LEARNING OBJECTIVES
1. Identify a widened mediastinum on a posttrauma chest radiograph and state the differential diagnosis (including aortic/arterial injury, venous injury, and fracture of sternum or thoracic spine).
2. Identify and describe the indirect and direct signs of aortic injury on contrast-enhanced chest computed tomography (CT).
3. Identify, describe the features of, and state the significance of chronic traumatic pseudoaneurysm of the aorta on a chest radiograph, CT, or magnetic resonance imaging (MRI).
4. Identify fractured ribs, clavicle, spine, sternum, and scapula on a chest radiograph or CT.
5. Name five common causes of abnormal lung opacification on a posttrauma chest radiograph or CT.
6. Identify an abnormally positioned diaphragm or loss of definition of a diaphragm on a posttrauma chest radiograph, and suggest the diagnosis of ruptured diaphragm.
7. Recognize and describe the signs of diaphragmatic rupture on a chest CT.
8. Identify pneumothorax, pneumopericardium, and pneumomediastinum on a chest radiograph or CT.
9. Identify the fallen lung sign on a chest radiograph or CT and suggest the diagnosis of tracheobronchial tear.
10. Identify a cavitary lesion on a posttrauma chest radiograph or CT, and suggest the diagnosis of laceration with pneumatocele formation.
11. Recognize and distinguish between laceration and contusion on a chest radiograph or CT.
Each year in the United States, more than 300,000 patients are hospitalized, and 25,000 people die as a direct result of chest trauma (1). Thoracic injury accounts for 25% of all traumatic deaths, and substantial chest trauma is a factor in 50% of fatal traffic accidents (2). Most of the chest trauma seen in civilian populations is blunt chest trauma (90%), usually a result of motor vehicle crashes and falls (3). The incidence of penetrating trauma is stabilizing or decreasing, and many penetrating wounds to the chest can be treated by observation or tube thoracostomy alone (4) (Figs. 8.1 to 8.3).
After a patient has been clinically evaluated and stabilized, a chest radiograph is usually obtained. These radiographs are often compromised by limited exposure capability, low lung volumes, poor or absent patient cooperation, obscuration of thoracic anatomy by portions of external monitoring and support devices overlying the patient, suboptimal or supine patient positioning, and magnification and distortion of the mediastinum. In one study, computed tomography (CT) was superior to supine chest radiography in showing findings of chest trauma, and the CT findings influenced patient management in a significant number of patients (5). This chapter reviews the chest radiographic and CT findings of blunt trauma to the chest.
AORTIC AND GREAT VESSEL INJURY
Traumatic rupture of the aorta alone accounts for 16% of fatalities resulting from motor vehicle crashes, and 85% to 90% of patients with traumatic aortic rupture die before reaching a medical facility (6). In clinical series, 90% of aortic ruptures occur at the aortic isthmus, just distal to the origin of the left subclavian artery (7–10) (Figs. 8.4 to 8.6). A few aortic injuries (1% to 3%) involve the descending thoracic aorta, typically at the level of the diaphragm (Fig. 8.7). Chest radiographic signs of aortic injury lack sensitivity and specificity. The most sensitive (but not specific) radiographic signs are widening of the mediastinum and loss of definition of the aortic arch (Table 8.1) (11). A normal chest radiograph has a high negative predictive value (98%) but a low positive predictive value for aortic injury.
Contrast-enhanced, thin-section CT scanning (3-mm collimation or less with overlapping reconstructions) has replaced conventional aortography in evaluating patients for aortic injury. Direct signs of aortic injury on CT include (a) aortic caliber change at the site of injury (pseudoaneurysm or pseudocoarctation), (b) abnormal or irregular aortic wall or contour, (c) intraluminal irregularities or areas of low attenuation (clot, linear intimal flap), (d) intramural hematoma or dissection, and (e) active extravasation of contrast. CT is useful not only for detecting direct signs of aortic injury, but also for its ability to show other causes of a wide mediastinum, including venous bleeding (Fig. 8.8), excessive mediastinal fat (Fig. 8.9), paramediastinal atelectasis or pleural effusion, residual thymic tissue, adjacent lung injury (Fig. 8.10), artifact caused by supine positioning, vascular tortuosity, vascular anomalies, lymphadenopathy, and persistent left-sided superior vena cava (12).
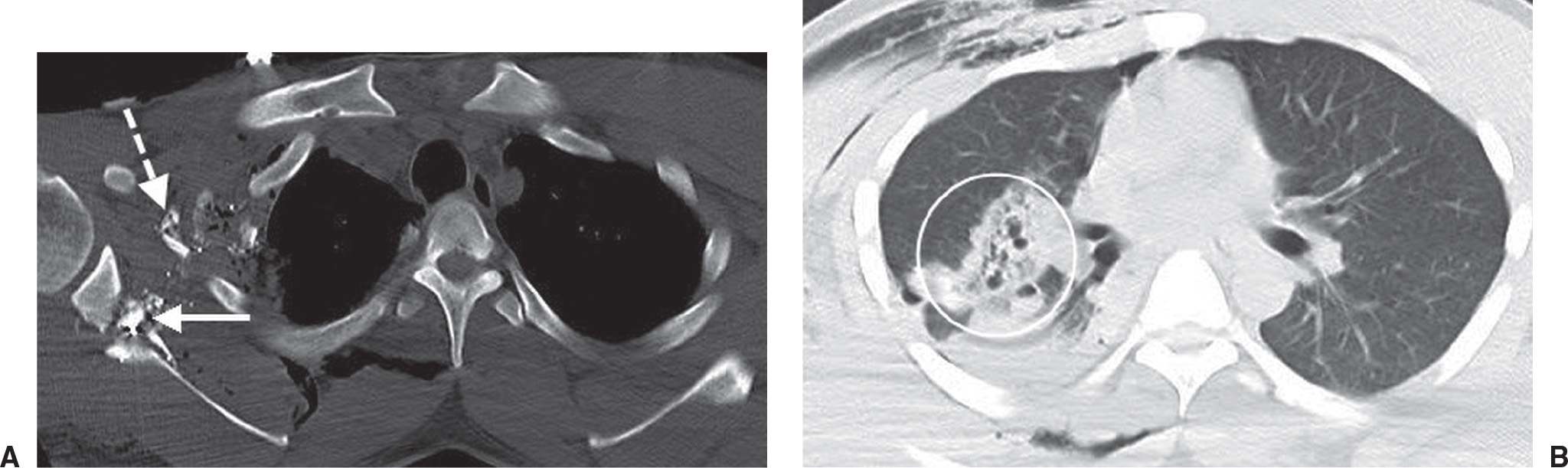
FIG. 8.1 • Penetrating injury. A: CT scan with bone windowing of a 29-year-old man who sustained a gunshot wound to the right shoulder and chest shows metallic fragments adjacent to a comminuted fracture of the right scapula (solid arrow) and comminuted right rib fractures (dashed arrow). B: CT scan with lung windowing shows multiple lucencies within an area of consolidation in the right upper lobe (circle), indicating pulmonary lacerations. There is also subcutaneous emphysema.
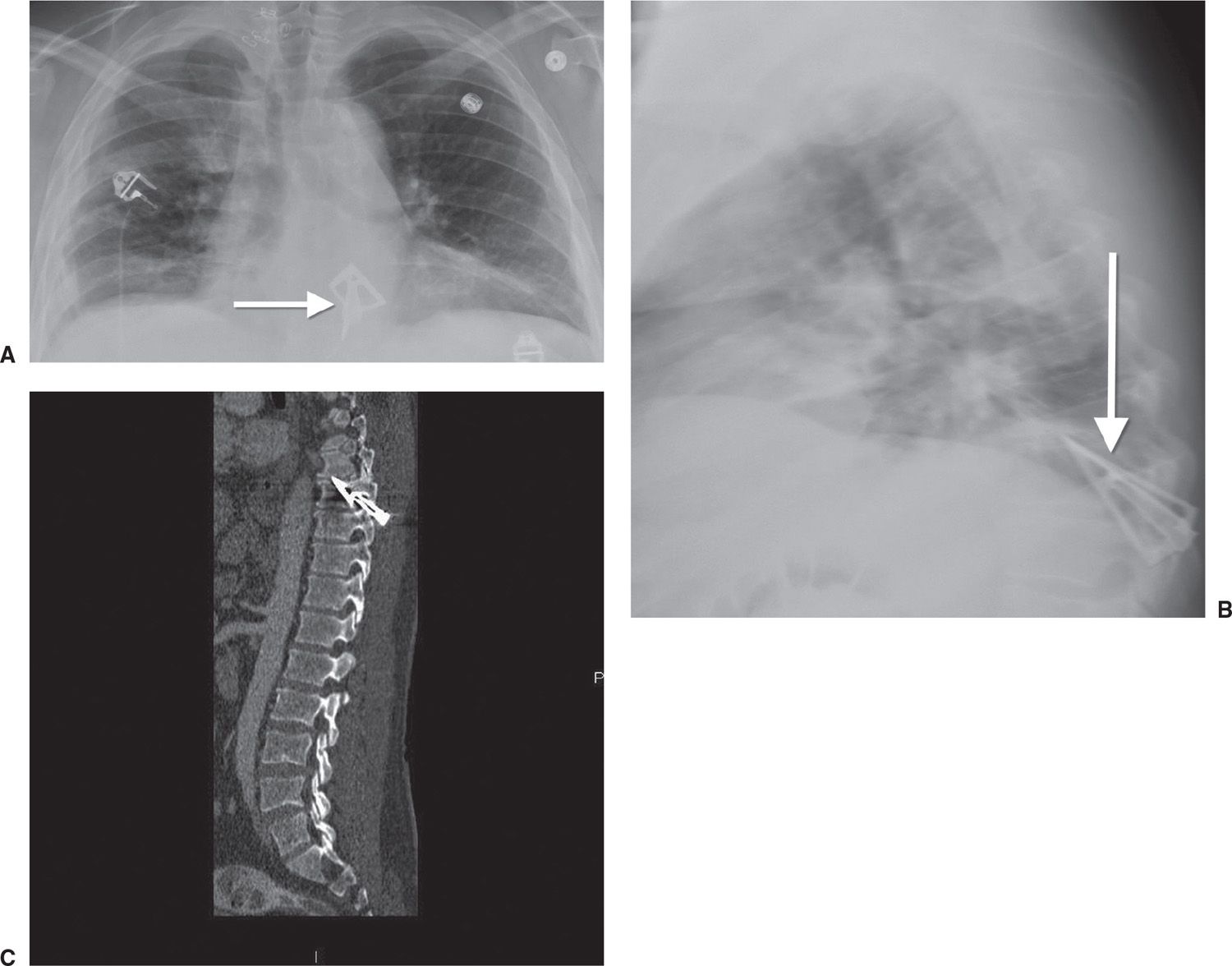
FIG. 8.2 • Penetrating injury. Posteroanterior (PA) (A) and lateral (B) chest radiographs of a 50-year-old man shot with an arrow show an arrow within the thoracic spine (arrow). C: Sagittal reformatted CT scan confirms the (arrow) placement.
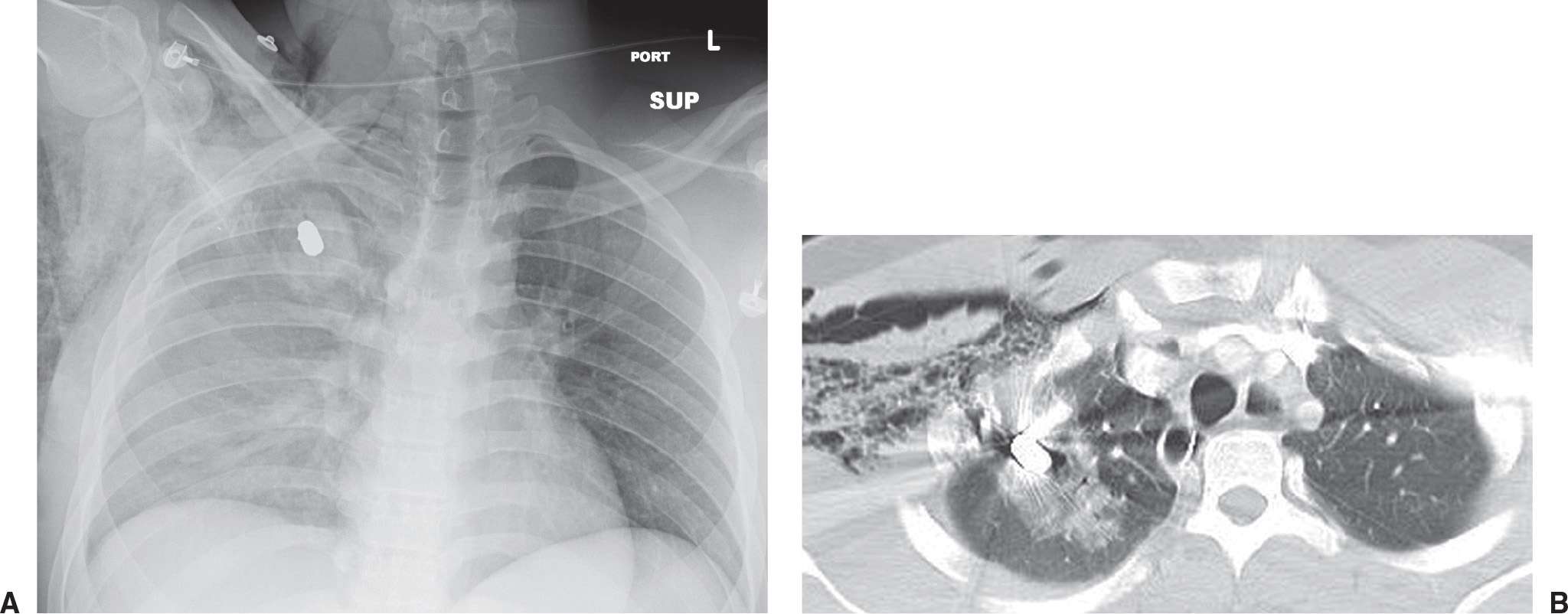
FIG. 8.3 • Penetrating injury. A: PA chest radiograph of an 18-year-old man who sustained a gunshot wound to the chest shows a metallic bullet with adjacent opacity (hematoma) in the right upper lobe. There is also hazy opacity throughout the right hemithorax and subcutaneous emphysema. B: CT scan shows the bullet and adjacent ground-glass opacity representing hemorrhage.
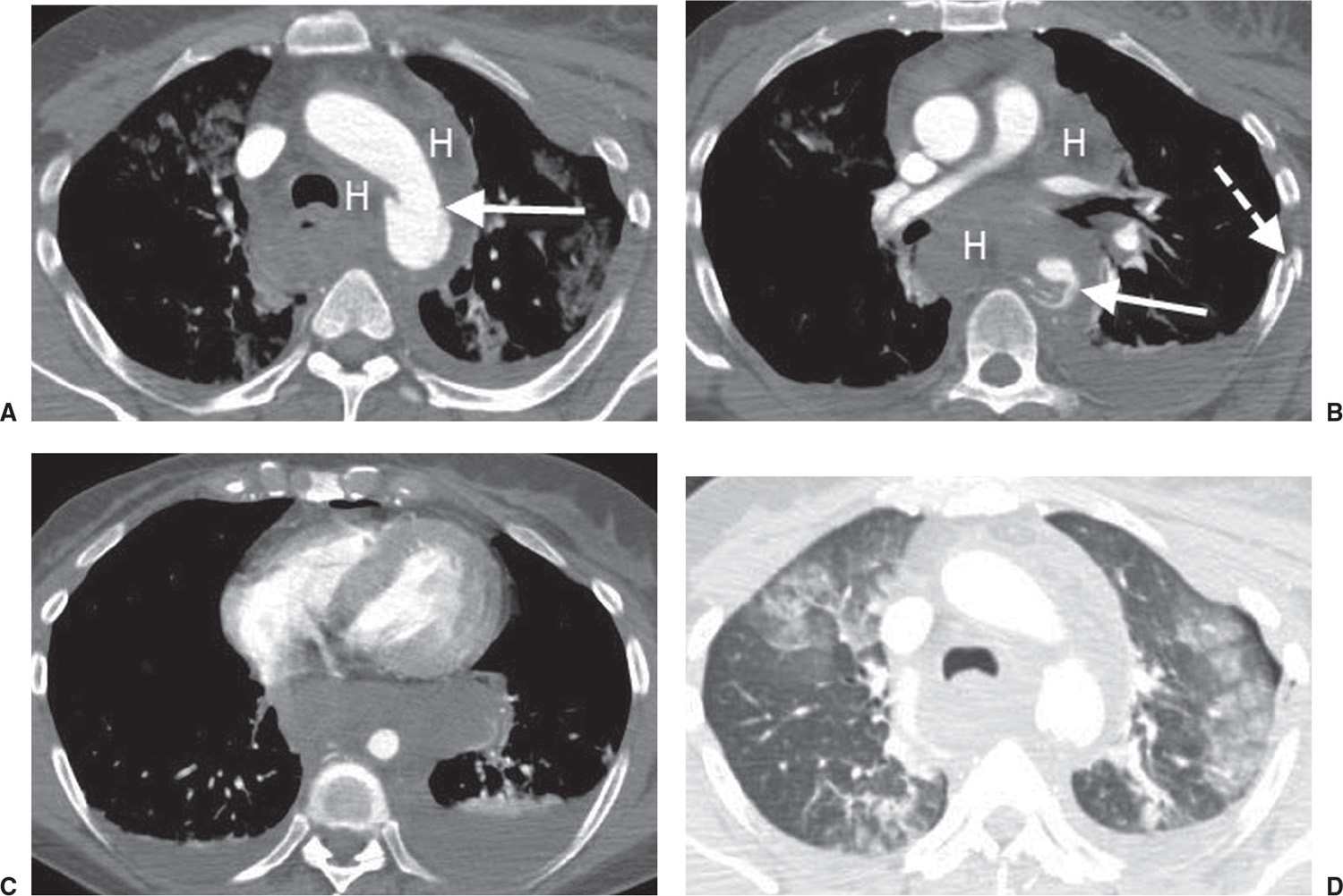
FIG. 8.4 • Aortic laceration. A: CT scan of a 52-year-old woman involved in a motor vehicle crash shows aortic caliber change at the level of the isthmus (arrow) and extensive mediastinal hemorrhage (H). B: CT scan at a level inferior to (A) shows a disrupted aorta (arrow) and mediastinal hemorrhage (H). C: CT scan at a level inferior to (B) shows diminution of the aortic caliber below the tear and surrounding hematoma. D: CT scan with lung windowing shows a left pneumothorax and subpleural ground-glass opacity representing lung contusions.
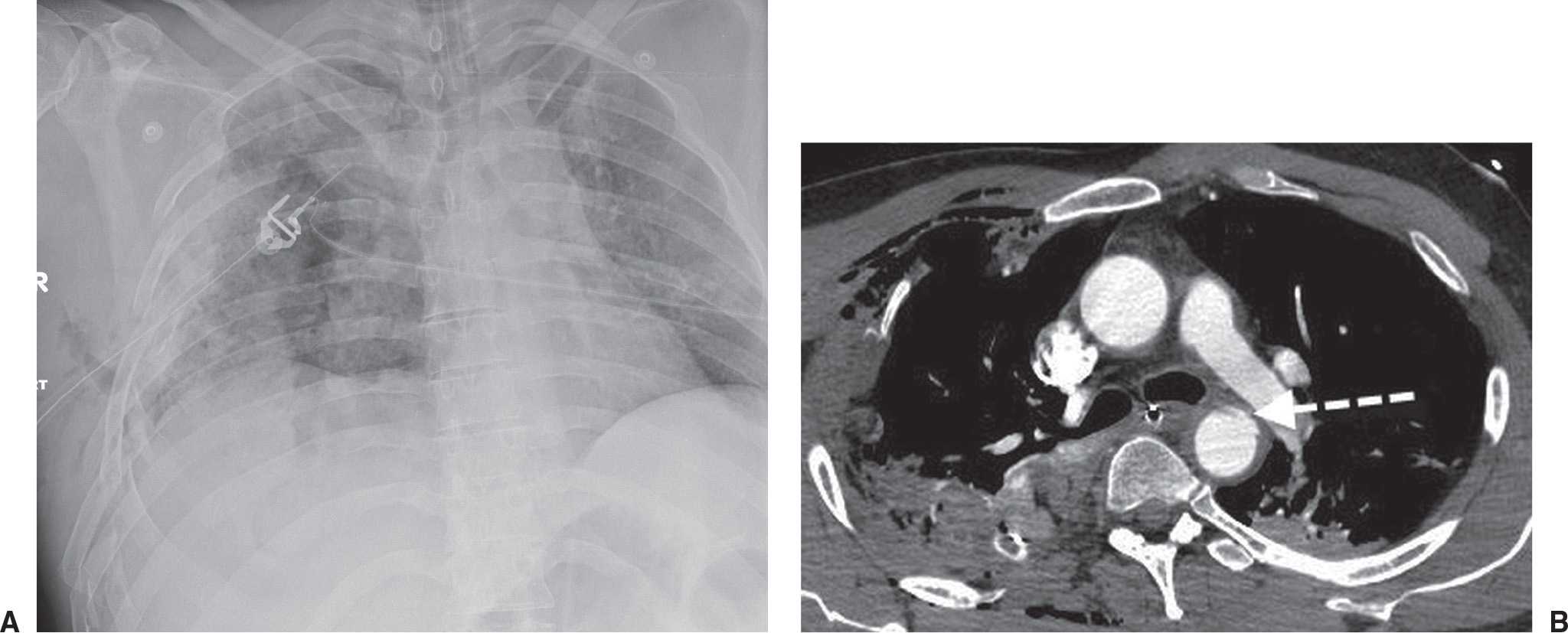
FIG. 8.5 • Aortic laceration. A: PA chest radiograph of a 49-year-old male injured in an all-terrain vehicle that went off a cliff shows diffuse opacity throughout the right hemithorax, a right chest tube, and numerous contiguous right rib fractures (creating a flail chest). The upper mediastinum is wide, and the aortic arch is not visualized. B: CT scan shows irregularity in aortic contour at the level of the isthmus (dashed arrow), representing laceration.
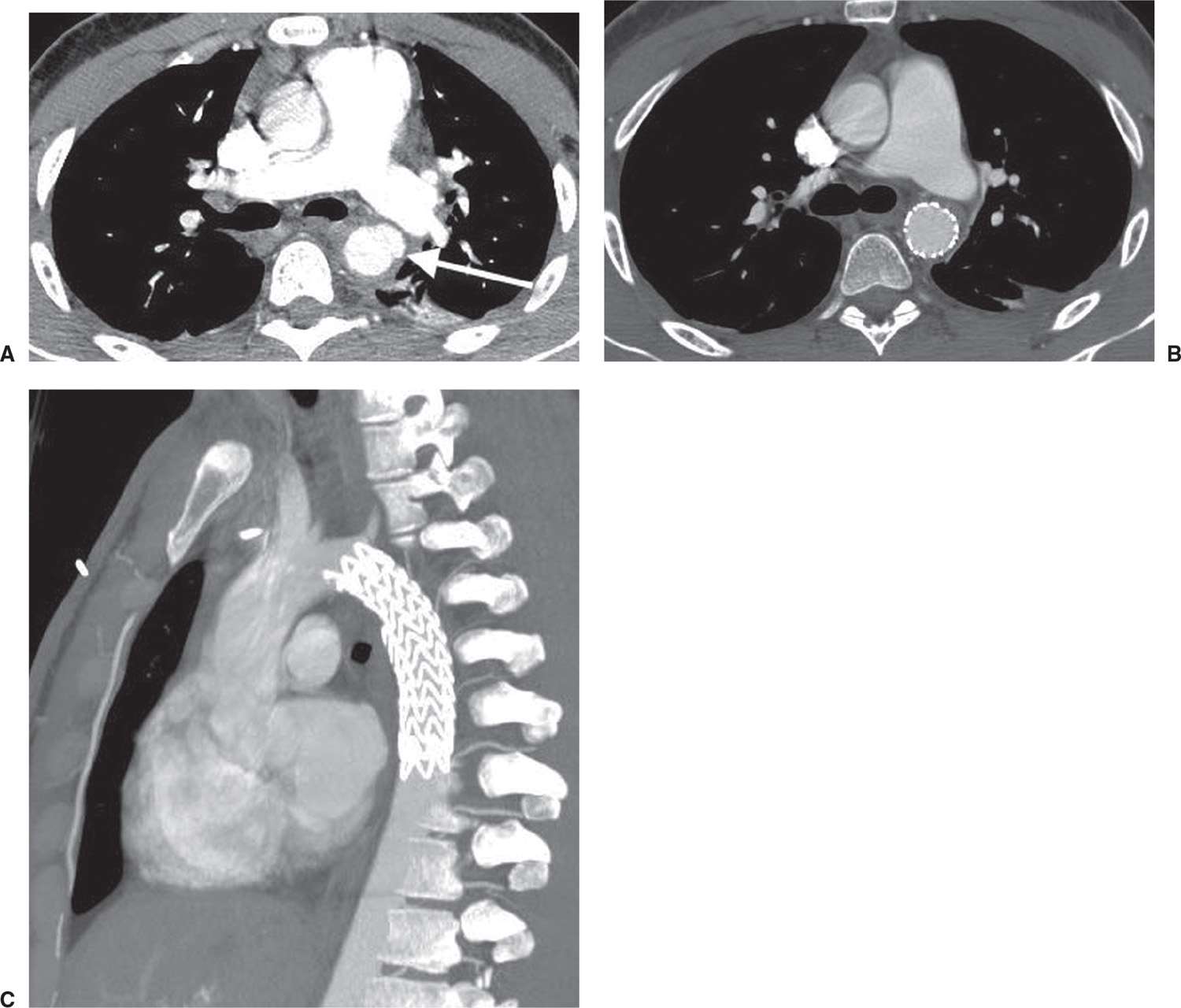
FIG. 8.6 • Aortic laceration. A: CT scan of a 22-year-old man involved in a motor vehicle crash shows aortic wall irregularity and caliber change representing laceration and pseudoaneurysm (arrow). B: CT scan acquired after intervention shows a stent at the site of the lacerated aorta. C: Sagittal reformatted CT scan shows a metallic stent spanning the aortic injury.
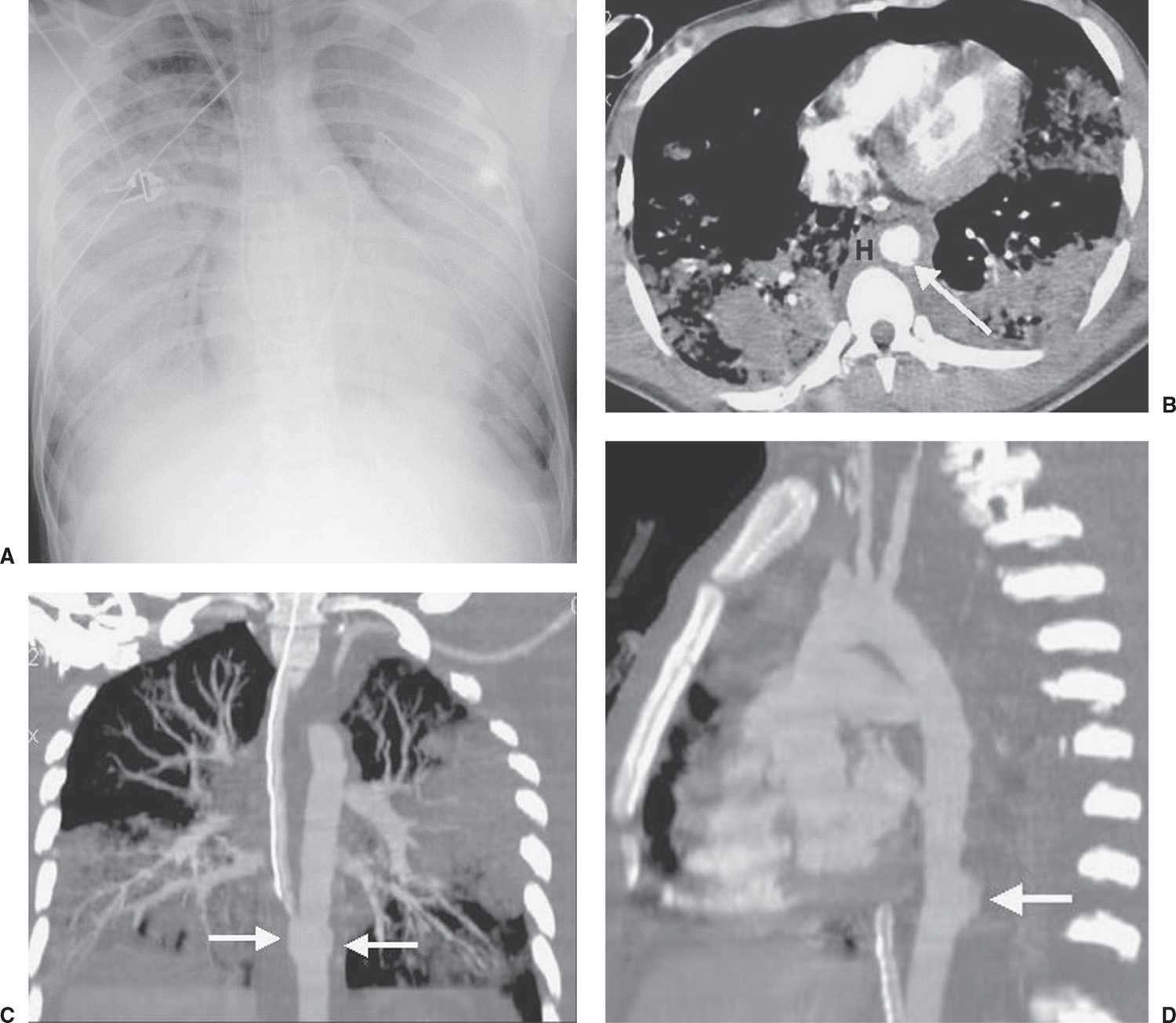
FIG. 8.7 • Descending aortic laceration. A: Anteroposterior (AP) supine chest radiograph shows diffuse opacity of both hemithoraces. B: CT scan shows periaortic hematoma (H) and irregular contour of the descending aorta (arrow). Coronal (C) and sagittal (D) reformatted CT images show a pseudoaneurysm of the descending aorta (arrows).
Table 8.1 CHEST RADIOGRAPHIC SIGNS OF AORTIC INJURY
Widening of the mediastinum
Obscuration of the aortic arch
Abnormal aortic contour
Hemothorax
Rib fractures
Tracheal shift to the right
Left apical cap
Depression of the left mainstem bronchus below 40 degrees
Nasogastric tube displacement to the right
Pneumothorax
Pulmonary contusion
Widened left paraspinous line
Potential pitfalls in CT interpretation include hemomediastinum caused by sternal or vertebral body fracture, left pleural effusion with left lower lobe subsegmental atelectasis “surrounding” the aorta, pulsation artifacts, atherosclerotic plaques, prominent ductus arteriosus, and pseudointimal flaps secondary to volume averaging of the left brachiocephalic vein as it crosses in front of the aortic arch. These pitfalls have become less of a problem with the use of multidetector CT and fast scanning techniques.
Occasionally, patients will survive long term with an unrepaired pseudoaneurysm and develop a chronic pseudoaneurysm (13). Calcification of the wall of the aneurysm and a history of prior thoracic trauma indicate an old aortic injury (Fig. 8.11).
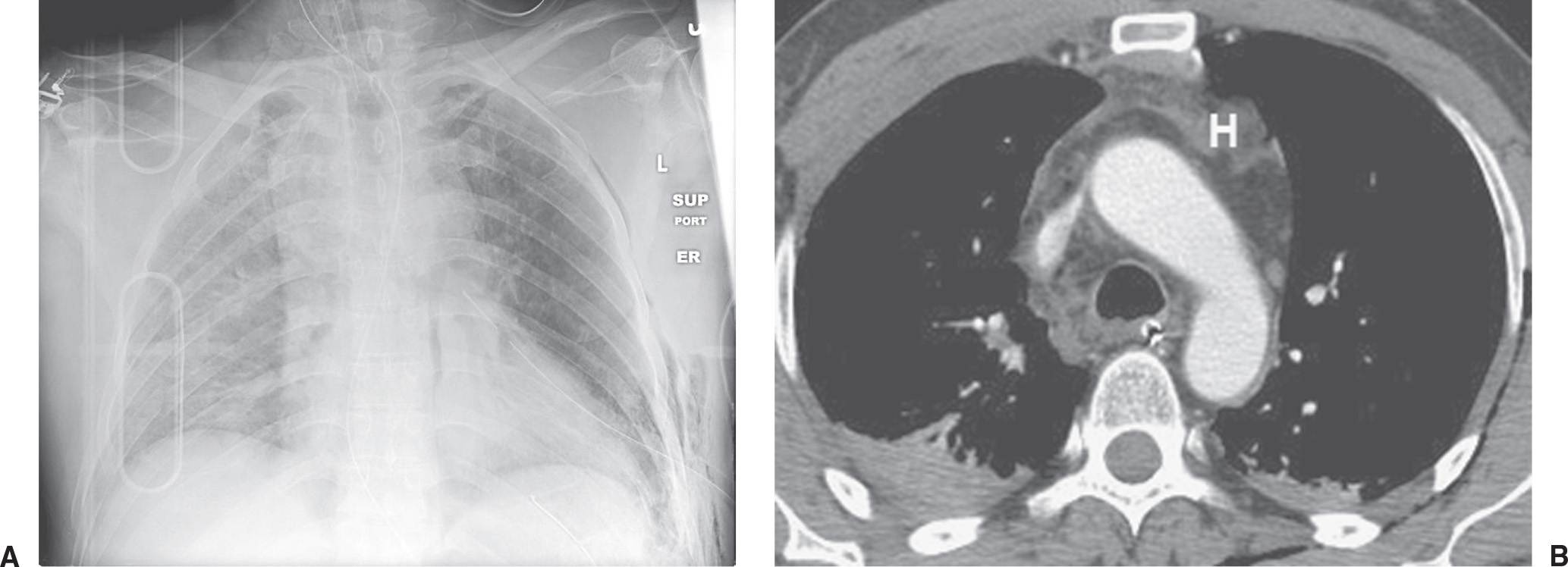
FIG. 8.8 • Mediastinal hematoma. A: AP supine chest radiograph of a patient involved in a motor vehicle crash shows a wide mediastinum. B: CT scan shows blood in the mediastinum (H). Note the preservation of a fat plane between the mediastinal blood and the normal aorta, which in the absence of a sternal or spine fracture indicates that the bleeding was venous and not arterial.
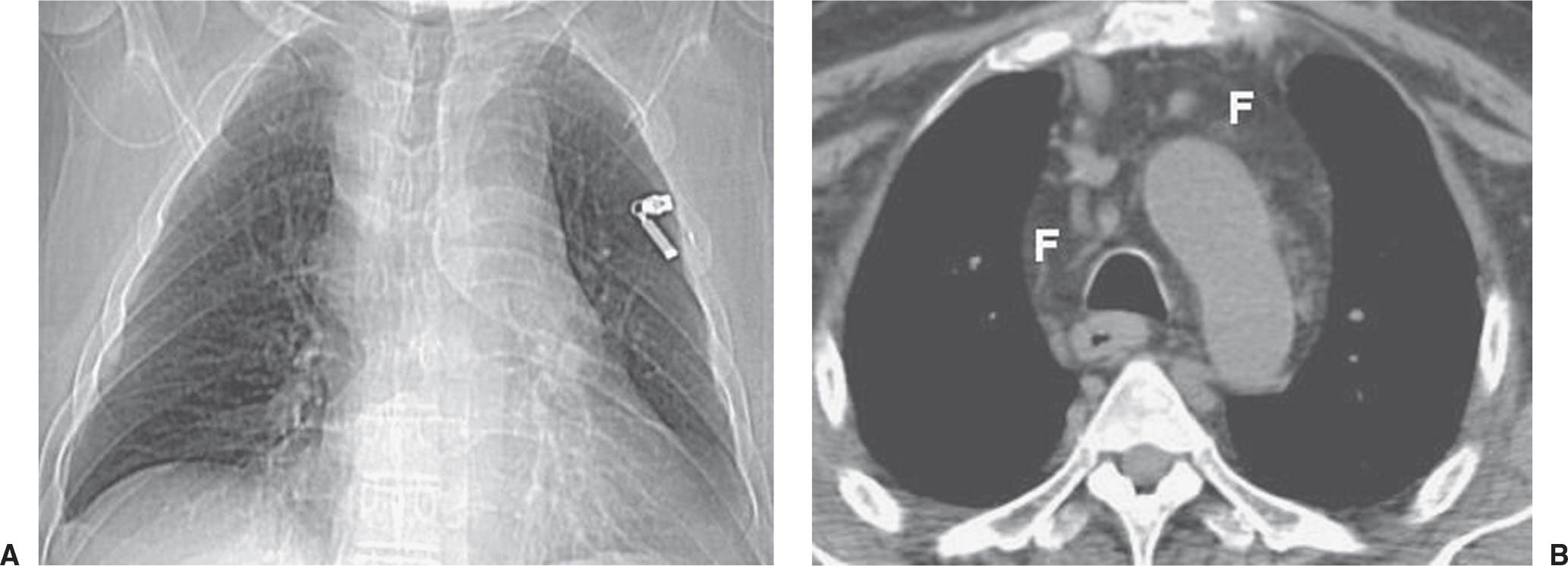
FIG. 8.9 • Mediastinal fat. A: CT chest scout view shows a wide mediastinum. B: Axial CT shows abundant mediastinal fat (F), normal lymph nodes, and no aortic injury or mediastinal mass.
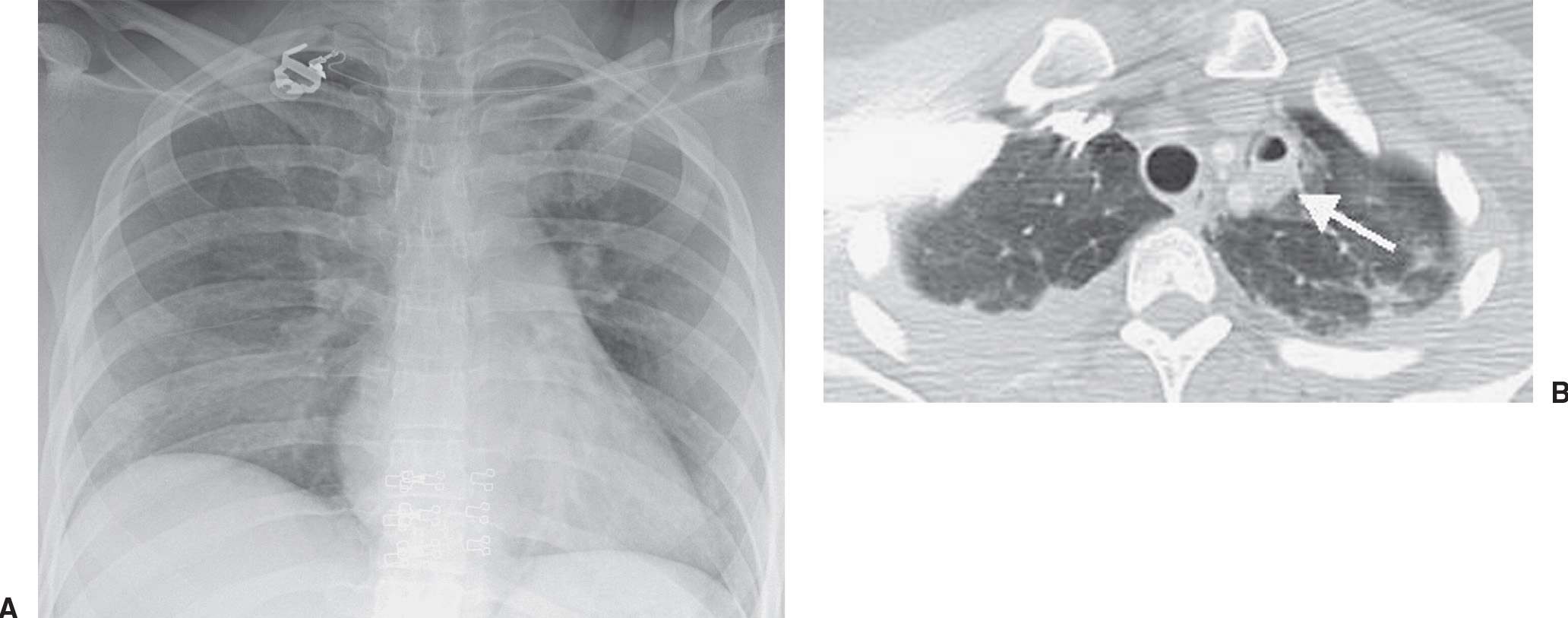
FIG. 8.10 • Lung laceration. A: AP supine chest radiograph of a patient involved in a motor vehicle crash shows a wide upper mediastinum and lack of definition of the aortic arch. B: CT shows airspace opacity with central lucency, consistent with laceration and pneumatocele formation, adjacent to the upper mediastinum (arrow).
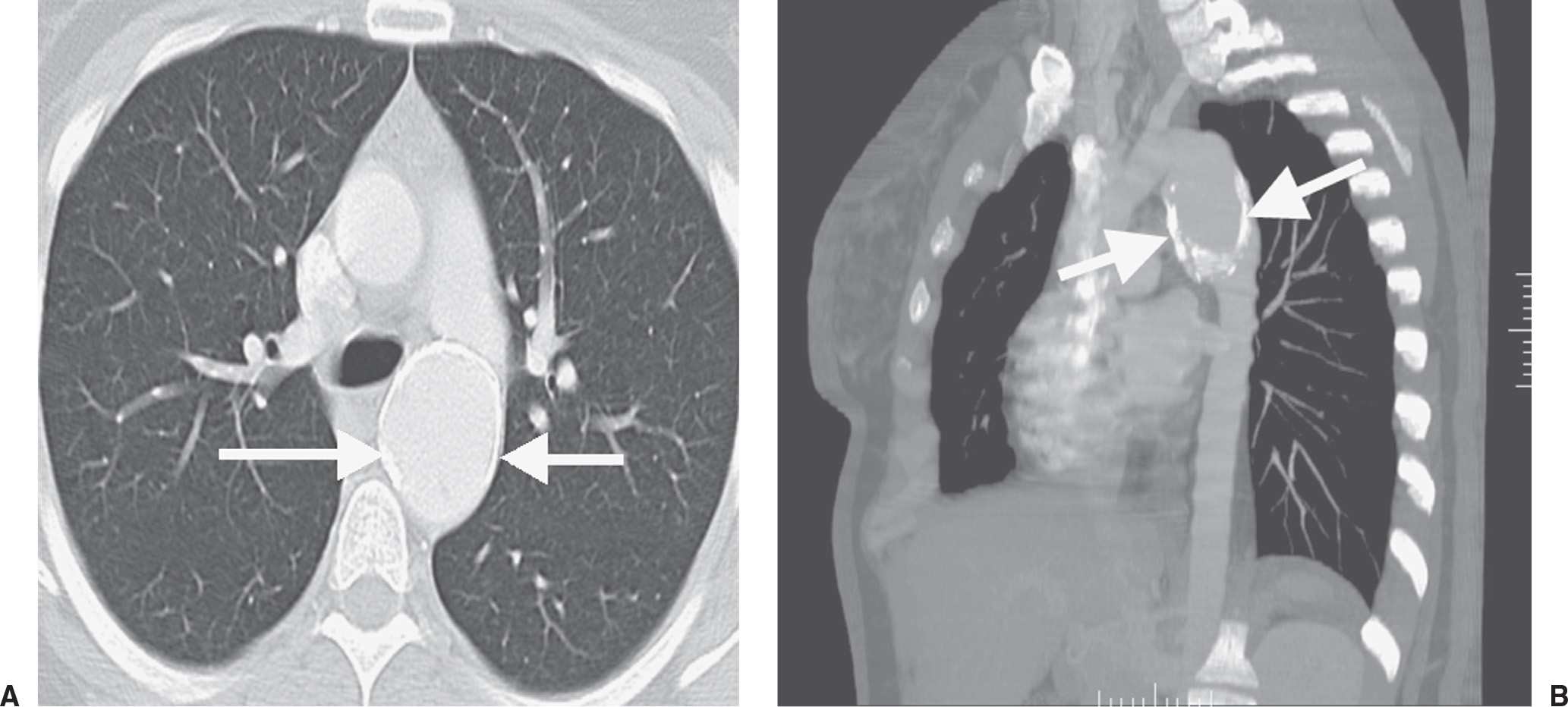
FIG. 8.11 • Chronic pseudoaneurysm. A: CT scan of a patient with a remote history of chest trauma shows a dilated descending aorta with dense rim calcification (arrows). B: Sagittal reformatted CT scan shows a densely calcified aortic pseudoaneurysm (arrows) at the level of the isthmus.
Great vessel injuries (with or without concomitant aortic tear) occur in 1% to 2% of patients with blunt chest trauma (14). A perivascular superior mediastinal or low cervical hematoma, especially in the presence of upper rib fractures or posterior sternoclavicular dislocation, should prompt concern for great vessel injury and injury to other structures in the thoracic inlet (Fig. 8.12).
LUNG PARENCHYMAL INJURY
Abnormal lung parenchymal opacification in trauma patients can result from atelectasis, aspiration, edema, pneumonia, and lung injury (contusion and laceration), and is commonly multifactorial in etiology. Pulmonary contusion (“lung bruise”) results in leakage of blood and edema fluid into the interstitial and alveolar spaces. Pulmonary laceration is a more severe injury that causes frank disruption of the lung architecture.
CT is more sensitive than radiography in demonstrating contusions and lacerations (15–22). On both chest radiography and CT, pulmonary contusions present as areas of consolidation, ground-glass opacification, or both, which tend to be peripheral, nonsegmental, and geographic in distribution (Fig. 8.13). Isolated pulmonary contusion in young, healthy patients is not associated with increased mortality (23). Contusions are typically evident at the time of injury, and they resolve, usually without permanent sequelae, within 5 to 7 days.
Pulmonary laceration results in tearing of the lung parenchyma and formation of a cavity filled with blood (hematoma), air (pneumatocele), or both. This injury may initially be masked by coexistent contusion and other forms of chest injury on the initial radiograph or CT scan, and it generally takes weeks to months to resolve, sometimes with residual scarring. The radiographic or CT diagnosis of lung laceration is based on the presence of a localized air and/or fluid collection within an area of airspace opacity in the setting of acute chest trauma (20) (Figs. 8.14 and (8.15). Lacerations can occur adjacent to solid structures, such as the ribs, from direct puncture, and from shearing along vertebral bodies (Fig. 8.16), and also centrally in the lung from compression rupture.
Fat embolization syndrome is characterized by abnormal diffuse lung opacification on chest radiography, dyspnea, mental status changes, and a petechial rash occurring 12 to 72 hours after trauma. Occurring most commonly after long bone fractures or their repair, fat embolization syndrome results when fat droplets from bone marrow are released into the circulation and occlude capillaries. The patient’s symptoms are caused by the decrease in perfusion to various organs from capillary occlusion. In the lungs, chemical pneumonitis ensues as a result of lipolysis and release of free fatty acids, causing lung injury, which does not occur immediately after trauma and accounts for the 12- to 72-hour delay in clinical signs and symptoms. The chest radiograph initially appears normal but develops patchy opacities and then widespread diffuse opacity within 72 hours of injury. The pulmonary opacity resembles pulmonary edema from other causes, with perihilar and basilar predominance and sparing of the lung apices (24) (Fig. 8.17). With fat embolization syndrome, the pulmonary opacity does not clear with diuresis. Contusion is generally seen earlier than fat embolization syndrome on the chest radiograph, and it clears more rapidly (5 to 7 days). Pulmonary opacity from fat embolization syndrome can take 7 to 10 days to clear.
TRACHEOBRONCHIAL INJURY
The incidence of tracheobronchial injury (TBI) is reported as 0.4% to 1.5% in clinical series of major blunt trauma (25). Blunt trauma must be severe to cause airway rupture, and injury to other structures such as the thoracic cage, lungs, and great vessels is likely. When the intrathoracic trachea or bronchi are injured, the aorta is the most commonly associated injured structure (26). TBI is associated with a 30% overall mortality rate, mostly from associated injuries (27). Failure to recognize TBI may result in death or allow cicatrization to occur at the site of injury, with airway obstruction arising days or months after initial injury (Fig. 8.18). More than 80% of TBIs occur within 2.5 cm of the carina (28,29).
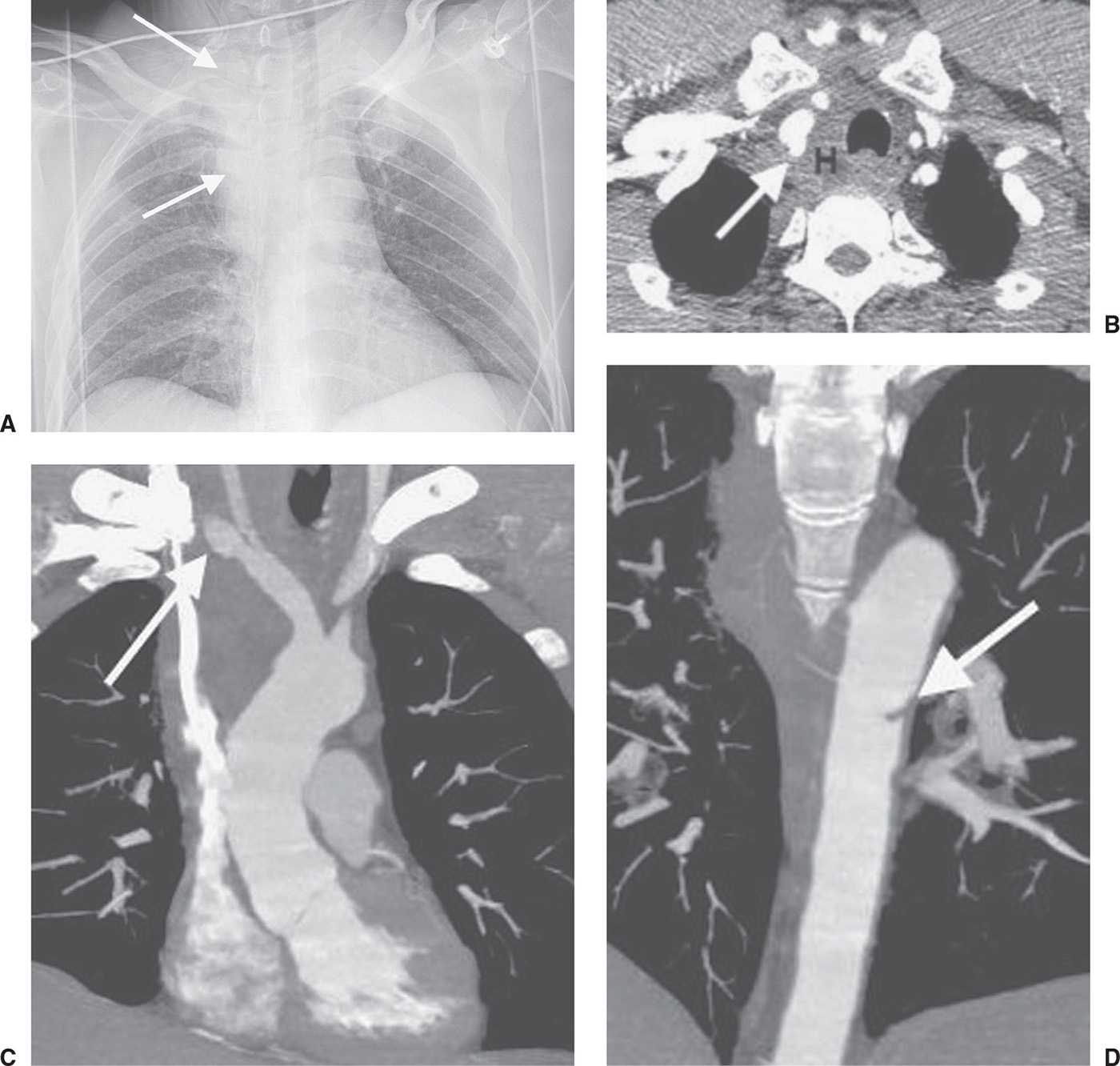
FIG. 8.12 • Concurrent subclavian artery and aortic injuries. A: AP supine chest radiograph of a patient involved in a motor vehicle crash shows a wide upper mediastinum (arrows) and leftward shift of the trachea. B: CT scan shows mediastinal hematoma (H) and pseudoaneurysm of the right subclavian artery (arrow). C: Coronal reformatted CT scan shows a right subclavian artery pseudoaneurysm (arrow) just beyond its origin from the right brachiocephalic artery. D: A more posterior coronal reformatted image shows an acute laceration of the aorta (arrow).
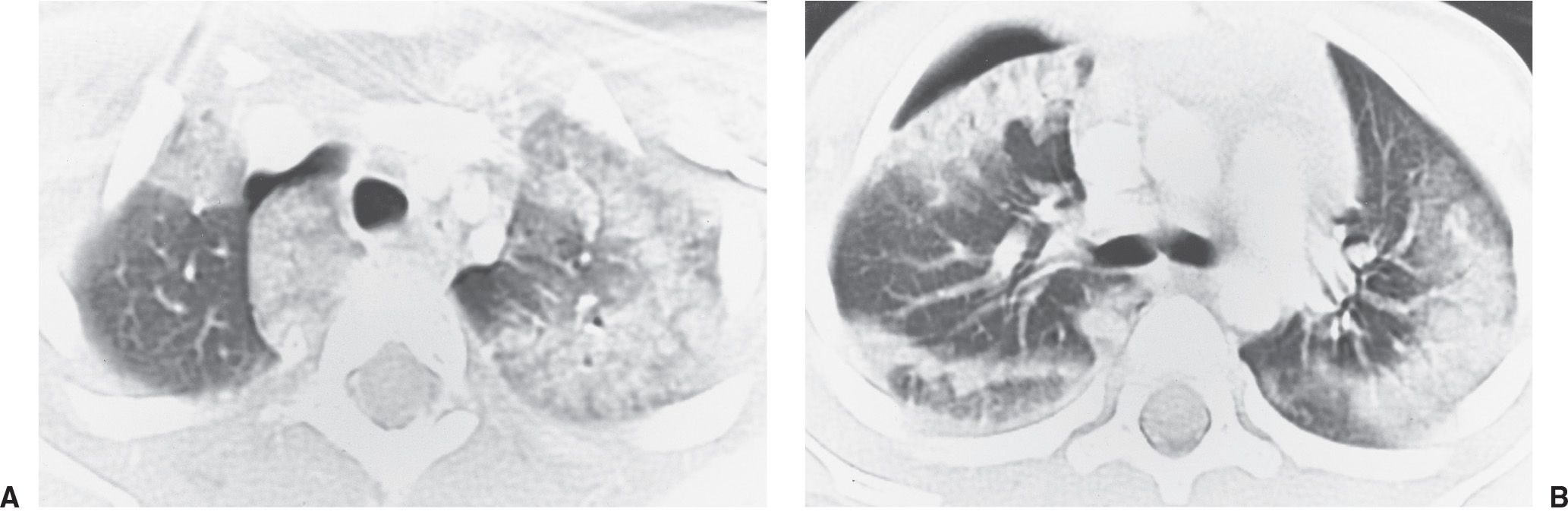
FIG. 8.13 • Pulmonary contusion. A: CT scan of a 4-year-old boy involved in a motor vehicle crash shows bilateral subpleural opacity, an opacified accessory azygos lobe, and a right pneumothorax. B: CT at a level inferior to (A) shows bilateral peripheral, nonsegmental opacities typical of pulmonary contusions. (Reprinted with permission from Collins J. Chest trauma imaging in the intensive care unit. Respir Care. 1999;14(9):1044–1063.)
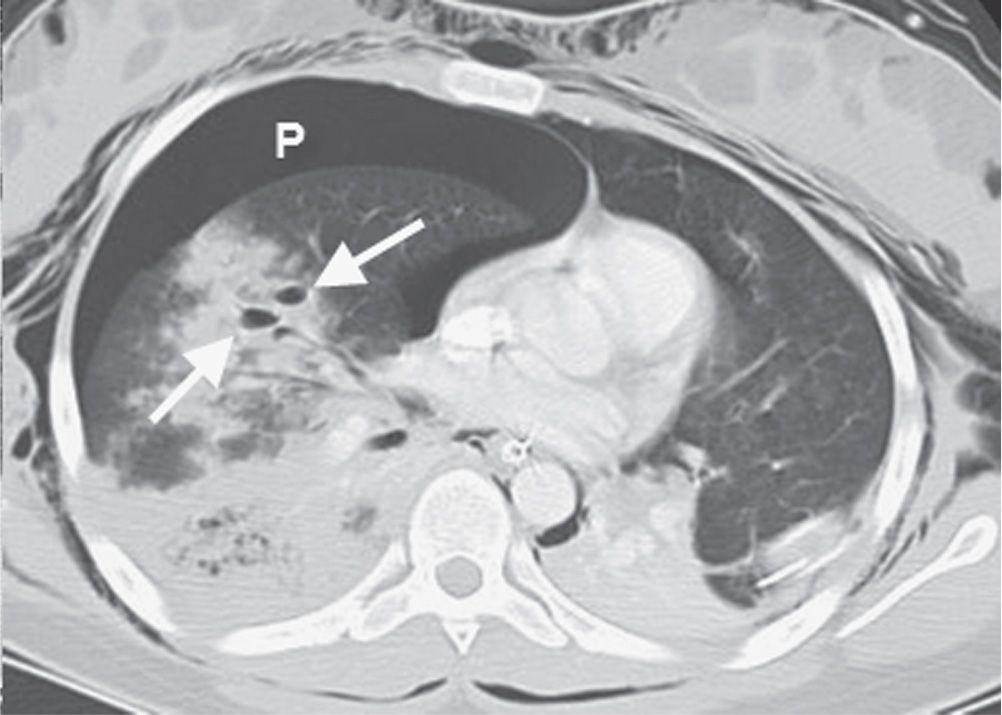
FIG. 8.14 • Pulmonary lacerations. CT scan of a patient involved in a motor vehicle crash shows dense opacity in the right lung with central lucencies (arrows), consistent with lacerations creating pneumatoceles and surrounding hemorrhage. Note a large right pneumothorax (P).
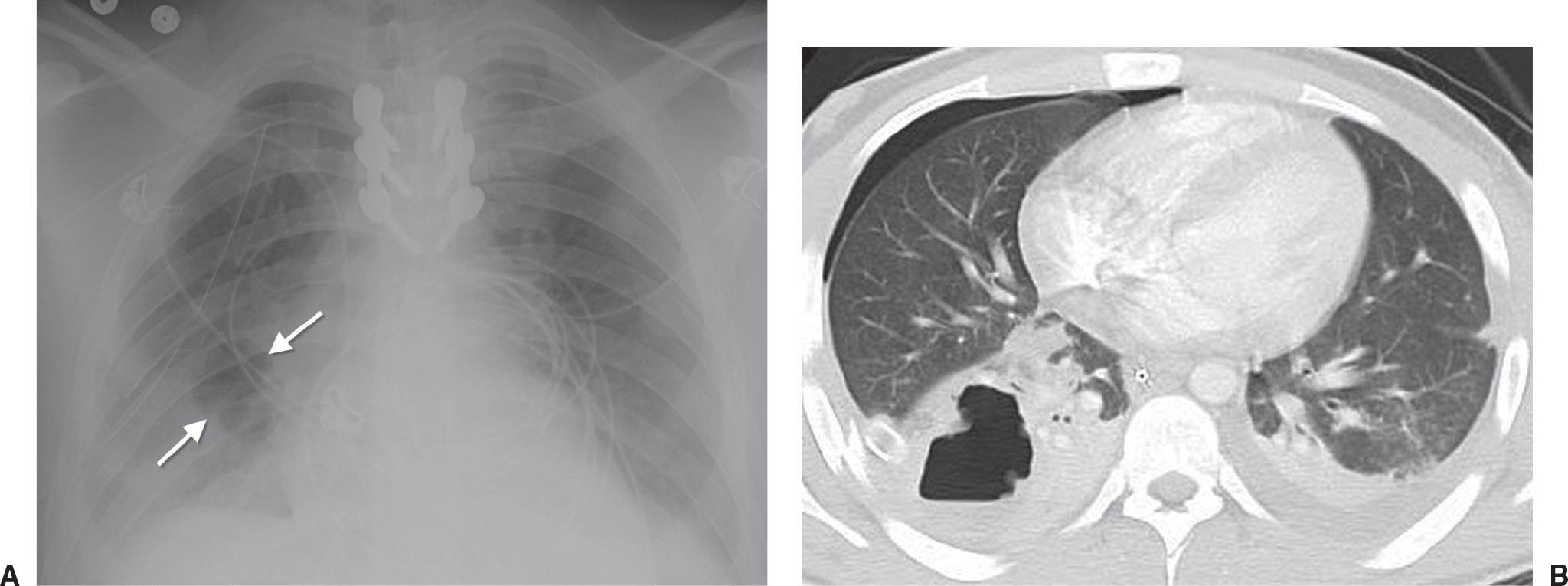
FIG. 8.15 • Pulmonary laceration. A: PA chest radiograph of a 23-year-old man involved in a motor vehicle crash shows airspace opacity in the right lower lung with central lucency (arrows). B: CT scan confirms an area of consolidation with central lucency and air–fluid level, representing laceration, in the right lower lobe, adjacent to a lateral rib fracture. There is also a right pneumothorax.
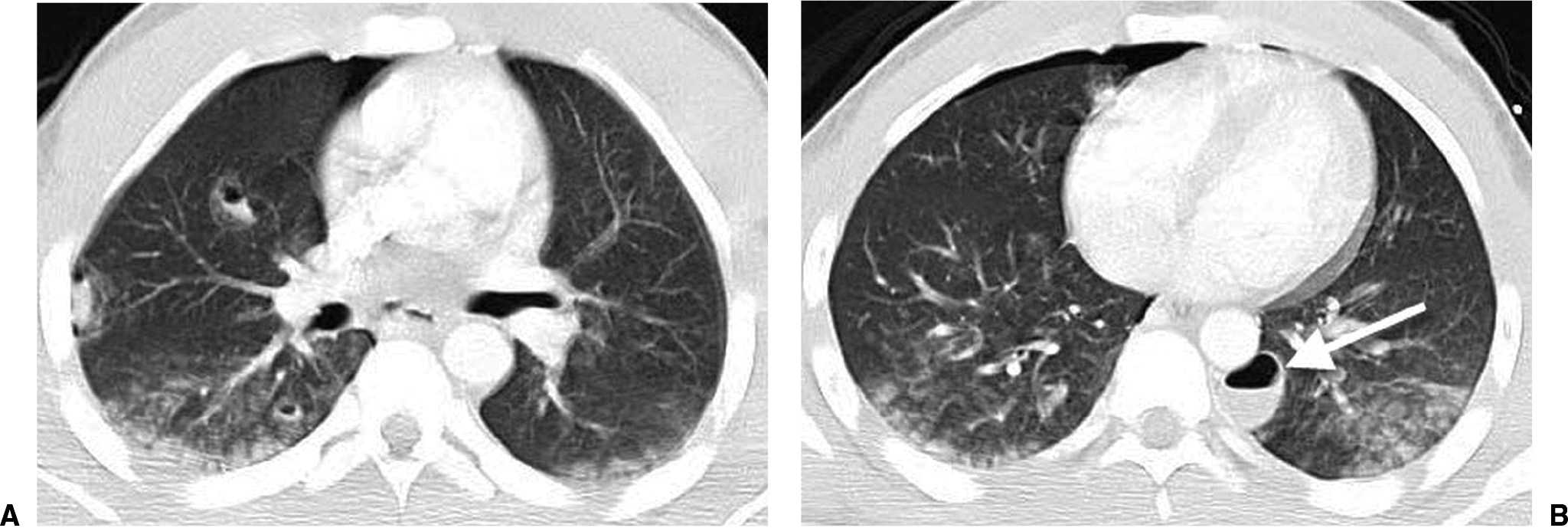
FIG. 8.16 • Pulmonary lacerations. A: CT scan of an 18-year-old man involved in a motor vehicle crash shows numerous airspace opacities with central lucency, consistent with lacerations, in the right lung. B: CT scan at a level inferior to (A) shows a laceration in the left paravertebral area (arrow), typical of a shearing type of pulmonary laceration. This should not be confused with a loculated pneumothorax.
Rupture of the cervical trachea may occur as a “clothesline injury” when the neck is extended on high-speed contact with ropes, wires, or cables by individuals riding many types of recreational vehicles or running. Tracheal laceration may also occur in a motor vehicle crash when the neck of a driver strikes the top of the steering wheel, compressing the airway against the spine.
Pathologically, tracheal injury most commonly presents as a transverse tear between the tracheal rings or a longitudinal tear in the posterior membranous segment. Complete separation of the trachea may occur, but airway continuity can still be maintained by peritracheobronchial tissue. Injury to the mediastinal trachea or major bronchi produces pneumomediastinum that rapidly extends into the neck and face, shoulders, and chest wall (Fig. 8.19). Pneumomediastinum is a more specific sign of TBI than is pneumothorax, because pneumothorax is commonly seen with rib fractures. Pneumothorax is seen in 60% to 100% of cases of TBI (30), but it may not be present if the outer adventitial sleeve of the bronchus remains intact and there is no air leak (31). In most cases, pneumothoraces will respond to chest tube placement, so reexpansion of the lung does not exclude TBI. However, a pneumothorax that does not resolve with functioning tube drainage is the sine qua non of mediastinal central airway injury (32).
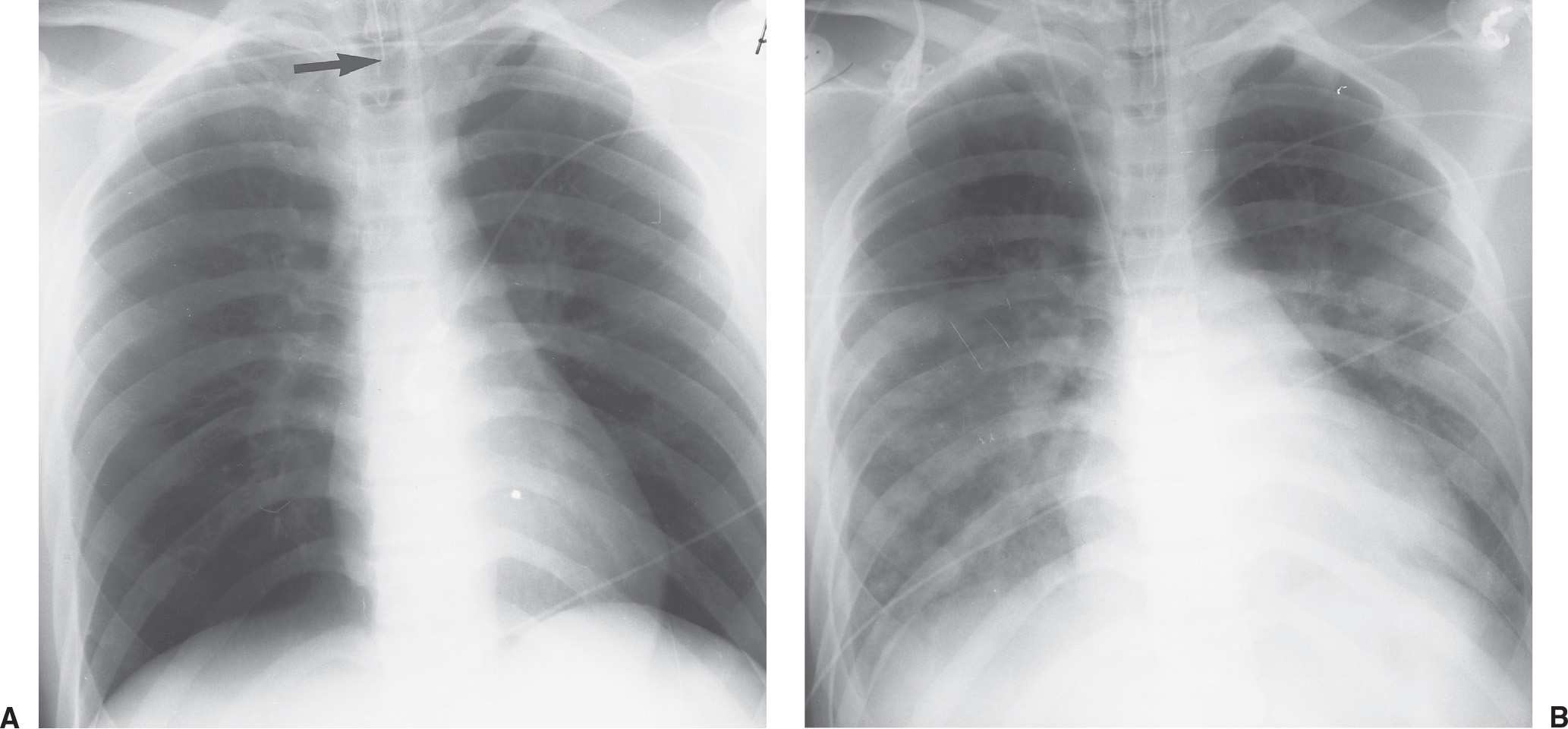
FIG. 8.17 • Fat embolization syndrome. A: AP supine chest radiograph of a young woman shortly after a motor vehicle crash shows clear lungs. The patient sustained multiple long bone fractures that required open reduction and internal fixation. Note the high position of the endotracheal tube (arrow). B: AP supine chest radiograph obtained 72 hours later shows bilateral airspace opacities, with a perihilar and basilar predominance. (Reprinted with permission from Collins J. Chest trauma imaging in the intensive care unit. Respir Care. 1999;14(9):1044–1063.)
An indication of tracheal tear is elevation of the hyoid bone above the level of C3, as seen on a lateral radiograph of the cervical spine (33). This occurs as a result of injured infrahyoid musculature, causing unopposed elevation of the hyoid bone by suprahyoid musculature. Another sign of tracheal transection is acute overdistension of the endotracheal tube cuff, to the point where it exceeds the normal diameter of the trachea (Fig. 8.20). In tracheal rupture, the balloon may approach the endotracheal tube tip as a result of distal expansion of the balloon in the tear, with partial herniation of the balloon in the tear as the tube moves in the airway or is repositioned (34) (Fig. 8.21).
The “fallen lung sign” (35) is a rarely seen but highly suggestive sign of bronchial tear that can be seen on chest radiographs and CT (Figs. 8.22 and (8.23). This sign refers to the lung falling laterally and posteriorly in supine positioning and falling inferiorly away from the hilum in the upright position. Normally with a pneumothorax, the lung recoils inward toward the hilum.
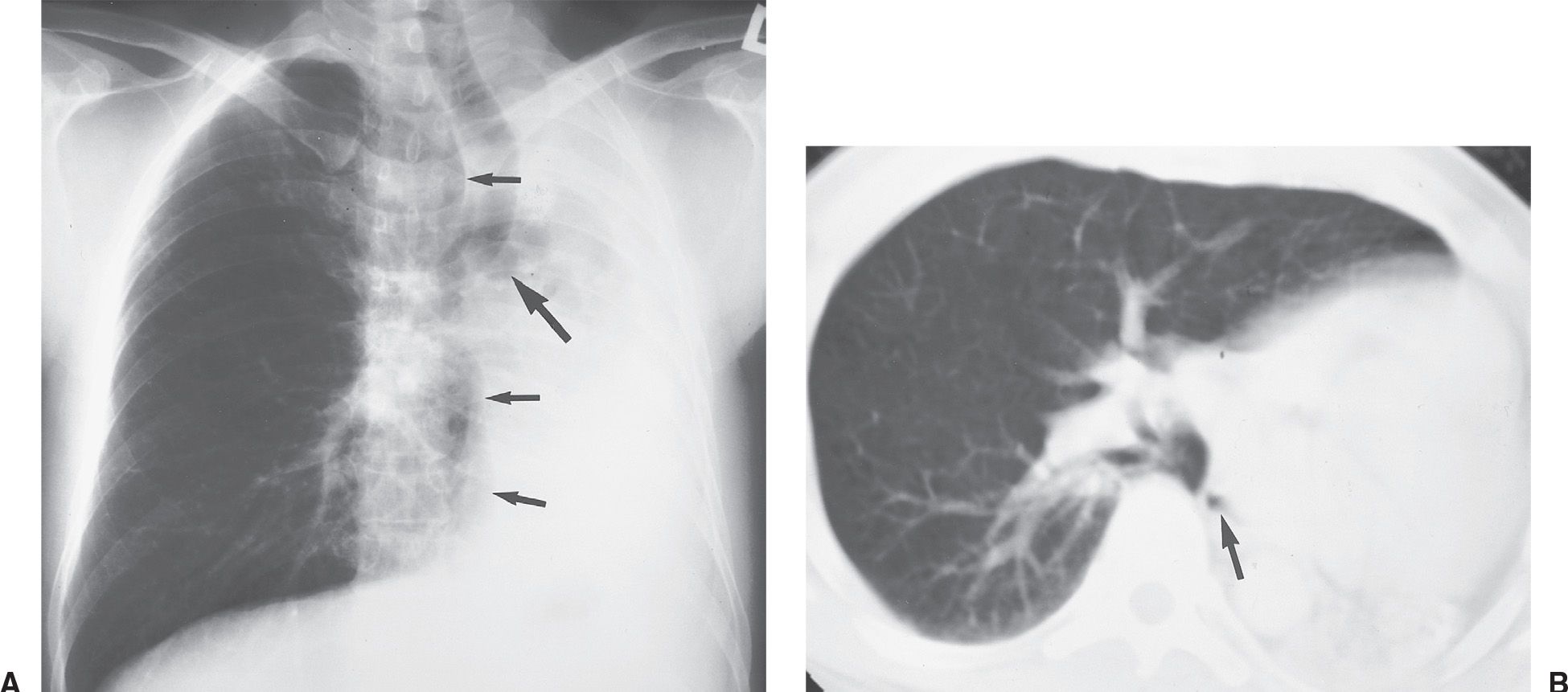
FIG. 8.18 • Remote bronchial fracture. A: PA chest radiograph of an asymptomatic man with a remote history of trauma to the chest shows collapse of the left lung, mediastinal shift to the left (note the position of the trachea), and “cutoff” of the left main bronchus (large arrow). The right lung is hyperinflated (small arrows). B: CT shows collapse of the left lung, cutoff of the left bronchus (arrow), and hyperinflation of the right lung. The fractured bronchus was not recognized at the time of injury, and scarring resulted in total occlusion of the bronchus.
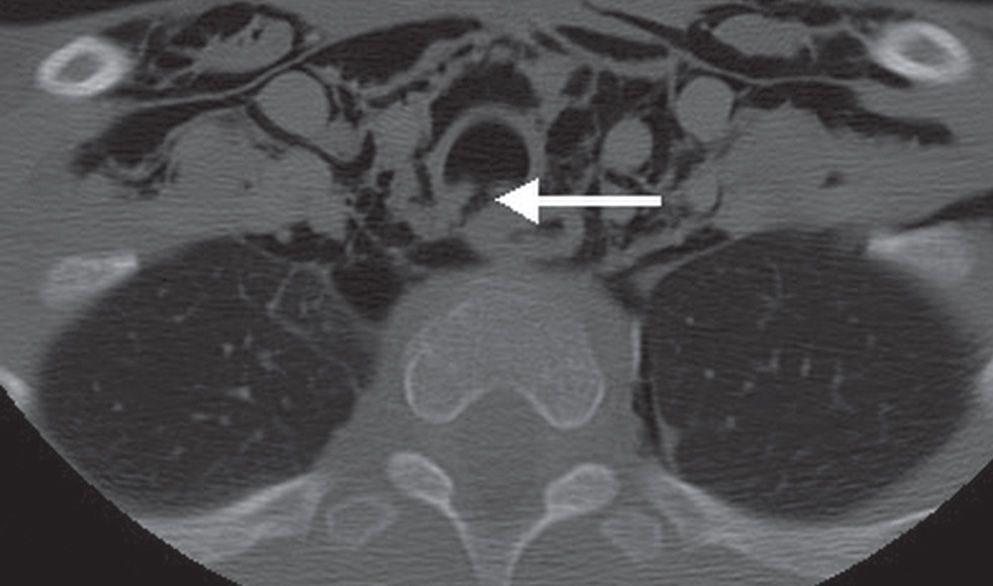
FIG. 8.19 • Acute tracheal injury. A: CT scan of a patient who sustained a handlebar injury to the neck shows a disruption of the posterior membranous trachea (arrow), pneumomediastinum, pneumothorax, and subcutaneous emphysema.
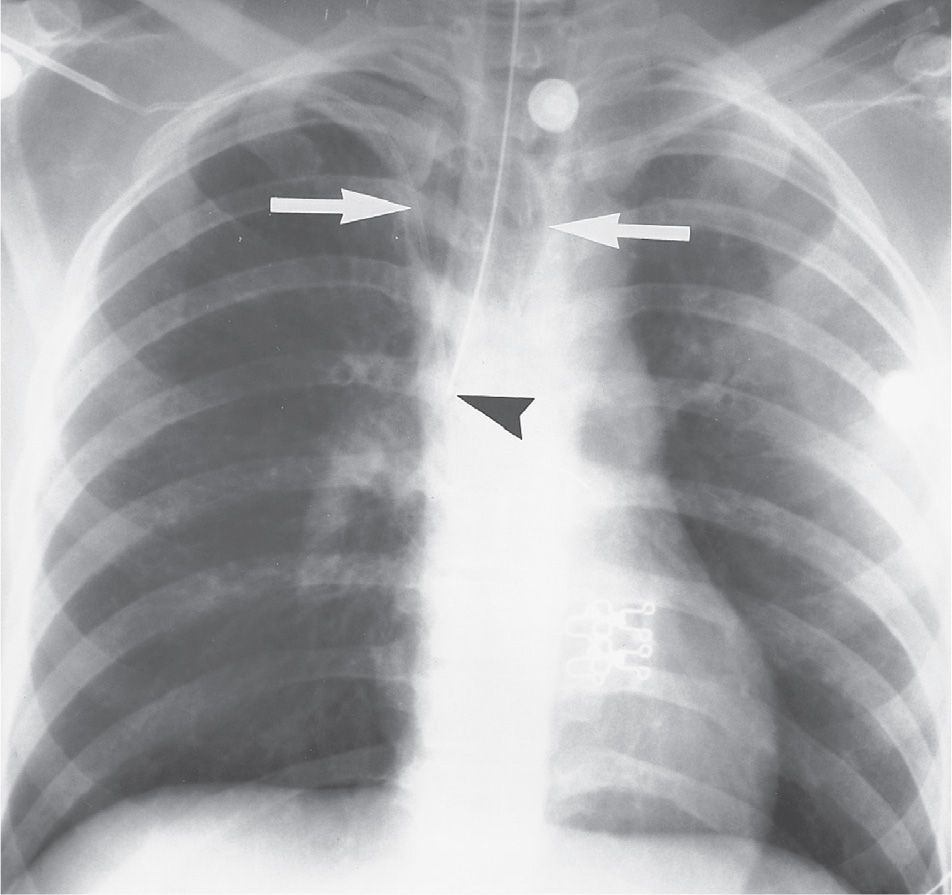
FIG. 8.20 • Tracheal tear. AP supine chest radiograph of a young woman involved in a motor vehicle crash shows an overdistended endotracheal tube balloon (arrows) at the site where the balloon herniates through a tracheal tear. Note the malpositioning of the tube tip within the right bronchus (arrowhead).
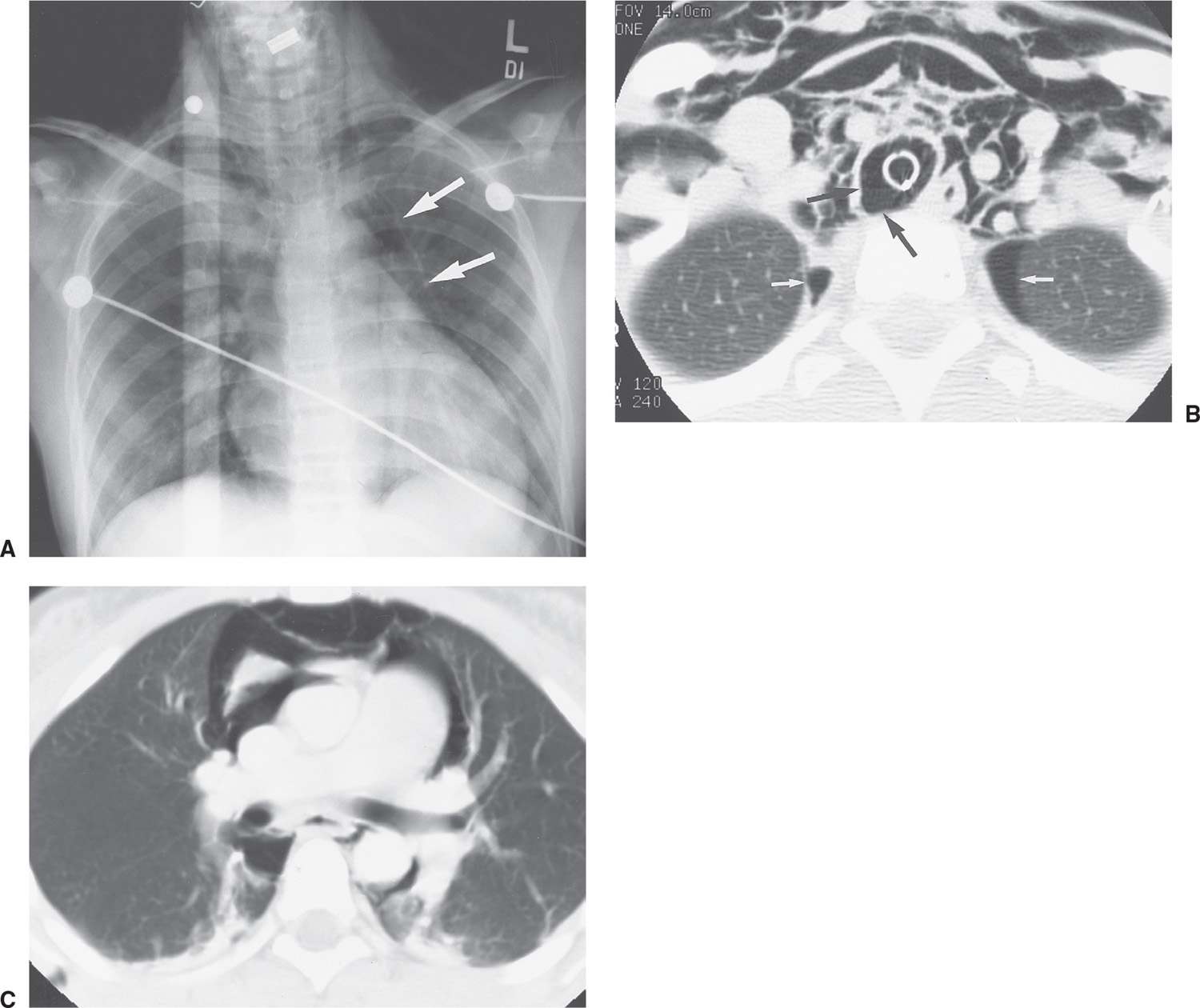
FIG. 8.21 • Tracheal tear. A: AP supine chest radiograph of an 11-year-old girl who impaled her neck on a dumpster bar while riding her bicycle shows linear streaks of air in the chest and neck and lateral displacement of the mediastinal pleura (pneumomediastinum) (arrows). B: CT image shows an overdistended endotracheal tube balloon herniating through a posterolateral tracheal tear (black arrows). The endotracheal tube is seen as a white ring within the trachea. Note the extensive air within the soft tissues of the neck and bilateral pneumothoraces (white arrows). C: CT at a level inferior to (B) shows pneumomediastinum, with air outlining the aorta, superior vena cava, pulmonary artery, and thymus.
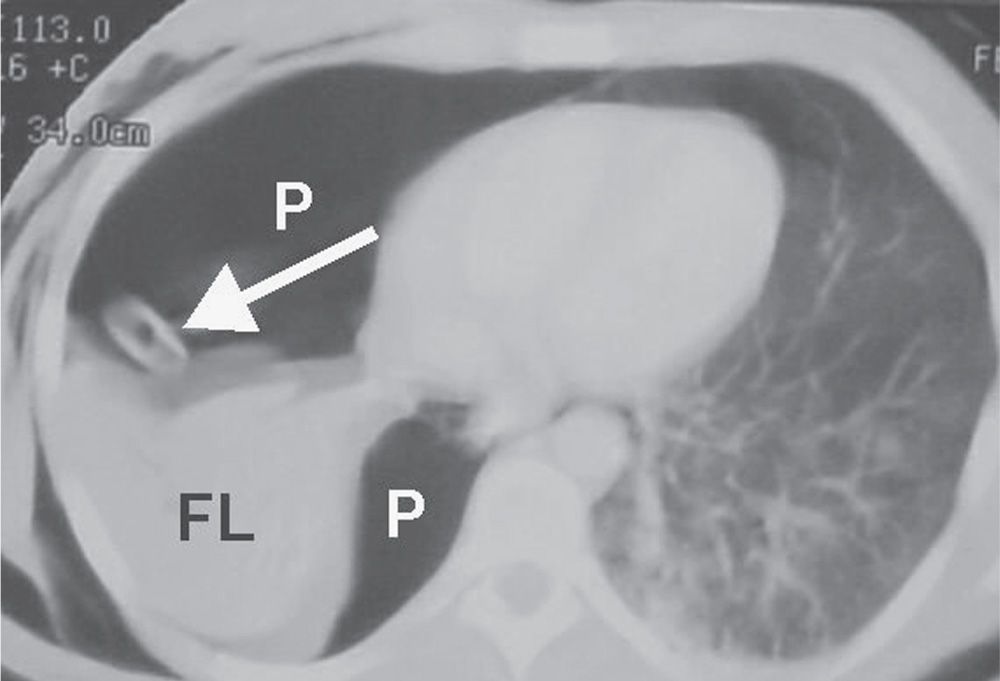
FIG. 8.22 • Fallen lung sign. CT scan of a patient with an acute traumatic fracture of the right main bronchus shows a large right pneumothorax (P), a right chest tube (arrow), and collapsed “fallen right lung” (FL) positioned in the posterior and lateral right hemithorax. Normally with pneumothorax, the collapsed lung recoils inward toward the hilum.
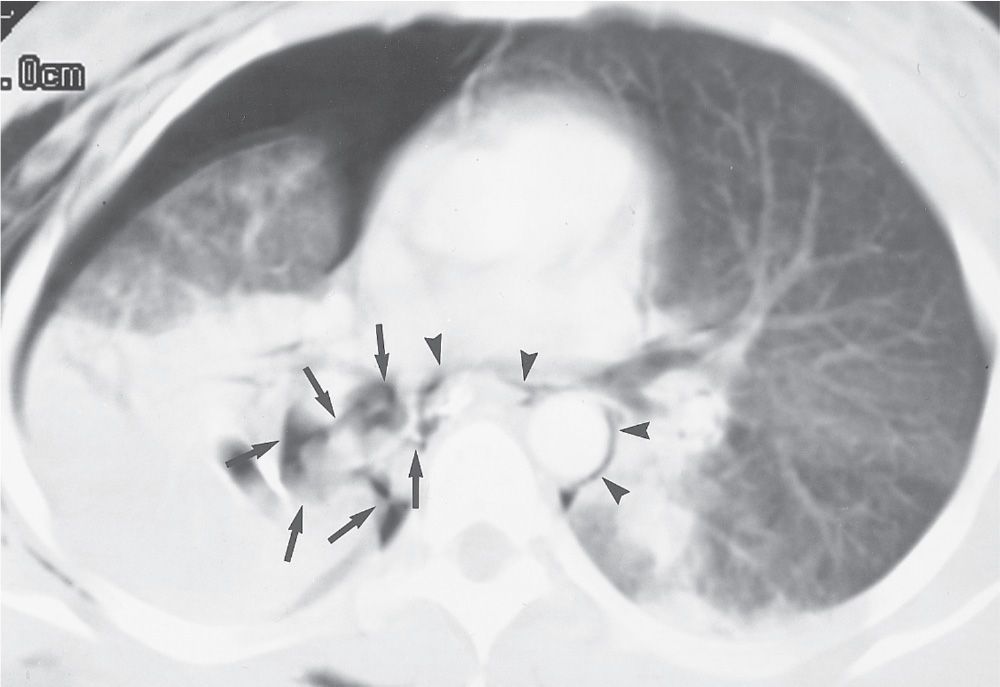
FIG. 8.23 • Fractured bronchus intermedius. CT of a young woman involved in a motor vehicle crash shows leakage of air from a fractured bronchus intermedius to the pleural space (arrows) and mediastinum (arrowheads), resulting in pneumothorax and pneumomediastinum, respectively. (Reprinted with permission from Collins J. Chest trauma imaging in the intensive care unit. Respir Care. 1999;14(9):1044–1063.)
DIAPHRAGM RUPTURE
Acute diaphragmatic rupture occurs in 1% to 7% of patients following major blunt trauma (36–38), and the diagnosis is missed on initial presentation in up to 66% of patients (39–45), sometimes as a result of the positive intrathoracic pressure of mechanical ventilation preventing the ascent of intra-abdominal contents through a lacerated hemidiaphragm. Seventy-five percent to 95% of patients with acute diaphragm rupture have abnormal chest radiographs, but only 17% to 40% have highly suggestive radiographic findings (46–48). Chest radiographic findings of rupture include a normal-appearing diaphragm, pneumothorax, displacement of stomach, liver, spleen, colon, or small bowel into the thorax (Fig. 8.24), superior displacement of an intragastric nasogastric tube (Fig. 8.25), pleural effusion, basilar lung opacity causing inability to visualize the diaphragm, apparent elevation of the diaphragm, an irregular or lumpy diaphragm contour, fractures of the lower ribs, and contralateral shift of the mediastinum in the absence of a large pleural effusion or pneumothorax (Table 8.2) (49). Rupture of the right hemidiaphragm probably occurs with almost the same frequency as rupture of the left hemidiaphragm, although most clinically recognized diaphragm injuries occur on the left. If diaphragm rupture is not promptly diagnosed, the patient may remain asymptomatic or develop incarceration of herniated abdominal viscera, which can occur at a time remote from the incidence of trauma (Fig. 8.26).
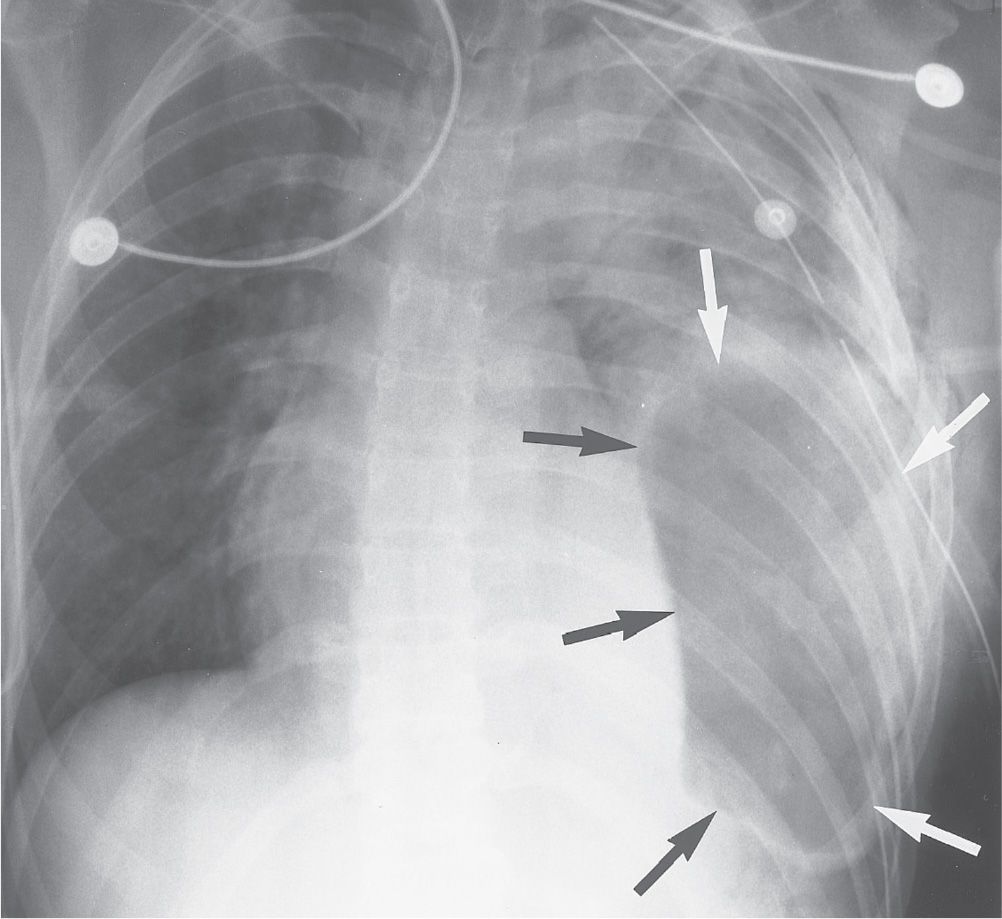
FIG. 8.24 • Diaphragm rupture. AP supine chest radiograph of a 24-year-old woman involved in a motor vehicle crash shows herniation of gas-distended stomach through a left diaphragmatic tear into the left hemithorax (black and white arrows). Note the shift of the mediastinum to the right, left rib fractures, and opacification of the left lung from parenchymal injury.
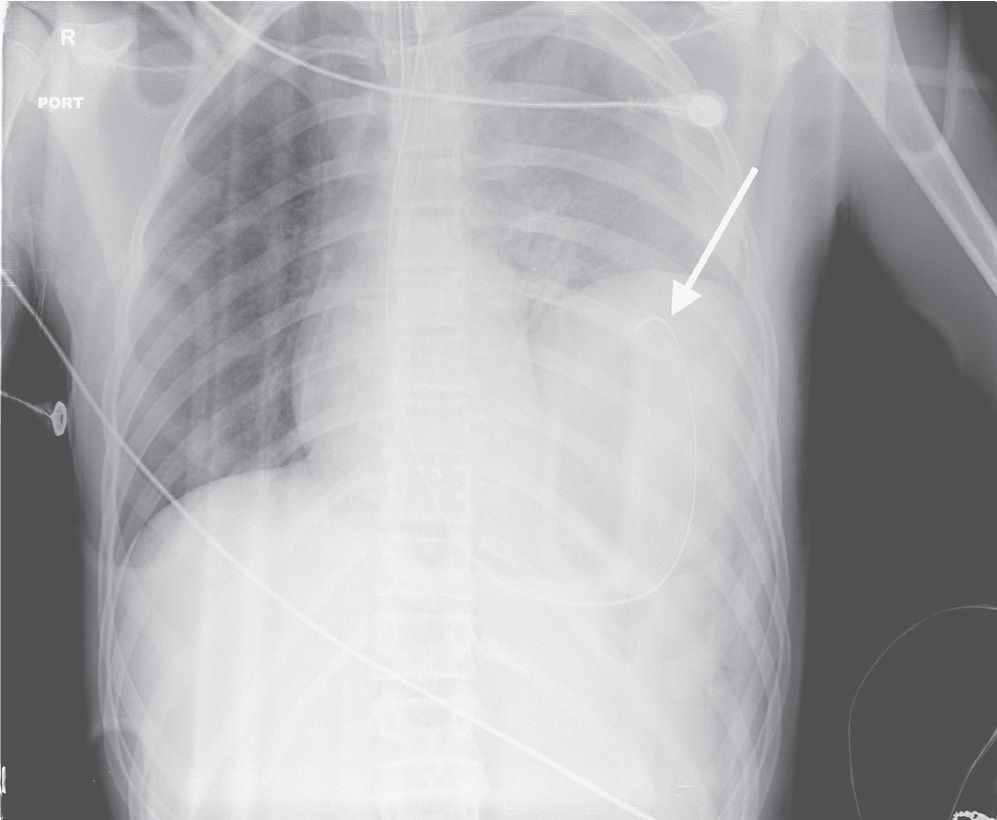
FIG. 8.25 • Diaphragm rupture. AP supine chest radiograph of a patient involved in a motor vehicle crash shows a mass in the left lower hemithorax representing herniated non–air-filled stomach, superior displacement of an intragastric nasogastric tube (arrow), and rightward shift of the mediastinum.
Table 8.2 RADIOLOGIC FINDINGS OF DIAPHRAGM RUPTURE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree