CHAPTER 5 MRI of the Thorax
MRI of the breast
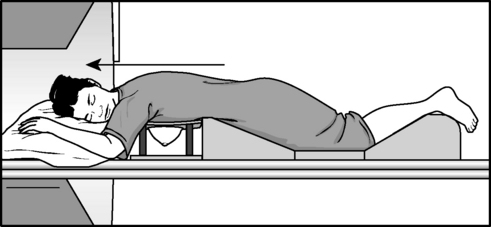
Patient Preparation and Positioning
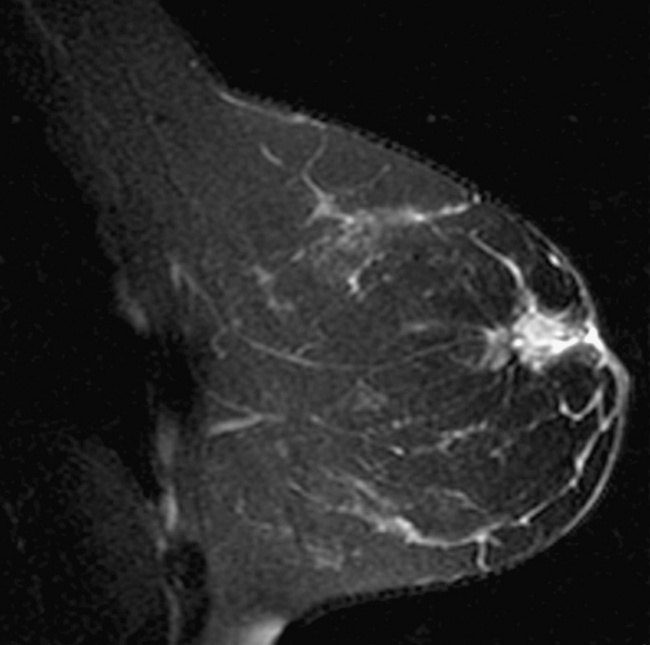
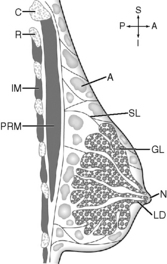
high-definition (HD) breast coil. High-definition breast array coils are available from all vendors and have biopsy capabilities. The breasts should be hanging freely in the coil and not touching the sides. Place gauze between the patient and the coil when necessary to avoid any possibility of bright signal from coil burnout. The patient should be made as comfortable as possible, making sure to support the feet as well as the head and arms. Communicating with the patient during the examination is imperative. The patient’s intravenous line should be hooked up to the power injector before the examination begins.
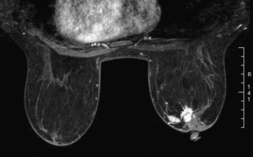
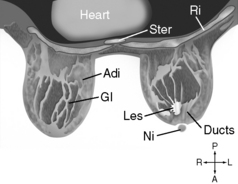
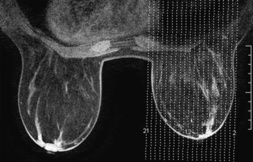
Bilateral Breast Imaging
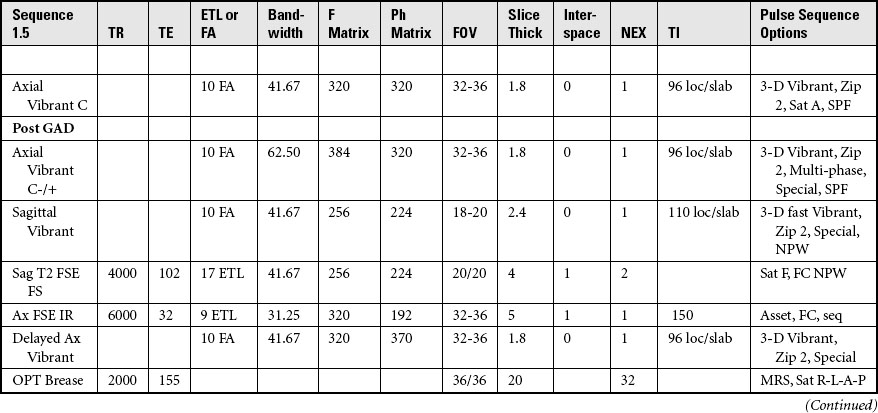
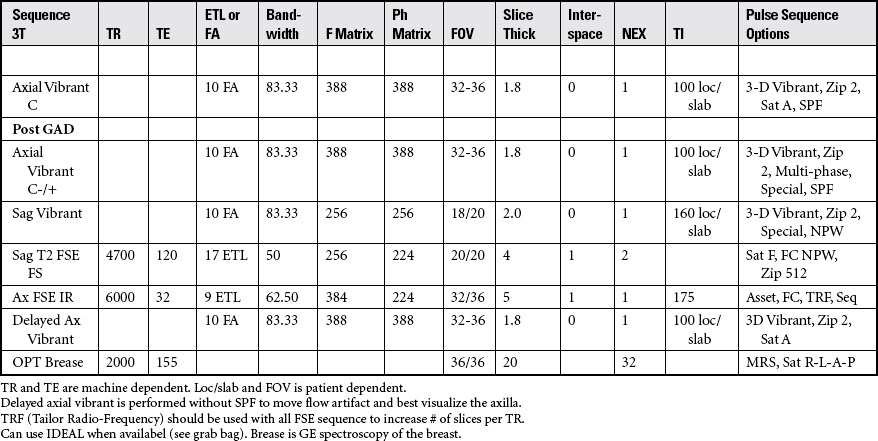
Acquire three-plane pilot per site specifications.
COIL: Multi-channel vendor-specific breast coil
POSITION: Prone, feet first with the breasts suspended in the coil
Place the cushion under the ankles, with the arms extended comfortably toward the head.
IMMOBILIZATION: Shield the patient from touching the sides of the magnet by using sponges or sheet.
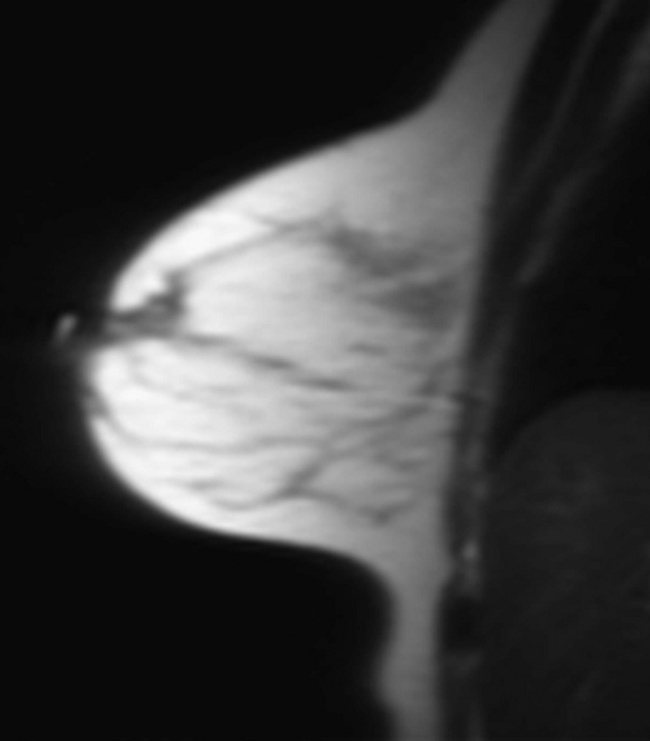
Acquisition of Axial images of the Breasts
SLICE ACQUISITION: Plot superior to inferior
SLICE ALIGNMENT: Perpendicular to the sternum
ANATOMIC COVERAGE: Chest wall through the nipple, including the axillary margins
Cardiac MRI
Cardiac Nomenclature
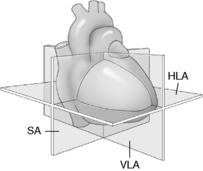
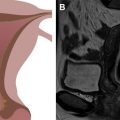
The nomenclature of short, vertical long, and horizontal long axis is suggested for cardiac planes used in cardiac MR. For the purpose of industry-wide consistency, this nomenclature will be adhered to in this text. See Figure 5-11 below.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree