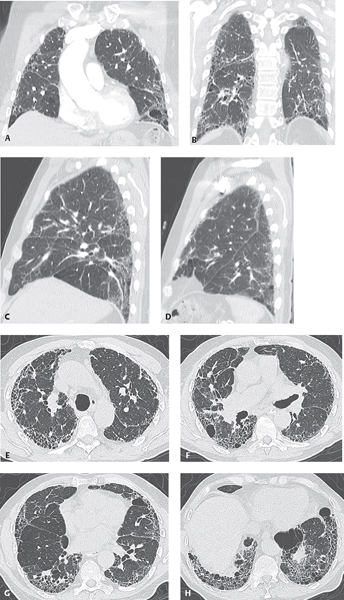
CASE 116 70-year-old man, non-smoker, with non-productive cough, increasing dyspnea, and fatigue Chest CT coronal anterior (Fig. 116.1A) and posterior (Fig. 116.1B) with accompanying right (Fig. 116.1C) and left (Fig. 116.1D) parasagittal MIP images demonstrate mild reduction in lung volume and a diffuse, chronic, interstitial fibrotic process that more extensively involves the posterior lung and lower lobes. HRCT axial CT images through the upper (Fig. 116.1E), mid (Figs. 116.1F, 116.1G), and lower lobes (Figs. 116.1G, 116.1H) reveal irregular septal and non-septal reticular opacities, architectural distortion characterized by traction bronchiectasis and bronchiolectasis, and honeycombing. Although all lobes are involved to some degree, the findings predominantly affect the paraseptal and juxtapleural regions of the lower lobes. Usual Interstitial Pneumonia (UIP); (Idiopathic Pulmonary Fibrosis) (IPF) aka Cryptogenic Fibrosing Alveolitis • Mixed Connective Tissue and Collagen Vascular Disorders with IPF • Recurrent Bouts of Aspiration • Chronic Pulmonary Drug Toxicity • Asbestosis • Chronic Hypersensitivity Pneumonitis • Fibrosing NSIP Usual interstitial pneumonia (UIP) is the most common of the idiopathic interstitial pneumonias (IIPs). It is a histologic pattern of chronic fibrosing interstitial pneumonia that may be idiopathic (idiopathic interstitial pneumonia, IPF) or may be a manifestation of various connective tissue disorders (e.g., rheumatoid arthritis, scleroderma), cytotoxic (e.g., bleomycin, busulfan, cyclophosphamide, methotrexate) and non-cytotoxic (e.g., amiodarone, gold salts, nitrofurantoin, oxygen) pulmonary drugs, or asbestosis. HRCT is accurate in the diagnosis of UIP. In one study, 47% of observers rendered a high-confidence diagnosis of UIP based on clinical findings alone, 79% with the addition of radiographic data, and 88% with the addition of HRCT. While HRCT is more sensitive than chest radiography, a normal HRCT does not exclude UIP, although this occurs in less than 10% of cases. Transbronchial biopsy cannot be used to establish the diagnosis but is useful in excluding alternative diagnoses (e.g., infection, malignancy, COP, eosinophilic pneumonia, sarcoidosis). The cause of UIP-IPF remains unknown. A role for genetic factors is supported by the findings of familial cases (e.g., Hermansky-Pudlak syndrome). Cigarette smoking results in a 1.6–2.3-fold increased risk of developing pulmonary fibrosis. Long-term exposure to metal or wood dusts is also an independent risk factor.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Radiology Key
Fastest Radiology Insight Engine