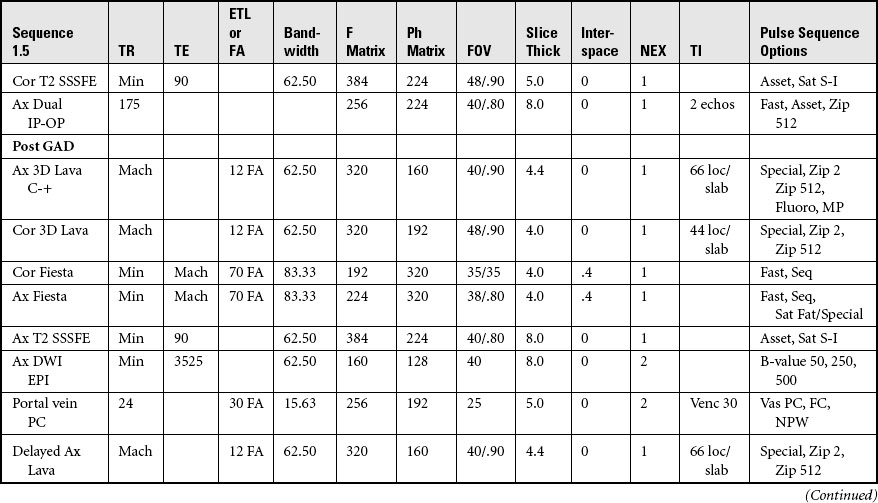
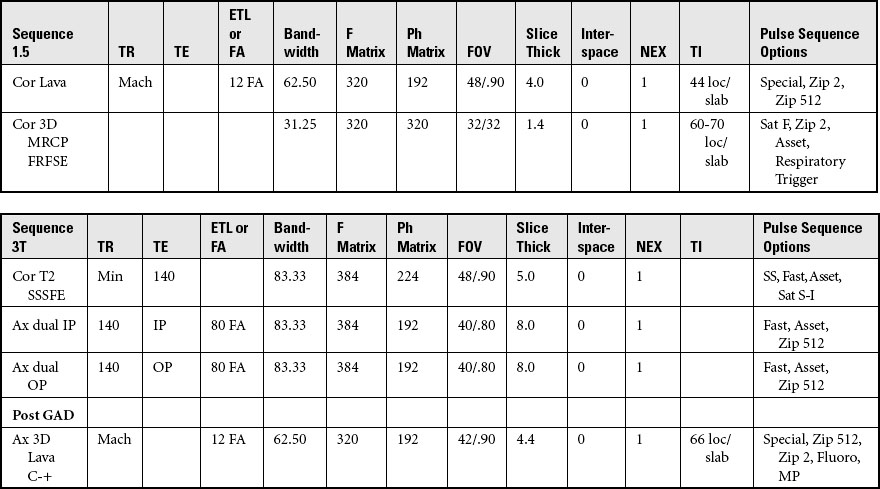
CHAPTER 6 MRI of the Abdomen and Pelvis
MRI of the abdomen and pelvis—considerations
Scan Considerations
Refer to all vendor-specific safety parameters.
Ensure that the patient empties their bladder before scanning.
• They allow for assessment of adequate anatomical coverage.
• They permit image review for asset artifacts in the FOV.
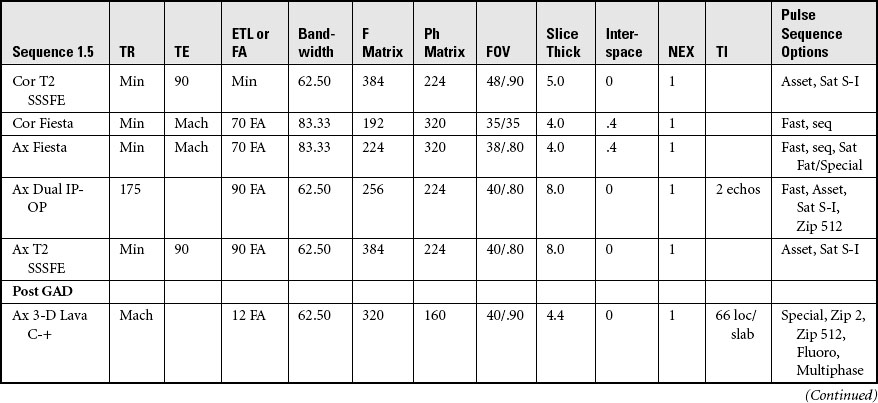
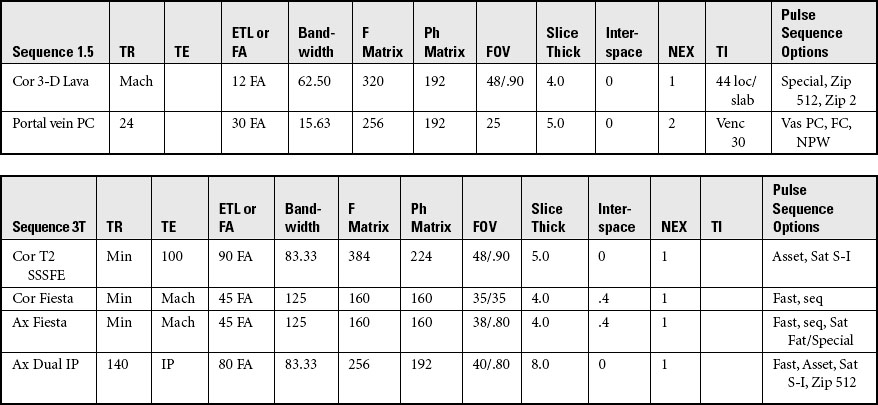
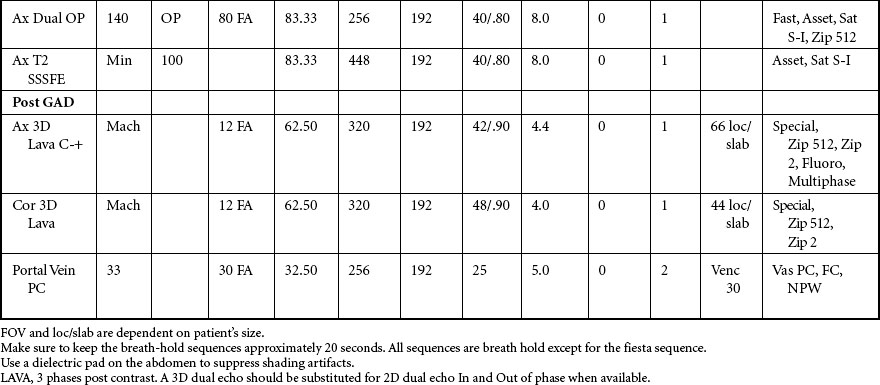
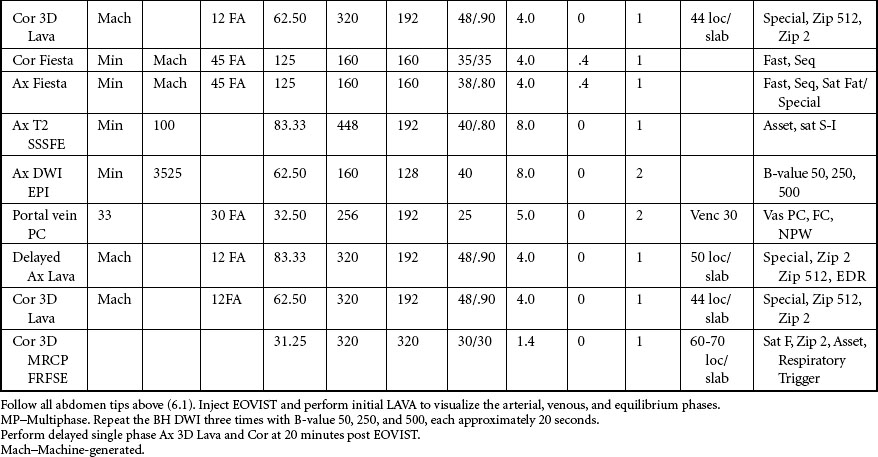
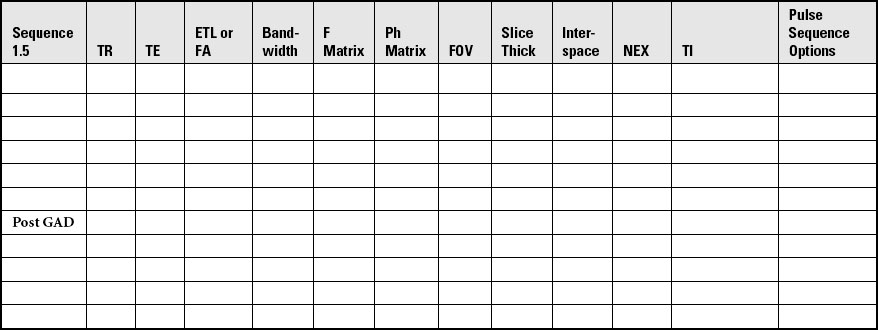
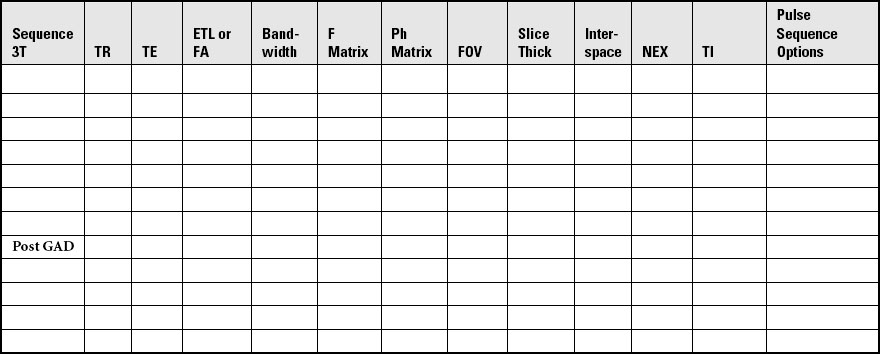
MRI of the abdomen—kidneys
Acquire three-plane pilot of the abdomen and pelvis per site specifications.
COIL: Multi-channel or 12-channel torso array or multi-channel cardiac coil
SPECIAL CONSIDERATIONS: Position respiratory bellows on the patient before starting the scan at the level of the diaphragm. Position a diaelectric pad on the abdomen to help suppress shading artifacts.
POSITION: Supine, feet first, with coil covering diaphragm to iliac crest
Place patient’s arms over the head or elevated on cushions away from the body.
LANDMARK: Midline, 4 inches above the iliac crest.
IMMOBILIZATION: Place a cushion under the patient’s knees.
Prevent the body from touching the sides of the magnet by using sponges or sheets.
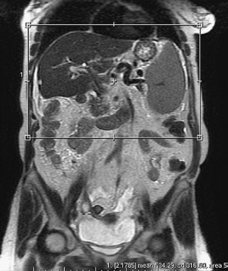
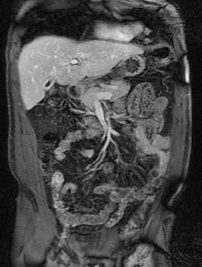
Acquisition of Coronal Images of the Abdomen
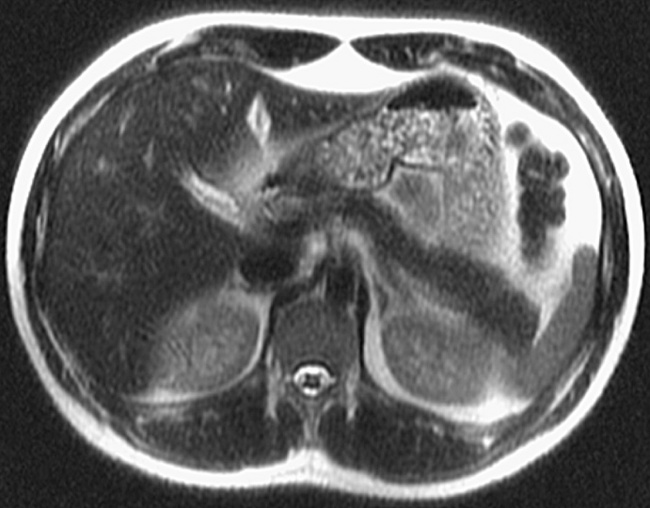
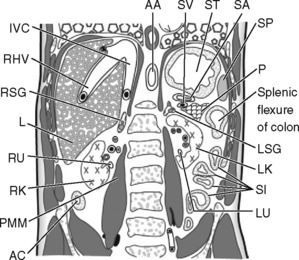
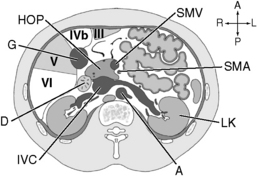
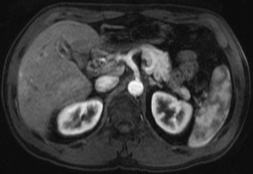
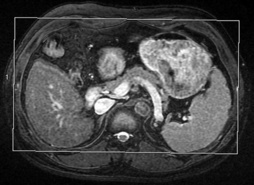
Acquisition of Axial Images of the Abdomen
SLICE ACQUISITION: Superior to inferior
SLICE ALIGNMENT: Straight; no angulation of slices is necessary.
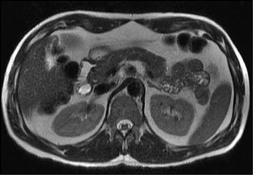
Acquisition of the Axial 3-D LAVA Images of the Abdomen
SLICE ACQUISITION: Superior to inferior
SLICE ALIGNMENT: Straight; no angulation of slices is necessary.
ANATOMIC COVERAGE: From diaphragm to the lower poles of the kidneys
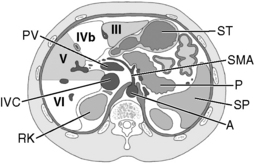
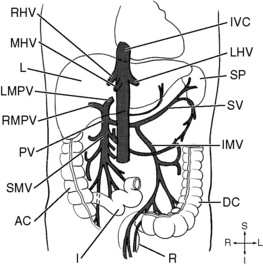
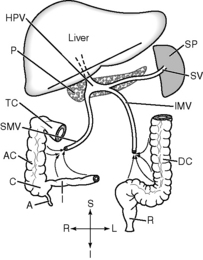
MRI of the abdomen—portal vein
Follow the scan protocol for abdomen and kidneys, adding a sequence for the portal vein.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree