Metastases
Melissa L. Rosado-de-Christenson, MD, FACR
Key Facts
Terminology
Lung most common site of metastases
Pathways: Hematogenous, lymphatic, endobronchial
Imaging Findings
Multifocal bilateral pulmonary nodules
Peripheral, basilar predominant
Variable size
Spherical shapes; smooth, lobular, or irregular margins
Ground-glass opacity and mixed attenuation nodules
Lymphangitic carcinomatosis
Smooth or nodular thickening of interlobular septa
Peribronchovascular thickening
Rare: Solitary nodule, cavitation, calcification
Top Differential Diagnoses
Multifocal Pulmonary Nodules
Vasculitis, septic emboli, lymphoma
Lymphangitic Carcinomatosis
Sarcoidosis, silicosis
Pathology
Mechanical arrest model: Metastases are 1st established in filtering organ
Environmental model: Metastases occur in environments favorable for growth
Clinical Issues
Death from malignancy usually attributable to metastatic disease
Metastasectomy for early metastases to prevent systemic disease
TERMINOLOGY
Definitions
Metastasis: Spread of disease from 1 organ to another nonadjacent organ or body part
Used to describe spread of malignant neoplasms and infections
Ability to metastasize is hallmark of malignancy
Metastatic pathways: Hematogenous, lymphatic, and endobronchial
Proposed mechanism of hematogenous metastases
Invasion of vascular structures by tumor cells
Transport of tumor cells in bloodstream
Arrest of tumor cells in filtering organ
Adherence to vessel walls and subsequent extravasation into tissues
Micrometastasis
Lung is most common site of metastases: Up to 50% at autopsy
Filtering organ; receives systemic venous drainage
“Seed and soil” hypothesis of chemokine-modulated “homing” of tumor cells to specific organs
IMAGING FINDINGS
General Features
Best diagnostic clue: Multifocal bilateral pulmonary nodules &/or masses
Patient position/location
Lung bases
Lung periphery; subpleural; outer 1/3 of lung
Size: Variable; 2-4 mm (miliary) to several centimeters
Morphology
Spherical with smooth margins
Also lobular and irregular-shaped
CT Findings
Multifocal bilateral pulmonary nodules and masses
More numerous in lung bases (dominant pulmonary arterial flow) and subpleural lung periphery (outer 1/3)
Variable size
Miliary nodules: Thyroid cancer, renal cell cancer, and melanoma
Large masses: Sarcomas, colon, and renal cancer
Morphology: Typically spherical
Margins: Well defined, smooth, lobular, irregular
Attenuation: Typically solid nodules
Ground-glass nodules: Hemorrhagic metastases, endobronchial dissemination, metastatic adenocarcinoma
Mixed attenuation nodules: Solid nodule surrounded by ground-glass; CT halo sign
Random or uniform distribution of nodules with respect to normal structures
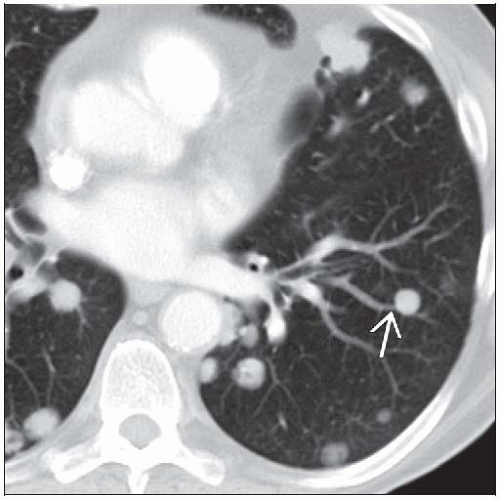
Feeding vessel sign; association of nodule with pulmonary artery
Variable attenuation
Most are solid nodules
Ground-glass nodules: Metastatic adenocarcinoma
Nodules with surrounding ground-glass; hemorrhagic lesions
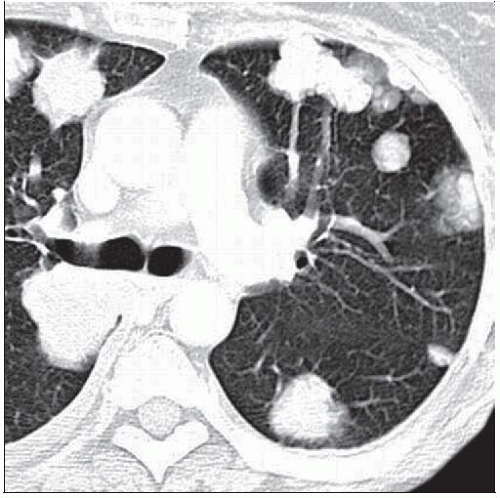
Lymphangitic carcinomatosis
Advanced adenocarcinoma
Hematogenous or lymphatic dissemination
Smooth &/or nodular thickening of interlobular septa
Peripheral reticular opacities
Central polygonal arcades
Thickening of peribronchovascular interstitium
Prominent central dot; thick centrilobular bronchovascular bundle
Asymmetric involvement (50%)
Normal pulmonary architecture
Lymphadenopathy (30-50%), pleural effusion (30%)
Unusual manifestations
Solitary nodule (2-10%)
Colon and kidney primaries, melanoma, sarcoma
New primary lung cancer must be excluded
Cavitation (4%): Typically from central necrosis
Cavity walls usually thick and nodular
Squamous cell carcinomas: Head & neck and cervical cancer
Adenocarcinomas and sarcomas
Treated metastases
Metastatic osteosarcoma may result in spontaneous pneumothorax
Calcification typically in bone-forming neoplasms
Osteosarcomas, chondrosarcomas; also mucinous adenocarcinomas
Endobronchial metastases (2%)
Typically renal cell carcinoma; also melanoma, breast cancer
May mimic central primary lung cancer
May produce mucus plugs, atelectasis, postobstructive pneumonia
Intravascular tumor emboli
2.5% of autopsied malignancies
Occlusion and enlargement of pulmonary arteries by tumor
Branching nodular enlargement of small and medium-sized pulmonary arteries
Other thoracic metastases
Pleural metastases
Pleural effusion, exudate, may be large
Solid pleural nodules
Pleural effusion and solid pleural nodules
Circumferential nodular pleural thickening
Lymphadenopathy
Genitourinary, breast, head and neck primaries, melanoma
Typically right paratracheal; other lymph node groups affected
Radiographic Findings
Pulmonary nodules
Multifocal, bilateral, lower lobe predominant
Well-defined or ill-defined margins
Variable size
Rarely: Solitary nodule, calcification, cavitation, endobronchial metastasis
Lymphangitic carcinomatosis
Asymmetric reticular opacities
Thick interlobular septa; Kerley B lines
Pleural effusion; lymphadenopathy
Pleural metastases
Pleural effusion
Pleural masses
Circumferential nodular pleural thickening
Mediastinal lymphadenopathy
Nuclear Medicine Findings