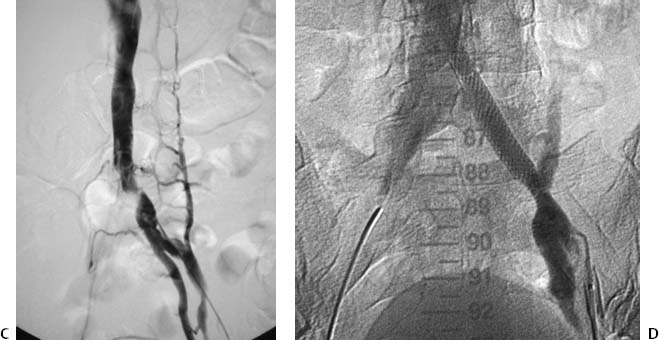
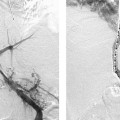
CASE 14 A 19-year-old male presented to the outpatient clinic with intermittent left lower extremity swelling. Figure 14-1 Diagnosis and treatment of May-Thurner syndrome. (A) Infused CT shows compression of the left common iliac vein by the right common iliac artery. The right common iliac vein appears enlarged. (B) Left pelvic venogram shows nearly complete obstruction of the left common iliac vein with venous drainage of the left leg occurring through pelvic and paraspinal collaterals. (C) Repeat venogram after initial angioplasty with side holes of pigtail catheter crossing the level of obstruction. The vertical linear defect of the left common iliac vein is consistent with May-Thurner syndrome. (D) After placement of a 10- × 40-mm Wallstent across the left common iliac vein, there is free flow across the common iliac vein with resolution of collateral flow. An infused CT scan showed compression of the left common iliac vein by the right common iliac artery without evidence of adjacent masses, inflammation, or fibrosis (Fig. 14-1A). The right common femoral vein was punctured, the left femoral vein was selected using a visceral catheter (RIM, Cook, Bloomington, Indiana), and left femoral venograms were performed (Fig. 14-1B, C) showing obstruction of the left common iliac vein with minimal contrast material passing into the inferior vena cava. Multiple pelvic and paraspinal collateral veins were markedly enlarged and provided venous drainage from the left leg. Obstruction of the left common iliac vein resulting from May-Thurner syndrome. The left common iliac vein occlusion was traversed from an ipsilateral common femoral vein approach. After pre-dilating the lesion with an 8mm angioplasty balloon catheter (Fig. 14-16), a Wallstent (Boston Scientific, Natick, Massachusetts; length, 10 x 40 mm) was deployed (Fig. 14-1D) to preserve potential venous collateral pathways, and the width was chosen to overestimate the diameter of the iliac vein by at least 10%. The patient’s leg swelling resolved, and he returned to his sports activities after 2 weeks. He has been symptom-free for 1 year.
Clinical Presentation
Radiologic Studies
CT
Venography
Differential Diagnosis
Diagnosis
Treatment
Endovascular Stent Placement
Equipment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree