Sarcoidosis, Fibrotic
Melissa L. Rosado-de-Christenson, MD, FACR
Key Facts
Terminology
Multisystem granulomatous disease
Unknown etiology
Young and middle-aged adults
Frequent involvement of lymph nodes, lung, eye, and skin
Imaging Findings
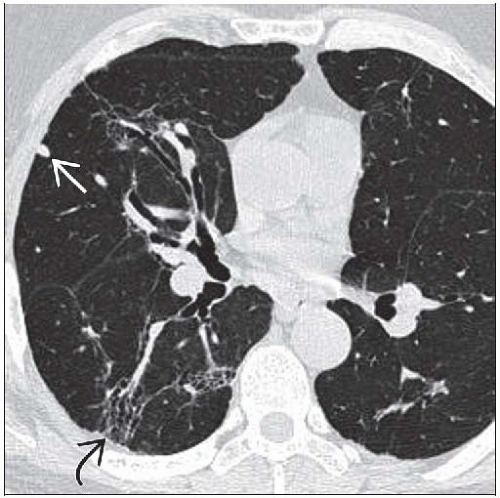
Best diagnostic clue: Predominant architectural distortion of central upper lobe with volume loss
Peribronchovascular nodules aggregate into masses extending from hilum to lung periphery
Often cuts swath through lung
Traction bronchiectasis prominent, may lead to cystic change within lung
Cystic areas may be secondarily involved with aspergillomas
Lymph nodes typically become smaller as parenchymal disease worsens
Lymph nodes may have “eggshell” calcification or smudgy central putty-like calcification
Top Differential Diagnoses
Silicosis
Post-Primary Tuberculosis
Hypersensitivity Pneumonitis
Pathology
Diagnosis of exclusion
May be difficult to diagnose in advanced stages as granulomas replaced by fibrous tissue
Clinical Issues
Poor prognosis
Respiratory failure from fibrosis, mycetomas, hemorrhage, cor pulmonale
TERMINOLOGY
Definitions
American Thoracic Society definition
Multisystem granulomatous disorder of unknown etiology; affects young and middle-aged adults
Frequent hilar lymphadenopathy, pulmonary involvement, eye and skin lesions
Typical clinical and imaging findings supported by histologic evidence of noncaseating epithelioid granulomas
Exclusion of other granulomatous diseases and local sarcoid reactions
Löfgren syndrome: Bilateral hilar lymphadenopathy, erythema nodosum, fever, arthralgias/arthritis
Heerfordt syndrome: Uveitis, parotitis, fever
Lupus pernio: Chronic subcutaneous induration and purplish discoloration of central face and hands
Produced by granulomatous infiltration; associated with sarcoidosis
IMAGING FINDINGS
General Features
Best diagnostic clue: Predominant fibrosis and architectural distortion of upper lobe
Patient position/location: Central upper lung fibrosis
Morphology
Architectural distortion
Cystic changes
Subpleural honeycomb lung
CT Findings
Lung
Smooth or nodular peribronchovascular thickening, follows lymphatic pathways in lung
Decreased number of small perilymphatic nodules as they aggregate into mass-like lesions
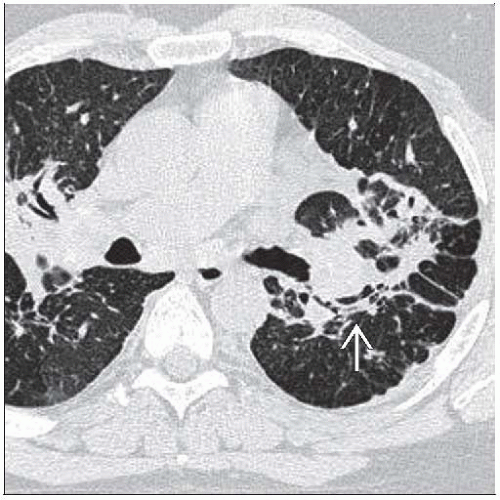
Cystic changes
May exhibit intracystic soft tissue related to saprophytic fungus (mycetoma)
True cavities uncommon
Peripheral subpleural honeycomb lung
Linear opacities
Airways
Traction bronchiectasis (central)
Bronchial wall thickening and airway stenosis
Distribution
Predominantly upper lung zone
Posterior displacement of main and upper bronchi
Secondary to volume loss in posterior segments of upper lobes
Hilar retraction from volume loss
Central perihilar conglomerate masses cut swath through lung
Lymphadenopathy
All nodal stations on CT
Bilateral hilar, right paratracheal, AP window, subcarinal
Rarely: Dominant anterior mediastinal, unilateral hilar, posterior mediastinal
Calcification may be present in varying degrees
“Eggshell”
Central smudgy or putty-like
As lung findings in sarcoid advance, adenopathy typically resolves or decreases in size
Complications
Pulmonary artery hypertension: Enlarged central pulmonary arteries, dilatation of right atrium and ventricle
Pleura
Pleural effusion/thickening or pneumothorax uncommon
Ipsilateral pleural thickening; typically precedes mycetoma formation
Radiographic Findings
Radiography
Findings not as specific as CT
Radiographic staging of sarcoidosis
Stage 0: Normal chest radiograph
Stage I: Lymphadenopathy, no pulmonary disease
Stage II: Lymphadenopathy and pulmonary disease
Stage III: Pulmonary disease, no lymphadenopathy
Stage IV: Pulmonary fibrosis
Imaging Recommendations
Best imaging tool: CT to characterize lung disease
DIFFERENTIAL DIAGNOSIS
Silicosis
Progressive massive fibrosis
Irregular conglomerate masses
Associated cavitation and traction bronchiectasis
Cicatricial emphysema
Small perilymphatic nodules
Lymphadenopathy; may exhibit calcification
Post-Primary Tuberculosis
Mycobacterium tuberculosis infection
Upper lobe predominant; apical and posterior segments
Frequent cavitation; associated bronchiolitis
Upper lobe architectural distortion, hilar retraction, traction bronchiectasis
Chronic Hypersensitivity Pneumonitis
Exposure history
Architectural distortion, septal thickening, honeycomb lung, traction bronchiectasis
Ground-glass opacities, centrilobular nodules
Talcosis
History of IV drug abuse
Background nodules usually pinpoint in size
Progressive massive fibrosis (PMF) may be of high density
PATHOLOGY
General Features
General path comments
Sarcoidosis is diagnosis of exclusion
Granulomas are nonspecific finding
Etiology: Unknown
Epidemiology
Higher prevalence in African-Americans and northern Europeans
Higher prevalence rates in 1st degree relatives
Sarcoidosis is more common in nonsmokers
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree