11
Breast Imaging
Laurie L. Fajardo • Limin Yang
 Chapter Outline
Chapter Outline
Technique for Screening and Diagnostic Mammography
What We Should See on a Mammogram
Indications for Breast Ultrasound and Magnetic Resonance
Suggested Workup of Common Clinical Problems
Approximately one in eight women in the United States will develop cancer of the breast during her lifetime, and this incidence appears to be increasing. Unfortunately, there is no known cause of most breast cancers, and therefore the best way to prevent mortality is early detection of the nonpalpable and potentially curable disease using mammography. It is generally believed that the earlier breast cancer is diagnosed, the smaller the chance of metastases and the better the long-term prognosis. Consequently, mammography is widely used for the screening of breast cancer in the general asymptomatic female population. Screening mammography should be used in conjunction with regular breast self-examination and an annual clinical breast examination performed by a physician (Table 11.1). Diagnostic mammography is also a key tool in the evaluation of patients with known or suspected breast disease. There is little doubt that mammograms are best interpreted by qualified radiologists. In addition, a radiologist may perform image-guided breast biopsy allowing an accurate and cost-effective diagnosis of nonpalpable breast lesions. Given the prevalence of breast disease, all physicians should be aware of the clinical applications and limitations of breast imaging. The purpose of this chapter is to review the importance of screening mammography for early cancer detection and the use of diagnostic mammography, ultrasound (US), and magnetic resonance imaging (MRI) in the management of breast disease.
SCREENING MAMMOGRAPHY
The mortality rate for breast carcinoma has fallen by almost 30% over the past 20 years. Several large reputable studies have linked this reduction in mortality with earlier detection of breast carcinoma due to screening mammography. Critics of routine screening argue that women may go through unnecessary treatment such as surgery, radiotherapy, and chemotherapy for cancers that would not have posed a risk as some cancers will be diagnosed and treated that would never have caused any harm. In the United Kingdom, it is estimated that screening prevents about 1,300 deaths per year, but it also may result in about 4,000 women receiving treatment for a condition that would not have been threatening.
In 2009 the U.S. Preventive Services Task Force (USPSTF) revised their recommendations for screening mammography for women aged 40 to 49 years, because there was only moderate certainty that the net benefits for this age group were small. Previously routine screening mammography was recommended every 1 to 2 years starting at age 40. Their current recommendations are for biennial rather than annual screening in women aged 50 to 74 years. No recommendation was made for women over age 74, citing insufficient evidence. The Society of Breast Imaging (SBI) and The American College of Radiology (ACR) strongly criticized the USPSTF recommendations, and they have jointly published their own recommendations for screening mammography (Table 11.2). These recommendations are on the basis of evidence-based medicine where available. Where evidence is lacking, the recommendations are based on consensus opinions. The ACR and SBI firmly stand behind their recommendation that screening mammography should be performed annually beginning at age 40 for women at average risk for breast cancer.
Table 11.1

As can be seen from these recommendations, several risk factors influence the onset and type of screening. One of these risk factors is a BRCA gene mutation which is associated with a rare hereditary breast–ovarian carcinoma syndrome. As many as two-thirds of women born with a deleterious mutation in BRCA1 will develop breast cancer by age 70, and one-third will develop ovarian cancer by age 70. Approximately one-half of women with a deleterious mutation in BRCA2 will develop breast cancer by age 70, and up to one-quarter will develop ovarian cancer by age 70. The ACR/SBI recommendations include annual screening mammograms and also cover the role of MR of women with BRCA mutations.
Technique for Screening and Diagnostic Mammography
The importance of a well-performed mammogram cannot be overemphasized. A standard screening mammogram consists of two views: A mediolateral oblique (MLO) view with the central x-ray beam traversing the breast obliquely in a medial to lateral direction (Fig. 11.1A) and a craniocaudal (CC) view (Fig. 11.1B) with the central x-ray beam traversing the breast in a head to foot direction. It is necessary to compress the breast during the examination to visualize all the breast tissue and to minimize radiation dose, and patients should be warned that compression may be uncomfortable. As with other forms of imaging, mammography has limitations and adjunct screening using US and MRI is becoming more widely accepted. A diagnostic workup may require specific mammographic views including microfocus magnification compression views for microcalcifications and focal (spot) compression views for mass or focal asymmetry and possibly the need for US and/or MRI. For women under 30 years who present with a breast mass, US is the best initial examination to perform.
Table 11.2
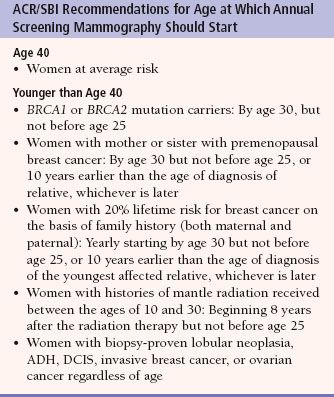
From: Lee CH, Dershaw DD, Kopans D, et al. Breast cancer screening with imaging: Recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol. 2010;7(1):18–27; copyright © 2010 Elsevier.
Diagnostic mammography is performed most commonly when a breast mass is palpated, or a radiologist finds an abnormality on a screening mammogram. The vast majority of screening and diagnostic mammograms performed in the United States use digital technology which has replaced film-screen mammography. The advantages of digital mammography include the ability to use image-processing techniques to enhance the images, the use of computer-assisted diagnostic techniques (CAD) in lesion detection and characterization, and the electronic transmission and storage of images. Compared with film-screen mammography, digital mammography has been shown to be superior in detecting breast cancer in women younger than 50 years, pre- or perimenopausal women, and those with dense breasts.
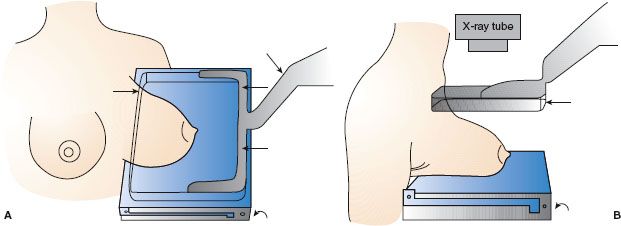
FIGURE 11.1. Mammographic technique. A: Illustration of patient positioning for a mediolateral oblique (MLO) mammogram. The x-ray beam passes obliquely through the breast in a medial to lateral direction. The breast is routinely compressed between the compression device (straight arrows) and the radiographic cassette (curved arrow). The cassette contains a radiographic film on which the image will be recorded. Compression improves the diagnostic quality of the images by reducing the breast to a more uniform thickness. B: Illustration of patient positioning for a craniocaudal (CC) mammogram. The x-ray beam passes through the breast in a head to foot or cephalad to caudad direction. The compression device (straight arrow) is more easily visualized in this illustration. Again, the image will be recorded on the film in the radiographic cassette (curved arrow).
It is important that the mammographer (technologist) be properly trained and qualified and that the federally mandated mammography quality controls are met.
WHAT WE SHOULD SEE ON A MAMMOGRAM
In general, breast tissue is composed predominately of fibroglandular tissue in younger women and gradually replaced with adipose tissue in older women. Correspondingly, normal mammograms show a mixture of fat and fibroglandular tissue. Normal MLO and CC views of the breast are shown in Figure 11.2. Notice that breast images are a combination of fat (black) and soft tissues (gray to white). This background of black and gray, especially the black, enhances visualization of masses and calcifications.
Approximately 85% of breast carcinomas are of ductal origin and are discrete by imaging modalities.
The two most important mammographic findings suspicious for malignancy are masses and microcalcifications. Other suspicious abnormalities include focal asymmetry, architectural distortion, and skin or nipple deformity. Any structural changes over time require attention and further workup, unless otherwise explained such as surgical scar.
The Breast Imaging Reporting and Data System (BI-RADS) initiative was instituted by the ACR in the late 1980s to address a lack of standardization and uniformity in mammography practice reporting. An important component of this system is the lexicon, a dictionary of descriptors of specific imaging features which historically have been shown to be predictive of benign and malignant disease. Use of the BI-RADS lexicon promotes communication, quality assurance, research, and improved patient care. Initially, BI-RADS was developed for mammographic findings, but it now includes US and MRI findings (Table 11.3). This system is continuously revised on the basis of experts’ opinions and evidence-based findings.
Masses
Using BI-RADS terminology, a mass is a space-occupying lesion seen on two different mammographic projections. Masses are described in terms of their shape, border (margin), density, location, size, and associated findings such as microcalcifications and architectural distortion.
Table 11.3
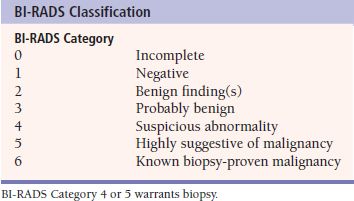
FIGURE 11.2. Normal mammogram. A: Left breast mediolateral oblique (MLO) digital mammogram. Normal. B: Left breast craniocaudal (CC) digital mammogram. Normal.
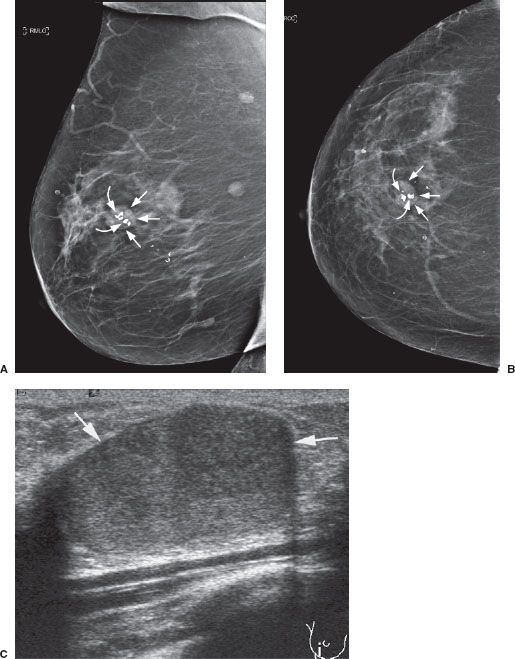
FIGURE 11.3. Fibroadenoma. Right breast MLO (A) and CC (B) mammograms. Calcified benign fibroadenoma. The fibroadenoma is oval and isodense with circumscribed borders (straight arrows). The benign calcifications within the fibroadenoma are typically globular, coarse, and variable in size (curved arrows). C: Ultrasound of the right breast shows a well-circumscribed homogeneous isoechoic solid mass which is corresponding to a palpable mass (arrows).
Benign Masses
Benign breast disease (Table 11.4) may or may not be symptomatic or have associated masses. A fibroadenoma (Fig. 11.3) is a common benign mass that generally occurs in young women and may be single or multiple. On physical examination, fibroadenomas are often movable. The mammographic appearance is an oval circumscribed mass sometimes associated with coarse “popcorn” calcifications. On sonography, fibroadenomas will usually appear isoechoic.
Table 11.4
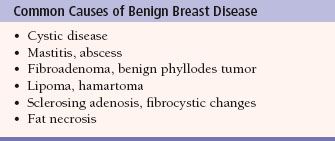
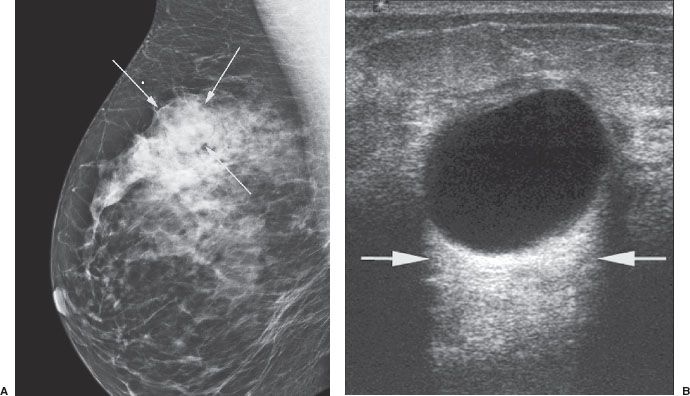
FIGURE 11.4. Simple cyst. A: Right breast MLO digital mammogram. A simple cyst. The isodense cyst (arrows) has sharp borders and no calcifications. Note the difference between the smooth sharp borders of this benign cyst compared to the irregular and poorly defined borders of the carcinoma in Figure 11.7. B: Right breast ultrasound of the lesion (A). This is the classic appearance of a benign simple cyst. The cyst is a round well-circumscribed anechoic mass with very thin cyst–parenchymal transition. Posterior acoustic enhancement (arrows) is commonly found immediately posterior to a cyst.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree