CHAPTER 21
Fetal Arrhythmias
Definition
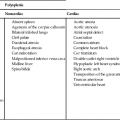
Fetal cardiac arrhythmias occur in up to 1% to 3% of all pregnancies and account for 10% to 20% of referrals to fetal cardiologists.1–4 The majority of fetal arrhythmias are benign; however, they can be an important cause of fetal morbidity and death.5 The normal fetal heart rate is regular and between 100 and 180 beats per minute.6 Fetal arrhythmias are therefore defined as those that are irregular or outside the normal range. Clinically, fetal arrhythmias can be classified as those with an irregular but overall normal rate, tachycardia, and bradycardia.7 The approach to diagnosing prenatal arrhythmias is significantly different from that used in the postnatal period because of the difficulty in distinguishing fetal electrocardiographic (ECG) signals from maternal cardiac signals.
Embryology
Spontaneously depolarizing cells, which give the heart its unique characteristic of automaticity, are present early in gestation in all parts of the developing heart. Rhythmic contraction of the fetal heart begins 21 to 22 days after conception and is present before the conduction system is established.8 The conduction system of the fetal heart is functionally mature by 16 weeks of gestation.9 The heart rate changes throughout gestation. Initially, the rate is slow (82 beats per minute), increasing to 177 beats per minute at 63 days and then decreasing to 147 beats per minute at 15 weeks of gestation.10,11 After 34 weeks of gestation, fetal heart rate patterns are related to fetal rest and activity.12 Fetal heart rate control is through the parasympathetic and sympathetic nervous systems.13 The conduction system of the heart consists of the sinus node, atrioventricular node, bundle of His, and Purkinje fibers. The pacemaker of the heart is the sinus node. The electrical signal travels down specialized conduction tissue through the atria to the atrioventricular node, where conduction of the signal is slowed. The signal is then sent through the bundle of His to the Purkinje fibers, which initiate ventricular contraction.
Occurrence Rate
The number of fetuses referred for evaluation of arrhythmias varies among institutions. Fouron14 reported that approximately 14% of the 1450 fetuses seen annually at St Justine Hospital were referred for arrhythmia. Over a 5-year study period at that institution, 584 of the 940 fetuses referred for apparent arrhythmia were in sinus rhythm at the time of their echocardiographic examinations. Among the 356 fetuses with sustained fetal arrhythmias, premature atrial or ventricular contractions were noted in 86%, tachycardia in 8%, and bradycardia in 5%.14 Copel et al15 reported that 10% to 12% of the referrals for fetal echocardiography at Yale are due to fetal arrhythmias; of the 595 fetuses referred to Yale for irregular heart rhythm over a 10-year period, 55% had normal rhythms, 43% had extrasystoles, and 2.4% had hemodynamically significant arrhythmias.
Irregular Fetal Rhythms
Irregular heart rhythms are generally detected during routine obstetrical auscultation of the fetal heart, most commonly between 28 and 32 weeks’ gestation, but can be noted as early as 17 weeks. Premature atrial contractions (PACs) account for the majority of irregular fetal rhythms.1,2 PACs in the fetus are generally idiopathic; however redundancy of the foramen ovale flap (Fig. 21–1) has been reported to possibly contribute to initiation of an ectopic atrial focus.16
Maternal consumption of nicotine, caffeine, or alcohol has also been implicated.17 Isolated ectopic beats are associated with congenital heart defects in up to 1% to 2% of cases.2
PACs generally present as irregular pauses detected by routine obstetrical auscultation and are usually transient and benign.18–20 They may increase as pregnancy progresses. Premature beats become significant when they occur with appropriate timing to initiate sustained tachycardia.21 Progression to sustained tachycardia can occur in up to 2% to 3% of cases of frequent atrial ectopy, either in utero or in the first 3 to 4 weeks of life.22,23 Those cases in which there are multiple blocked atrial ectopic beats causing a low ventricular rate appear to be at higher risk of progressing to tachycardia than do those with a normal ventricular rate.2 The risk increases to approximately 10% with complex ectopy, including couplets or triplets.24 Progression of PACs to sustained tachycardia is generally mediated by anatomic bypass tracts and leads to supraventricular tachycardia (SVT), but atrial flutter may also occur.23 Less commonly, premature ventricular contractions (PVCs) may cause an irregular fetal heart rhythm; the ratio of occurrence of PACs to PVCs in utero is approximately 10 : 1.5 PVCs may be difficult to distinguish from PACs in utero. A premature ventricular beat that is not preceded by a premature atrial beat should be interpreted as a PVC. The presence of atrioventricular valve regurgitation concurrent with the ectopic beat, less prominent flow reversal in the inferior vena cava by Doppler imaging, and a longer compensatory pause can be helpful to differentiate PVCs from PACs.2–4 The presence of PVCs may be benign but warrants exclusion of myocardial disease, intracardiac tumors, and any evidence of cardiac decompensation.
Tachyarrhythmia
Fetal tachycardia is defined as a sustained heart rate that exceeds 180 beats per minute. The fetal myocardium is intrinsically more susceptible to sustained tachycardia as a result of impaired diastolic relaxation and compliance. The inherent diastolic dysfunction of the fetal myocardium is thought to be at least in part due to immature structure and function of the sarcoplasmic reticulae.25,26 The most common forms of fetal tachycardia are SVT (66%–90%) and atrial flutter (10%–30%).27
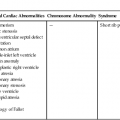
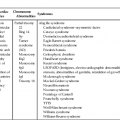
Fetal SVT is characterized by a regular fast rate with a 1 : 1 ratio of atrioventricular conduction. The heart rate in SVT is monotonous with no variation in the atrial or ventricular rate, in contrast to sinus tachycardia in which there is heart rate variability. Sinus tachycardia is generally a result of maternal or fetal distress, and identifying the underlying cause is of primary importance.28 Atrial flutter and fibrillation are rare fetal arrhythmias characterized by very fast atrial rates, often 300 to 500 beats per minute, with an irregular slower ventricular rate resulting from variable conduction delay, generally 2 : 1 or 3 : 1 block.29 Atrial flutter is associated with structural heart defects, chromosomal anomalies, or other pathological states in 30% of cases.5
Ventricular tachycardia is extremely rare in fetal life. It can, however, be present in association with long QT syndrome, which is a genetic syndrome involving ion channel abnormalities and increased risk of sudden death. Magnetocardiography has been the only definitive way to measure the QT interval in the fetus30,31; given the limited availability of this technique, the diagnosis is generally made in the postnatal period. Fetuses with long QT syndrome often present with sinus bradycardia between periods of tachycardia, which may facilitate determination of the diagnosis.32,33
Bradyarrhythmia
Fetal bradycardia is defined as a sustained heart rate less than 100 beats per minute. The most common causes of fetal bradycardia are blocked premature atrial beats, atrioventricular block, and sinus bradycardia.5 Transient bradycardia is common and is often associated with fetal vagotonia due to pressure on the maternal abdomen from the ultrasound probe, which resolves with removal of the transducer. Cord compression, which may occur when the umbilical cord is located around the fetal neck, may also result in a transient bradycardia (Fig. 21–2).
Bradycardia may be due to nonconducted premature atrial beats (blocked PACs). Most commonly this occurs with atrial bigeminy in which every other beat is premature and is blocked in the atrioventricular node, causing the ventricular rate to appear slow. Blocked PACs are usually benign and self-limited. The most important cause of sustained fetal bradycardia is complete atrioventricular block. Fetal heart block can be detected as early as the first trimester, endovaginally, with two-dimensional and color Doppler flow imaging.34 Complete heart block occurs in 1 : 20,000 newborns,34 but the overall incidence of fetal heart block is unknown. In complete heart block there is complete dissociation between the atrial and ventricular beats. It is important to distinguish pathological bradycardia resulting from complete heart block from benign blocked PACs. In complete heart block, the atrial rate is regular, whereas in blocked PACs the atrial rate is irregular, with every other beat occurring prematurely.
Complete heart block may be associated with structural heart defects involving the atrioventricular junction (atrioventricular discordance as in congenitally corrected transposition of the great arteries) or visceral heterotaxy syndrome with left atrial isomerism.35–37 Alternatively, complete heart block may be immune mediated in the setting of maternal connective tissue disorders such as systemic lupus erythematosus or Sjögren syndrome with elevated anti-SS-A or anti-SS-B antibodies. These antibodies may cross the placenta as early as 16 weeks’ gestation and cause inflammatory injury of the fetal atrioventricular node.21 Cardiac structure is generally but not always normal in the setting of immune-mediated complete atrioventricular block. These fetuses may also have autoimmune myocarditis from damage to cardiac contractile elements.
Fetal sinus bradycardia is marked by a regular slow rate with 1 : 1 atrioventricular conduction and may be due to cardiac structural defects (primarily left atrial isomerism) or prolonged QT syndrome or may be an isolated finding. Sinus bradycardia is usually the result of maternal or fetal distress. As with sinus tachycardia, determining the underlying cause is the most important aspect of the diagnosis.28
Sonographic Criteria
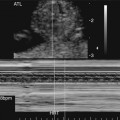
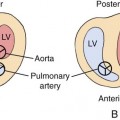
Analysis of fetal cardiac rhythm is based on the ability to record atrial and ventricular activity simultaneously. M-mode imaging was one of the first echocardiographic modalities used in assessing arrhythmias. Because of the high temporal resolution, it remains an important part of arrhythmia assessment. Electrical events are inferred from the motion of the cardiac chambers.38 M-mode imaging is performed by aligning the cursor through one of the atrial and one of the ventricular walls from a four-chamber view (Fig. 21–3) or with the cursor between the left atrium and aorta from a short-axis view of the great vessels (Fig. 21–4).
Atrial extrasystoles, the most common form of arrhythmia, can be readily assessed by M-mode imaging. The premature atrial beats may be conducted to the ventricle or blocked in the atrioventricular node. If the PAC is conducted, it is followed by ventricular contraction and then a pause during which the sinus rate is reset (Fig. 21–5). If the PAC is blocked within the atrioventricular node, no ventricular contraction occurs (Fig. 21–6). M-mode imaging can help differentiate blocked PACs from pathological causes of bradycardia, such as complete heart block. In atrial bigeminy with block, every other atrial contraction is premature and not conducted to the ventricle; the atrial rate appears irregular (Fig. 21–7). The atrial rate in complete heart block by contrast is very regular (Fig. 21–8).
In the setting of tachycardia, the 1 : 1 atrioventricular relationship seen in SVT is well demonstrated by M-mode imaging (Fig. 21–9); however, this must be distinguished from atrial flutter with 1 : 1 conduction. With SVT, the heart rate is maintained between 180 and 300 beats per minute. With atrial flutter, the atrial rate will be between 300 and 400 beats per minute, permitting the differentiation (Fig. 21–10). Atrial fibrillation is defined as an atrial rate greater than 400 beats per minute; however, it is rarely seen in the fetus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree