marginal erosions are those that occur on the periarticular bare area of bone not covered by articular cartilage). Erosions are initially subtle and radiographically detected as disintegration of the thin white strip of bony cortex at the joint margin. The cartilage is also destroyed by these proteases, resulting in uniform joint space narrowing, in contrast to the asymmetric narrowing of osteoarthritis. After the articular cartilage is destroyed, larger subchondral erosions and subchondral cysts may form. As the disease advances, radiographic findings progress to include severe joint space narrowing, diffuse osteoporosis, and joint subluxations with resultant deformity. Because of severe cartilage loss, secondary osteoarthritis may form; however, there is discordance between the severe degree of joint space narrowing and relatively mild osteophyte formation and subchondral sclerosis. Rheumatoid arthritis predominantly affects the appendicular skeleton and spares the axial skeleton, with involvement of the axial skeleton limited to the cervical spine.
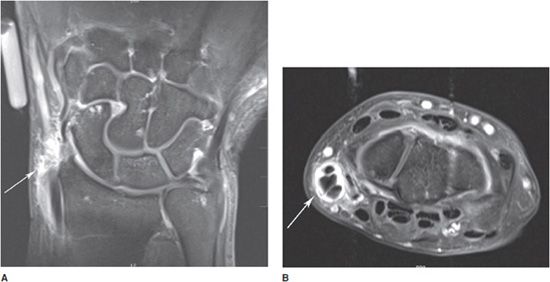
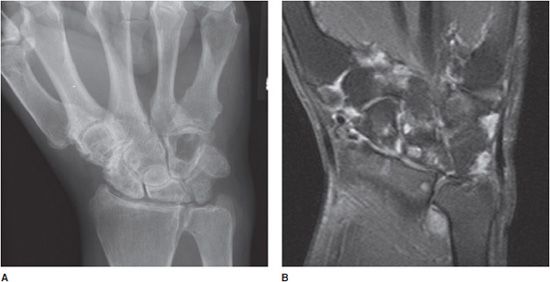
Rheumatoid arthritis classically involves the proximal joints of the hand and wrist, namely the PIP, MCP, ulnar, radiocarpal, and common carpal joints. The earliest signs of disease may include periarticular soft tissue swelling and periarticular osteoporosis. Inflammation of the tendon sheaths, referred to as tenosynovitis, may occur (Figure 6-6A,B). Erosions may be seen earliest at the MCP joints, typically at the radial aspect. With advancing disease, there is uniform cartilage loss throughout the joint space. Progressive osteoporosis leads to compressive collapse secondary to muscle tension along the joint, with resultant deformities of the fingers including Boutonnière and swan neck deformities. Progressive disease may ultimately lead to severe deformity (Figure 6-7). The earliest erosions in the wrist may occur at the ulnar and radial styloids (Figure 6-8A,B); however, pancompartmental changes may occur as the disease progresses. Erosions may be seen involving any of the carpal bones (Figures 6-9 and 6-10A,B). Tear of the triangular fibrocartilage complex (TFCC) is common in rheumatoid arthritis, which can be seen easily on arthrography (Figure 6-11) or MRI. Osteoporosis in males with rheumatoid arthritis may be less prominent despite advanced erosive changes (Figure 6-12).
Figure 6-6. Rheumatoid arthritis with De Quervain tenosynovitis. T1 postcontrast coronal (A) and axial (B) MRIs showing erosive changes of the carpal bones and distal ulna as well as contrast enhancement of the tendon sheathes of the extensor pollicis brevis and abductor pollicis longus tendons (white arrow).
Figure 6-7. Rheumatoid arthritis. Frontal view of the hand in a 59-year-old female demonstrating end-stage rheumatoid arthritis of the hand and wrist with marked osteoporosis and destructive changes of the carpal bones, distal radius and ulna, carpometacarpal, and metacarpophalangeal joints. There is subluxation and ulnar deviation of the metacarpophalangeal joints of the second through fourth fingers. There is complete dislocation of the fifth metacarpophalangeal joint.
Figure 6-8. Rheumatoid arthritis. PA radiograph (A) of the right wrist and coronal T1 postcontrast MRIs (B) in a 47-year-old male with early rheumatoid arthritis. Radiograph only shows soft tissue swelling around the wrist, especially at the ulnar styloid without underlying bony erosions evident. There is a suggestion of a widening of the scapholunate joint. MRI of the wrist shows contrast enhancement of the joint capsule and synovium with erosion of the radial (arrow) and ulnar (arrowhead) styloid and patchy bone marrow edema of the carpal bones. Note that MRI is superior to illustrating the extent of early disease compared with radiographs.
Figure 6-9. Rheumatoid arthritis. PA view of the wrist in a 63-year-old male shows erosive changes of the scaphoid, lunate, and most of the metacarpal heads. Note symmetric and concentric narrowing of the radiocarpal, common carpal, and carpometacarpal joints. There is prominent soft tissue swelling at the ulnar styloid and increased distance between the scaphoid and lunate due to scapholunate dissociation.
Figure 6-10. Rheumatoid arthritis. PA radiograph (A) and coronal proton density fat-saturated MRI (B) show erosive changes of the distal radius and the carpal bones with increased joint fluid.
Figure 6-11. Rheumatoid arthritis. AP arthrogram of the wrist of a patient with rheumatoid arthritis showing corrugated margin of the synovium secondary to synovial proliferation (arrowheads). Erosion of the triangular fibro-cartilage complex (TFCC) leads to the perforation of the radiocarpal joint with contrast seen in the distal radioulnar joint, indicative of TFCC tear (black arrow). Leakage of contrast from radiocarpal into common carpal joint is due to tear of the scapholunate and lunotriquetral ligaments.
Figure 6-12. Rheumatoid arthritis. PA view of the left wrist in a 45-year-old male shows robust, male-type rheumatoid arthritis with less remarkable osteoporosis. There are large subchondral cyst-like erosions of the distal radius and ulnar styloid and the capitate (black arrows). There is diffuse narrowing of the radiocarpal, intercarpal, and carpometacarpal joints. Note scapholunate dissociation (white arrowheads) and ulnar translocation of the carpal bones.
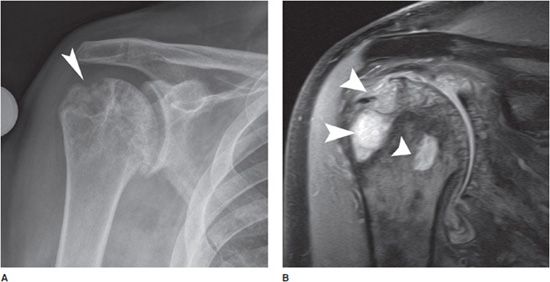
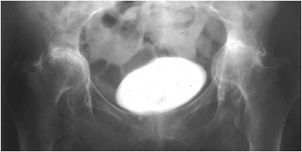
In the large joints of the appendicular skeleton, the disease is characterized by uniform joint space loss, periarticular osteopenia, and erosions. In the shoulder, there can be flattening of the glenoid, prominent erosions at the humeral head, osteoporosis and uniform joint space narrowing (Figure 6-13A,B). In advanced disease, the humeral head is elevated superiorly secondary to tears of the rotator cuff and there can be resorption of the distal clavicle (Figure 6-14). In advanced disease affecting the knee, there is uniform tricompartmental joint space narrowing with presence of erosions and often a suprapatellar joint effusion (Figure 6-15A–C). When the hip is involved, the joint is concentrically narrowed and the femoral head may migrate axially. As osteoporosis of the hip advances, protrusio acetabuli may occur, which is defined as the cortex of the medial femoral head projecting medial to the ilioischial line (Figure 6-16).
Figure 6-13. Rheumatoid arthritis. AP radiograph (A) and coronal proton density fat-saturated MRI image (B) of the right shoulder in a 71-year-old male show large cyst-like erosions of the humeral head (arrowheads), especially at the greater tuberosity. There is also osteoporosis and uniform joint space narrowing.
Figure 6-14. Rheumatoid arthritis. AP view of the left shoulder in a 77-year-old female shows severe osteoporosis, concentric glenohumeral joint narrowing with superior migration of the humeral head, narrowing of the acromiohumeral joint due to total atrophy of the rotator cuff and resorption of the distal clavicle.

Figure 6-15. Rheumatoid arthritis. AP (A) and lateral (B) radiographs and sagittal T2-weighted fat-saturated MRI (C) of the knee in a 63-year-old female. Radiographs show severe osteoporosis, symmetric joint narrowing and large subchondral cyst-like erosions, especially on the medial femoral and tibial condyles. Large suprapatellar bursa effusion (black arrow) and edema of Hoffa fat pad (white arrow) is also noted. MRI shows synovial proliferation and thickening (long arrow) with effusion (arrowhead) and large cyst-like erosions of the femoral and tibial condyle (short arrows).
Figure 6-16. Rheumatoid arthritis. AP radiograph of the pelvis shows severe osteoporosis, concentric, symmetric hip joint narrowing and bilateral protrusio acetabuli. Note contrast agent in the bladder is seen.
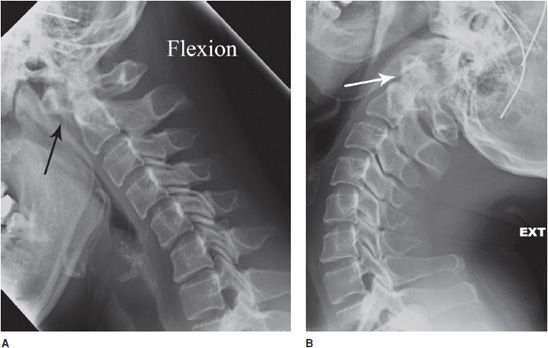
Rheumatoid arthritis involves the cervical spine in over half of patients. Pannus formation within the odontoid bursa leads to erosions at the posterior aspect of the dens. Synovitis in this location may eventually lead to destruction of the transverse ligament, leading to C1-C2 instability. This can be detected on flexion and extension radiographs of the cervical spine, which will demonstrate widening of the predens space on flexion view (Figure 6-17A,B). Evaluation of atlantoaxial instability is the reason flexion and extension radiographs are ordered in the preoperative evaluation of patients with rheumatoid arthritis. Multilevel subluxations may occur in the lower cervical spine leading to a “stepladder” appearance.
Figure 6-17. Rheumatoid arthritis. Flexion (A) and extension (B) views of the cervical spine in a 45-year-old female show widening of the distance in between the anterior tubercle of the atlas and the odontoid process (predens space, black arrow) due to atlantoaxial subluxation. There is also step ladder subluxation of C3 on C4 and C4 on C5 and C5 on C6. Note the predens space normalizes on extension view (white arrow), demonstrating the subluxation is dynamic.
For decades, radiographs have been the mainstay in the imaging evaluation of rheumatoid arthritis. Unfortunately, this modality is relatively insensitive to early disease. Historically, treatments had a limited effect on the progression of disease and instead focused on symptomatic relief. This paradigm has changed as a relatively new group of biologic immune modulating disease-modifying anti rheumatic drugs (DMARD) such as anti-TNF alpha have been proven to alter disease progression. Thus, there is increased need for more sensitive imaging modalities such as MRI to detect the changes of early stage disease.5 Treating this early stage disease may prevent some of the more severe late stage manifestations. On MRI, synovial proliferation/pannus formation is identified as synovial thickening that demonstrates avid gadolinium enhancement. Bone erosions are the result of overlying synovitis and appear as cortical defects usually adjacent to the enhancing synovium. Bone marrow edema (BME) can be appreciated as high T2 signal with amorphous boundaries. These foci of BME may be precursors for bone erosions. Tenosynovitis is inflammation of the synovial sheath surrounding tendons and it is an early manifestation of this disease and best appreciated when contrast is used for MRI. On MRI, it appears as thickening with avid enhancement, often associated with fluid. MRI can also be used to evaluate response to treatment, which is manifested as decreased synovial thickening and enhancement.5
PEARLS
 Juvenile Idiopathic Arthritis
Juvenile Idiopathic Arthritis
Juvenile idiopathic arthritis, also known as juvenile rheumatoid arthritis, refers to a group of related inflammatory arthropathies occurring in the pediatric population with unknown etiology. By definition, the onset is prior to age 16 and symptoms last for 6 weeks or greater. The most common presentation is pauciarticular disease, which involves four or less joints at onset. Other forms include polyarticular disease involving five or more joints, and systemic disease that combines fever and additional systemic symptoms with the arthritis.
Although several heterogeneous diseases with varying clinical presentations are grouped as juvenile idiopathic arthritis, the radiographic appearances are similar. The disease is characterized as an inflammatory arthropathy. Radiographic features include osteopenia, periarticular soft tissue swelling, marginal erosions related to synovial thickening (typically a late feature), joint space narrowing related to cartilage loss, and periostitis.6 Joint ankylosis may be seen and is more common than in adult rheumatoid arthritis. Joint contractures are not uncommon. Bony growth disturbances, such as early closure of the growth plate and overgrown epiphyses are often seen and particularly characteristic since the disease exerts its affects on an immature skeleton. Any joint may be affected, although there is a predilection for the large joints in pauciarticular disease.
The knees classically show epiphyseal overgrowth, which results in widening of the intercondylar notch. There is also characteristic squaring of the lower pole of the patella and commonly a joint effusion. In the hip, there is circumferential narrowing of the joint space and there may be coxa vara deformity, in which the angle between the femoral head and shaft is less than 120° (Figure 6-18). Osteopenia may also lead to ace-tabular protrusio similar to that seen in rheumatoid arthritis. The elbow is often involved with possible valgus deformity, effusion, and enlargement of the radial head. The mandible may also be affected, with shortening of the body and rami as well as flattening of the condyles. In polyarticular disease, the hand and wrist are most commonly involved. Growth disruption is common, manifested by epiphyseal overgrowth, premature closure of the growth plate resulting in brachydactyly (short digits). Distribution in the hand includes the MCP and IP joints. In the wrist, there is early maturation of the carpal bones, with ankylosis observed in about one-fifth of patients.
Figure 6-18. Juvenile idiopathic arthritis. AP view of the pelvis in a 18-year-old male shows concentric narrowing of the hip joints with shortening and erosion of the femoral necks bilaterally.
PEARLS
 Metabolic- and Crystal-Associated Disease
Metabolic- and Crystal-Associated Disease
Calcium Pyrophosphate Dihydrate Deposition Disease
Calcium pyrophosphate dihydrate (CPPD) deposition disease is the deposition of CPPD crystals into the periarticular soft tissues, including articular cartilage or fibrocartilage, synovium, articular capsule, tendons, ligaments, and menisci. CPPD has a variety of clinical presentations. Disease may be asymptomatic and solely manifested by calcification of the articular cartilage, called chondrocalcinosis. Patients may instead present with acute and recurrent inflammation due to CPPD crystal deposition in a joint. Such attacks are referred to as pseudogout and are diagnosed based on clinical presentation. Joint aspiration will reveal rhomboid, weakly positively birefringent crystals. Patients may also present with pyrophosphate arthropathy, which refers to the pattern of joint damage that occurs with CPPD crystal deposition. CPPD arthropathy may coexist with or without the acute painful attacks of pseudogout. CPPD deposition is more common with advancing age and affects males and females similarly. It is a common disease after age 80, and thus it is called a disease of octogenarians. Most cases of disease are considered idiopathic; however, there is an association with osteoarthritis and many metabolic disorders including hemochromatosis and hyperparathyroidism.
CPPD arthropathy is usually polyarticular and symmetric. While CPPD can affect any joint, typical distributions help to distinguish the disease from other arthropathies. Chondrocalcinosis in characteristic locations including the knee, symphysis pubis, and wrist (radiocarpal joint) (Figure 6-19) is highly associated with CPPD. CPPD can affect essentially any joint, however, with the hip, shoulder, and elbow generally involved. The mechanism of joint destruction involves damage to the articular cartilage secondary to crystal deposition. Progressive loss of articular cartilage can result in joint space narrowing, subchondral sclerosis, and osteophyte formation in involved joints that is similar, if not identical, to the findings of osteoarthritis. Therefore, distribution of disease within a particular joint is of particular significance, as certain patterns are classically associated with CPPD arthropathy and can help differentiate this entity from osteoarthritis.
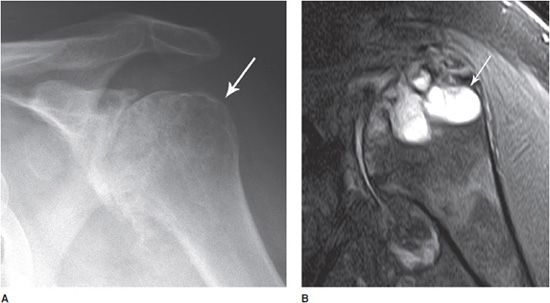
Figure 6-19. Calcium pyrophosphate deposition disease. Extensive calcification around metacarpophalangeal joints with joint narrowing, erosions, and chondrocalcinosis.
In the hands and wrist, the MCP (particularly the second and third) and radiocarpal joints are typically affected, in contrast to the distal involvement that distinguishes primary osteoarthritis. At the MCP joints, characteristic “hook” osteophytes may form at the metacarpal heads (Figure 6-20). Radial deviation of the MCP joints may occur. Chondrocalcinosis of the triangular fibrocartilage of the wrist is typical. In advanced disease, scapholunate advance collapse (SLAC) may occur, in which the scaphoid and lunate dissociate from each other, with proximal migration of the capitate. In the shoulder, there is circumferential narrowing of the glenohumeral joint in association with chondrocalcinosis (Figure 6-21). CPPD can also be associated with subchondral cyst or geode formation (Figure 6-22A,B).7 There is often narrowing of the subacromial space, which is similarly seen in rheumatoid arthritis, indicative of rotator cuff atrophy or tear. In the knee joint (Figure 6-23A,B), there is classically significant narrowing of the patellofemoral compartment (target joint) in distinction to the medial compartment narrowing associated with osteoarthritis. Chondrocalcinosis of the femoral cartilage and menisci is often best appreciated on the frontal view. Pyrophosphate arthropathy at times is so severe that it may resemble a neuropathic or Charcot joint. In the hip, there is axial (circumferential) narrowing of the femoroacetabular joint and associated osteophyte formation (Figure 6-24). In the cervical spine, CPPD can cause a partially calcified lesion posterior to the odontoid process (Figure 6-25), which in severe cases can result in compression of the cervical spinal cord. CPPD can have a similar appearance to hydroxyapatite deposition disease and gout in the cervical spine.
Figure 6-20. Calcium pyrophosphate deposition disease. PA view of both hands in a 39-year-old male shows chondrocalcinosis of the triangular fibrocartilage (white arrows) and metacarpophalangeal joints with hook-like osteophyte formation at the metacarpal heads (black arrow).
Figure 6-21. Calcium pyrophosphate deposition disease. External oblique radiograph (Grashey view) in a 68-year-old male shows significant axial narrowing of the glenohumeral joint with sclerosis, chondrocalcinosis (arrowheads), and calcification of the joint capsule.
Figure 6-22. Calcium pyrophosphate deposition disease. AP external (A) rotation view of the left shoulder and coronal oblique proton density fat-saturated MRI (B) in a 68-year-old male show significant axial narrowing, osteophyte formation, and chondrocalcinosis. Note subchondral cyst formation on radiograph and MRI (white arrow). (Reprinted with permission of Anderson Publishing Ltd. from Farpour F, Maasumi K, Tehranzadeh J. Imaging of crystal deposition diseases. Applied Radiology. Aug 2012. ©Anderson Publishing Ltd.)
Figure 6-23. Calcium pyrophosphate deposition disease. AP (A) and lateral (B) views of the bilateral knees in a 39-year-old male show articular cartilage and meniscal calcification of both knees at the femorotibial and femoropatellar joints. Note significant femoropatellar joint narrowing and joint effusion.
Figure 6-24. Calcium pyrophosphate deposition disease. AP view of the pelvis in a 39-year-old male shows chondrocalcinosis of the hip joints with axial joint narrowing and osteophyte formation of both hips. Note erosive changes at the sacroiliac joints and the symphysis pubis.
Figure 6-25. Calcium pyrophosphate deposition disease. Sagittal reformat from a CT of the cervical spine in a 81-year-old male shows odontoid erosion and narrowing of the atlantoodontoid joint. Note calcification in the region of the transverse ligament posterior to the odontoid (white arrow). There is also disk space narrowing and irregularity of the end plate with cystic changes and osteophytes at the C5 to T1 disk spaces.
PEARLS
Hemochromatosis
Hemochromatosis is a disease of iron overload, which results in soft tissue and organ deposition with subsequent fibrosis and organ toxicity. The disease may be hereditary and caused by increased gastrointestinal iron absorption, or secondary and related to causes such as increased iron intake or frequent blood transfusion. Clinical manifestations include cirrhosis, bronzing of the skin, hypogonadism, diabetes, cardiomyopathy, and arthropathy. Arthropathy is seen in approximately 50% of patients with hemochromatosis and is degenerative in nature, with joint space narrowing, sclerosis, subchondral cysts, and osteophyte formation. The distribution, however, is characteristic and classically involves the second and third MCP joints. Large “hook-like” osteophytes are commonly seen at the radial aspect of the affected meta-carpal heads. Up to half of patients with hemochromatosis also have CPPD deposition disease, thus chondrocalcinosis is commonly seen. Other affected joints may include the radio-carpal joints, knee, shoulder, or hip (Figure 6-26A,B), similar in distribution and appearance to CPPD deposition disease.
Figure 6-26. Hemochromatosis. PA oblique view of the bilateral hands (A) demonstrates hook-like osteophytes with erosion at the metacarpal phalangeal joints with calcification of the TFCC cartilage of the wrist. Transaxillary view of the shoulder (B) shows significant concentric narrowing and sclerosis of the glenohumeral joint (bone on bone) with total loss of cartilage and osteophyte formation. (Reproduced from Afshin A, Zoga A. Hemochromatosis. In: Musculoskeletal Imaging Cases, Tehranzadeh J, ed. New York, NY: McGraw-Hill; 2009:266-267.)
PEARLS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree