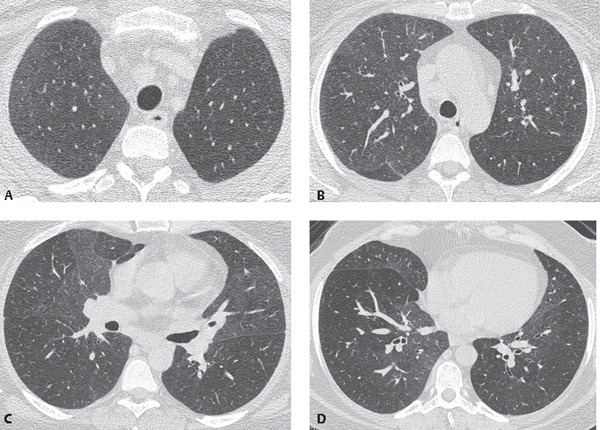
CASE 117 41-year-old man with long-standing history of tobacco abuse since age 11, complaining of worsening cough and progressive dyspnea over the past 18 months HRCT (Figs. 117.1A, 117.1B, 117.1C, 117.1D) demonstrates profuse poorly defined subtle centrilobular nodules primarily in the upper lung zones (Figs. 117.1A, 117.1B) and a background of diffuse, patchy ground glass throughout both lungs with a mid and upper lung zone predominance (Figs. 117.1A, 117.1B, 117.1C, 117.1D). Mild bronchial wall thickening is present. Expiratory images (not provided) demonstrated multifocal lobular areas of air trapping. Subsequent open lung biopsy confirmed the diagnosis. Respiratory Bronchiolitis–Interstitial Lung Disease (RB-ILD) Fig. 117.1 • Desquamative Interstitial Pneumonitis (DIP) • Acute-Subacute Hypersensitivity Pneumonitis (HP) • Pulmonary Langerhans’ Cell Histiocytosis (PLCH) Respiratory bronchiolitis (RB) (smoker’s bronchiolitis) is a common but incidental histologic finding in asymptomatic cigarette smokers. Symptomatic smokers presenting with symptoms mimicking interstitial lung disease are diagnosed with respiratory bronchiolitis–interstitial lung disease (RB-ILD). RB, RB-ILD, and desquamative interstitial pneumonia (DIP) (see Case 108) are part of the spectrum of smoking-related interstitial lung diseases. Any given patient with a significant history of tobacco abuse may exhibit overlapping clinical and histopathologic features of all three diseases as well as centrilobular emphysema (see Case 28). The incidence and prevalence of RB and RB-ILD are unknown, and there is no sexual predilection. The cause and pathogenesis are unknown, but RB and RB-ILD are strongly related to tobacco abuse.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Clinical Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree