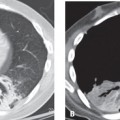
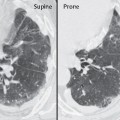
CASE 119 58-year-old woman with untreated adenocarcinoma of the left lung diagnosed three months earlier and who refused treatment returns with complaints of increasing dyspnea. PA (Fig. 119.1A) and lateral (Fig. 119.1B) chest X-rays reveal abnormal irregularly thickened septal linear opacities throughout both lungs. Although the cardiomediastinal silhouette is enlarged, there is no evidence of heart failure. The vascular pedicle is not widened and vascular clarity is maintained. Note the left upper lobe mass and the right hilar lymphadenopathy. HRCT images through the upper, mid, and lower lung zones (Figs. 119.1C, 119.1D, 119.1E, 119.1F) acquired three weeks later following the onset of respiratory failure demonstrate profuse smooth and nodular thickening of the interlobular septa of multiple SPLs in both lungs. Asymmetric thickening of the bronchovascular bundles are seen in the right lung (Figs. 119.1E, 119.1F). The right pleural effusion proved to be malignant. Note the left upper lobe mass (Fig. 119.1D). Lymphangitic Carcinomatosis; Primary Lung Adenocarcinoma • Pulmonary Edema • Sarcoidosis • Coal Worker’s Pneumoconiosis (CWP) • Lymphocytic Interstitial Pneumonia (LIP) • Idiopathic Pulmonary Fibrosis (IPF) • Pulmonary Lymphoma Pulmonary lymphangitic carcinomatosis (PLC) refers to the proliferation and spread of tumor in the pulmonary lymphatics. Virtually any metastatic neoplasm can demonstrate lymphangitic spread. The most common primary neoplasms associated with PLC are adenocarcinomas that originate in the lung, breast, stomach, pancreas, and prostate. PLC also occurs in patients with carcinomas of the thyroid and cervix, and with metastatic adenocarcinoma from an unknown primary site. PLC typically results from hematogenous spread of neoplasm to the lung with subsequent interstitial and lymphatic invasion. Direct lymphatic spread of tumor from mediastinal and hilar nodes may also occur.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree