10 Diaphragm
Introduction
The diaphragm is a musculotendinous dome-shaped sheet between the thoracic and abdominal cavities. More than just a geographical boundary between the thoracic and abdominal cavities, the diaphragm is the most important muscle of respiration and vital to human life. Understanding its embryology, anatomy, and mechanism of action is key to interpretation of its pathologies.
Embryology
Four embryological structures give rise to the mature diaphragm during weeks 4 to 12 of human development: the transverse septum anteriorly, two pleuroperitoneal folds (membranes) laterally, the dorsal mesentery (aka the esophageal mesentery) dorsomedially, and muscular ingrowth from the lateral body walls (Fig. 10‑1). These primitive structures together form the mature diaphragm’s two parts: a fibrous central tendon and peripherally arising muscular bundles, which will be described in detail later.
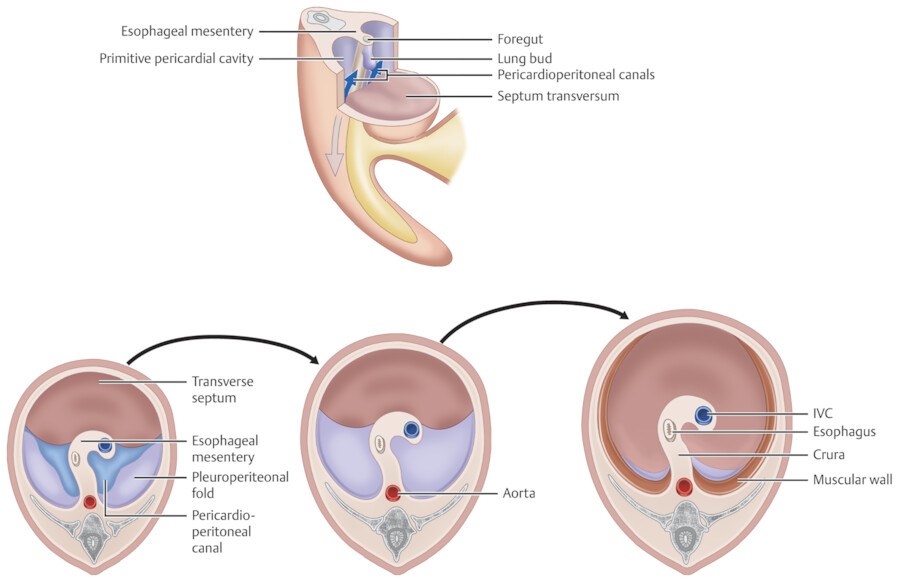
The transverse septum is the first diaphragmatic precursor to develop, arising from the mesenchymal coelomic wall at the level of the C3 cervical somites during weeks 3 to 4 of gestation. As the head folds ventrally during the fourth week of gestation, the transverse septum forms a partition between the pericardial and abdominal cavities anteriorly, separating the heart from the liver. During weeks 4 to 8 this mesoderm descends from the cervical level to its final position at the junction of the thoracic and abdominal cavities. 1 , 2 , 3 , 4 During this descent through the neck, myogenous stem cells are able to migrate from cervical somites into the transverse septum. The transverse septum forms major parts of the diaphragm; therefore, innervation of the diaphragm is mainly supplied from the phrenic nerve, derived from C3, C4, and C5. 3 The pleuroperitoneal membranes are the next diaphragmatic precursors to develop. Arising during week 6 of development from the lateral body wall, they grow medially to flank the esophagus, meet the transverse septum and the dorsal mesentery. The dorsal/esophageal mesentery anchors the foregut to the body wall and eventually forms the diaphragmatic crura. After the pleuroperitoneal membranes have fused to the transverse septum and dorsal mesentery, muscle bundles derived from myotomes of the 7th to 12th segments begin to develop between the primitive pleura and peritoneum, forming the muscular portion of the diaphragm and give the final dome-shaped appearance of the diaphragm. These muscle bundles are categorized into three groups based on their origins from the peripheral body wall: the pars lumbalis, costalis, and sternalis. Therefore, innervation of the peripheral part of the diaphragm is by the lower intercostal nerves. The diaphragm in newborn is relatively flat and moves mainly in its posterior part whereas in the adult it is dome-shaped and move centrally.
Anatomy
The diaphragm is domed-shaped peripherally and is relatively flat in its central portion (Fig. 10‑2). It is approximately 2 to 4 mm in thickness. The right hemidiaphragm is located higher on the right than the left. The overall configuration and position of the diaphragm is influenced by the status of respiration, patient position, and pathologies. In supine position, the diaphragm remains high than standing position. 4 , 5 , 6 Hyperinflated lungs or large pleural effusion can depress the diaphragm. The slope of the diaphragm from the dome to the periphery is greatest in the posterior region forming the posterior costophrenic angle where pleural fluid accumulates first (Fig. 10‑2 , Fig. 10‑3).
The superior surface of the diaphragm is covered by the endothoracic fascia, parietal diaphragmatic pleura, and pericardium. The diaphragmatic pleura and the fibrous pericardium are firmly attached to the endothoracic fascia and diaphragm.
The anteroinferior surface of the diaphragm is covered by the diaphragmatic fascia, an extension of the transversalis fascia, extraperitoneal fat, and in part by the peritoneum (Fig. 10‑4). The posteroinferior surface of the diaphragm is not covered completely by the peritoneum and faces the retroperitoneal fat. The diaphragmatic attachment of the falciform ligament and bare area of the liver also are not covered by the peritoneum (Fig. 10‑4). The falciform ligament is the remnant of the primitive ventral mesentery, extending between the anterior abdominal wall and the diaphragm and the anterior surface of the liver. 4
The round ligament of the liver and the obliterated left umbilical vein run in the free edge of the falciform ligament facing the peritoneum.
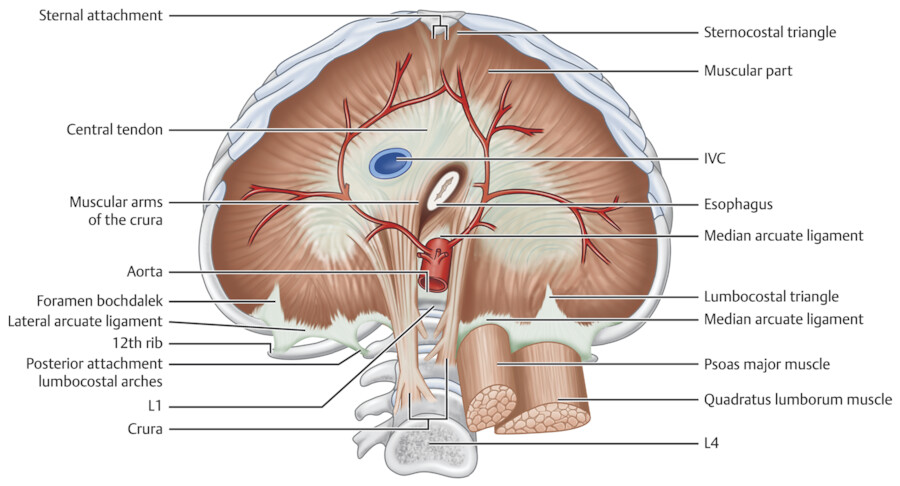
The diaphragm is comprised of two parts: a central tendinous and a peripheral muscular (Fig. 10‑5). The diaphragm muscle is composed of two regions. The costal diaphragm which is a thin striated muscle in the periphery of the diaphragm and the crural diaphragm which is thicker and located more posteriorly in the paravertebral area.


Central Tendon
The central tendon of the diaphragm is an aponeurosis to which the diaphragmatic muscles project from the body wall. This central tendon is positioned anteriorly along the diaphragmatic dome and subjacent to the fibrous pericardium. The tendon is most commonly V-shaped. Three leaflets comprise the central tendon: right, middle, and left, listed here in order of decreasing size. 7 Superior surface of the central tendon is adhered to the fibrous pericardium (Fig. 10‑3).
Peripheral muscular attachments of the central tendon are divided into (1) sternal or anterior, (2) costal or lateral, and (3) lumbar or posterior. The tendon area is smaller than the muscle area in most individuals. 7 Diaphragmatic attachments on the sides are symmetric. The crural attachment of the diaphragm is asymmetric when comparing the left and right sides.
Muscular Attachments
Anterior/Sternal and Lateral Attachments
Anteriorly, the diaphragm attaches to the xiphoid process, aponeurosis of the transverse abdominal muscle (Fig. 10‑4 , Fig. 10‑5). The anterolateral diaphragm attaches to the medial aspects of the 7th and 8th ribs and their anterior costochondral junctions anteriorly and the 9th and 10th ribs laterally. The xiphoid slip attachment, or the sternal part of the diaphragm, being the most central and superior anterior attachment, results in an inverted V- or U-shaped configuration to the diaphragm when viewed in the frontal (coronal) projection 8 (Fig. 10‑6 , Fig. 10‑7). Small triangular spaces known as “foramina of Morgagni” separate the sternal attachment slips from the costal fibers on each side (Fig. 10‑5).


Posterior/Lumbar Attachments
Posteriorly and medially, the diaphragm attaches to the body wall via the left and right crura, which are anchored to the superior aspect of the lumbar spine. Posterolaterally, the diaphragm attaches to the 11th and 12th ribs. This part of diaphragm blends with aponeurosis of the transverse abdominal muscle and the deep layer of the thoracodorsal fascia.
Variable Appearance of the Diaphragmatic Muscular Slips
As described earlier, muscle bundles forming the muscular part of the diaphragm are categorized by their origin: lumbar, costal, and sternal or the pars lumbalis, costalis, and sternalis. 8 , 9 These muscle bundles course from their peripheral origins, centrally and superiorly, toward the diaphragm’s central tendon. Diaphragmatic muscle bundles vary in morphology (Fig. 10‑6 , Fig. 10‑7). Thickened slips may pose a diagnostic challenge on imaging. Prominent slips may indent or invaginate the hepatic surface. Multiple slips invaginating the liver surface can mimic cirrhosis, though hepatic surface nodularity in cirrhosis is more irregular (Fig. 10‑7). In some cases, a particularly prominent slip may mimic a hepatic mass on some projections, particularly on ultrasound. Slips have also been shown to mimic abdominal adenopathy. In patients with abundant fat in the mediastinum and anterior abdominal wall, the sternal slips of the diaphragm may be displaced laterally. These laterally displaced slips with adjacent fat should not be mistaken with Morgagni hernia (Fig. 10‑6). On computed tomography (CT), identifying contiguity with the diaphragm on multiple transaxial CT images can help distinguish a slip from abdominal pathology. 8
Diaphragm Ligaments
Several ligaments composed of loose connective tissue are attached to the superior or inferior surface of the diaphragm. Above, the phrenopericardial ligament connects the diaphragm to the fibrous pericardium (see Chapter 5). The phrenicoesophageal ligaments join the esophagus and the left and right hemidiaphragms. 10 The inferior pulmonary ligament is a pleural thickening connecting the diaphragm to the hila of the lungs (see Chapter 5). In patients with hyperinflated lung volumes, the lower lobe engulfs the ligament on both sides, causing the ligament to appear to be located within the paravertebral lung on axial CT sections (Fig. 10‑8). The right ligament is located near the inferior vena cava (IVC) and the left ligament near the descending aorta. 8

Inferior to the diaphragm the two layers of the falciform ligament are continuous with the peritoneal reflections between the liver and diaphragm. 4 These peritoneal reflections form the anterior and posterior layers of the coronary ligament on the right and left. The anterior and posterior coronary ligaments meet to enclose the bare area on each side. Their confluence points form the right and left triangular ligaments. The bare area of the liver faces the IVC, right adrenal, superior pole of the right kidney, right crus, and vertebrae (Fig. 10‑4 , Fig. 10‑9). There is also a small bare area behind the abdominal esophagus facing the diaphragm and at the attachment of gastrophrenic ligament. The phrenicocolic ligament connects the splenic flexure of the colon to the diaphragm at the level of the 11th rib (Fig. 10‑4). The ligament of Treitz connects the duodenojejunal junction to the right crus.

Arcuate ligaments are thickened fascia along the posterior margin of the diaphragm. Posteriorly and laterally, the diaphragm forms two arcuate ligaments on each side. 11 The lateral arcuate ligament spans the quadratus lumborum, whereas the medial arcuate ligament spans the psoas muscles (Fig. 10‑5). The lateral arcuate ligament extends between the transverse process of L1 and the inferior edge of the 12th rib. The medial arcuate ligament extends between the transverse process of L1 and the corresponding crus. The medial arcuate ligaments are separated from each other by the crura and the vertebral bodies.
The median arcuate ligament joints the crura in midline. It usually passes superior to the origin of the celiac axis. Low-lying variations of the median arcuate ligament’s attachments to the lumbar spine can compress the celiac artery in 10 to 24% of people, in some cases resulting in symptoms including abdominal pain, nausea and vomiting, or median arcuate ligament syndrome 12 (Fig. 10‑10).

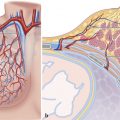
Diaphragmatic Crus
The term crura, the plural of crus, is derived from the Latin word cruralis, meaning “leg.” There are two diaphragmatic crura on the sides of the vertebral bodies that encircle the gastroesophageal (GE) junction and forms the hiatus of the diaphragm. 13 , 14 The crura arise from the anterior surface of the lumbar vertebral bodies and the anterior longitudinal ligament from L1 through L3 and insert on the central tendon. It is longer on the right side. The origin of the crura near the bone is tendinous but the crura become increasingly muscular as they ascend into the diaphragm. Only the tendinous parts hold sutures after surgery. Each crus has two parts, a vertical part that moves along the vertebrae and a transverse part along the diaphragm proper. The pattern of the transverse part of the crus at esophageal hiatus is variable. In many cases, especially on the right side, two arms exist, one anterior and one posterior to the GE junction, that encircle the esophageal hiatus. In a recent study by Loukas et al, it is shown that in 45% the esophageal hiatus is formed from muscular contributions of the right crus only (Fig. 10‑5). 14 This pattern is very common in CT studies of the abdomen. In 20 to 30% the left arm arises from the right crus, and the right arm arises from both crura or the right side. Extra bands may be seen in the remainder of cases (Fig. 10‑11). There is a wide range of normal variants of the diaphragmatic crura.

The phrenicoesophageal ligaments (membrane) attach the lower esophageal segment to the diaphragmatic crura within the esophageal hiatus and indirectly prevent GE reflux. Its fibers are continuous with the transversalis and endothoracic fascia covering the diaphragm and penetrate superiorly and inferiorly in the adventitia and intermuscular connective tissue of the distal esophagus. 15 In adults, the ligament is attenuated as subperitoneal fat accumulates in the hiatus and in hiatal hernia the ligament is either torn or disappeared.
Retrocrural Space
The retrocrural space is a small triangular region posterior to the two diaphragmatic crura and anterior to the spine. 16 Normal structures within the retrocrural region include the aorta, nerves, the azygos and hemiazygos veins, the cisterna chyli with the thoracic duct, fat, and lymph nodes (Fig. 10‑12). It is a common location for passage of abnormalities from the abdomen into the posterior mediastinum including lymph node metastasis, hernia of fat, and primary tumors. Aortic aneurysm and azygos and hemiazygos continuation of the IVC are among vascular abnormalities in this region. Enlarged azygos and hemiazygos veins in this region are a common finding in cirrhosis with portal hypertension and those with thrombosis of the IVC (Fig. 10‑12).

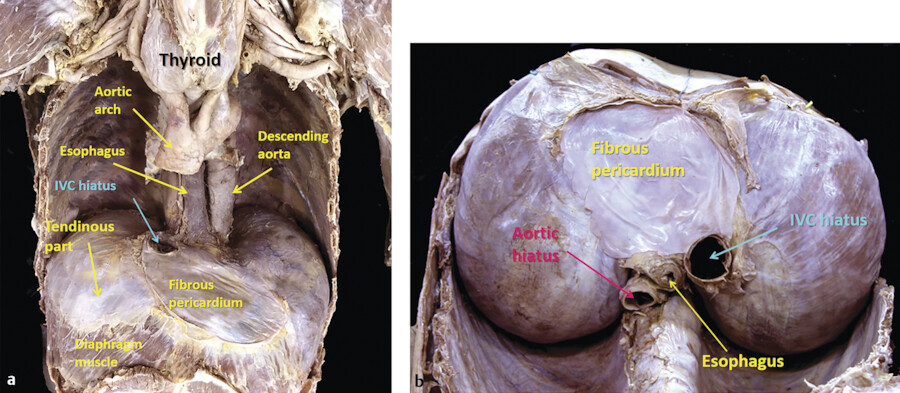
Diaphragmatic Hiatuses
While serving as a boundary between the thoracic and abdominal cavities, the diaphragm must allow, structures important to both cavities, to pass from one side to the other 17 (Fig. 10‑3 , Fig. 10‑5). The diaphragm thus provides three major openings, or hiatuses, named after the principal structures traveling through them, namely the aortic, esophageal, and vena caval hiatuses. Smaller hiatuses exist and will be described below. Communication occurs between structures above and below the diaphragm through the hiatuses. The aortic and esophageal hiatuses are the most common diaphragmatic communication pathways through which inflammatory, infectious, and malignant processes can spread from one cavity to another. Through small porous defects or perivascular sheaths air or fluid can travel between the thorax (mediastinum or pleura) and the abdomen (abdominal wall, peritoneum, or retroperitoneum).
Vena Cava Hiatus
The most cephalad hiatus is the vena caval hiatus, located at the T8 level approximately 2 cm to the right of the midline. In addition to the IVC, this diaphragmatic opening also provides a passage for branches of the right phrenic nerve and pericardiophrenic vessels. It is not uncommon to see the retroperitoneal fat entering this region causing narrowing of the IVC (Fig. 10‑13).

Esophageal Hiatus
At the T10 level, the esophagus with its vessels, vagal nerve, and additional sympathetic nerve fibers pass through the diaphragm at the esophageal hiatus. The anterolateral margins of the hiatus are formed by the crura and the posterior margin is formed by the median arcuate ligament. Given the common occurrence and poorly understood etiology of hiatal hernias, many authors have studied the anatomical variants of the esophageal hiatus. As described earlier, in the most common configuration, the esophageal hiatus is encircled by the dorsal and ventral arm of the right diaphragmatic crus, alone. 18 Of note, in a surgical electrophysiological stimulation study of 14 patients, Shafik et al suggested that the muscular loop encircling the distal esophagus was not crural in origin at all, but an entirely separate muscle, which he named the “striated GE sphincter.” 19 The normal size of the esophageal hiatus is variable. Mean hiatal surface area is reportedly 5.84 cm2. 20 It may become larger in patients with a large amount of visceral fat and increases with age as the space fills with loose connective tissue and fat (see Volume II, Chapter 2, Esophagus). 21
Aortic Hiatus
The aorta finds its way through the diaphragm at the T12 level along with the thoracic duct and azygos and hemiazygos veins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree