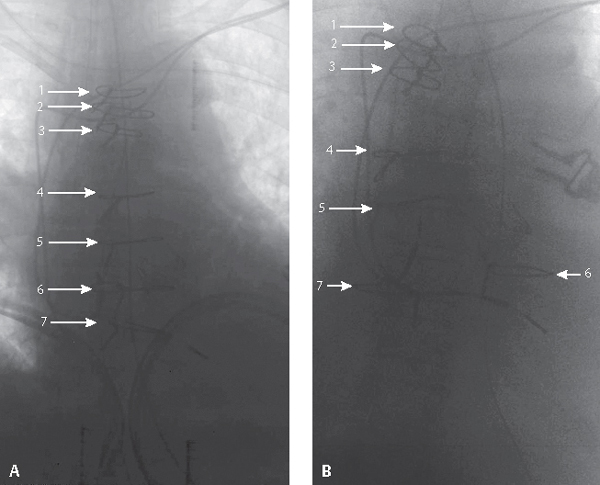
CASE 150 76-year-old woman status 11 days post median sternotomy and coronary artery revascularization, complaining of pain and the sensation of movement in her anterior chest wall, especially with coughing Initial postoperative coned-down inverted chest radiograph (Fig. 150.1A) shows normal midline alignment of the sternal cerclage wires. Follow-up coned-down inverted chest radiograph on postoperative day 11 (Fig. 150.1B) reveals approximately 2.0 cm lateral displacement of the sixth cerclage wire (annotations). Sternal Wound Dehiscence Sternal Wound Dehiscence with Mediastinitis Fig. 150.1 Median sternotomy is the preferred surgical approach to expose the mediastinum, pericardium, heart, and great vessels. Surgical complications occur in 5% of patients and include wound dehiscence, mediastinitis, and sternal osteomyelitis. Deep sternal wound infections arise from hematogenous seeding of the wound, or from direct extension of an adjacent infection. Staphylococcal species are responsible in most cases. Dehiscence usually develops within the first 7–10 days following surgery. Risk factors include hypertension, tobacco abuse, insulin-dependent diabetes, obesity, intra-aortic balloon pump, immunosuppression, prolonged bypass time and/or prolonged mechanical ventilation, female gender, re-operation, and harvest of both internal mammary arteries. Signs and symptoms include wound pain with or without drainage, sternal instability, palpable sternal clicking with deep breathing or coughing, fever, and leukocytosis. Normal postoperative sternotomy incision pain usually subsides over the first month. • Mid-sternal stripe of lucency on frontal exams: originally believed to be indicative of sternal dehiscence, now recognized as normal postoperative finding until sternal halves reunite (Fig. 150.2)
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Clinical Findings
Imaging Findings
Chest Radiography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree