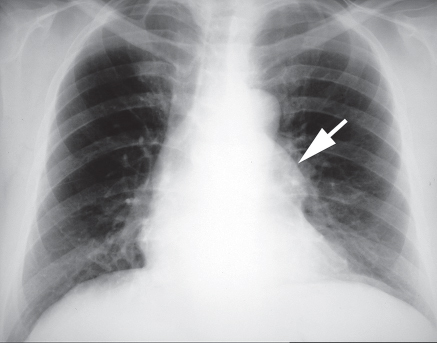
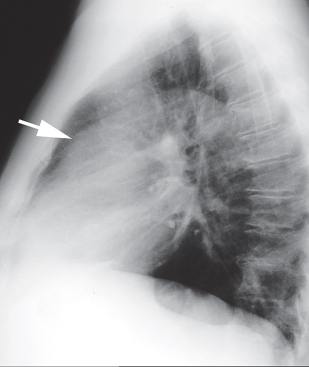
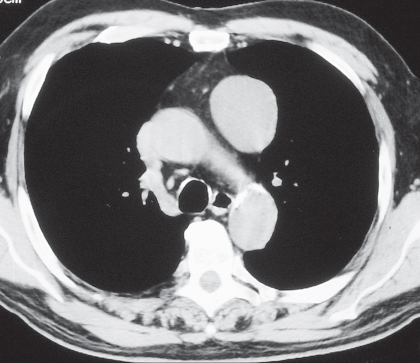
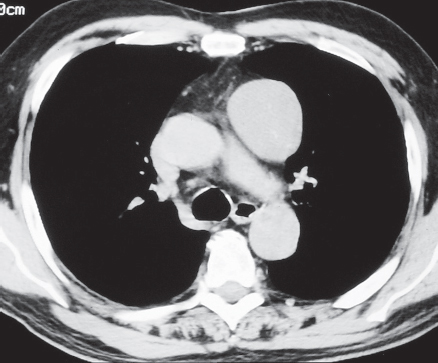
CASE 153 Asymptomatic 68-year-old man PA (Fig. 153.1) and lateral (Fig. 153.2) chest radiographs demonstrate a well-defined left anterior mediastinal mass (arrows). Contrast-enhanced chest CT (mediastinal window) (Figs. 153.3, 153.4) shows a well-circumscribed ovoid homogeneous soft-tissue mass located in the left lobe of the thymus. A tissue plane separates the mass from the adjacent great vessels. Thymoma; Encapsulated • Thymoma, Invasive • Thymic Carcinoid • Thymic Carcinoma • Lymphoma Thymoma is an epithelial neoplasm of the thymus. It represents the most common primary neoplasm of the thymus and the most common primary neoplasm of the anterior mediastinum. The recent classification of thymoma by the World Health Organization is based on epithelial cell morphology and lymphocyte-to-epithelial cell ratios. It groups thymomas into types A, AB, B1, B2, and B3, which have been further characterized as low-risk (A, AB, B1) and high-risk (B2, B3) thymomas. Thymomas may also be classified as encapsulated or invasive. Fig. 153.1 Fig. 153.2 Fig. 153.3 Fig. 153.4 The etiology of thymoma is unknown. Thymoma is associated with systemic and autoimmune disorders (parathymic syndromes) such as myasthenia gravis, hypogammaglobulinemia, and pure red cell aplasia as well as a variety of non-thymic neoplasms. Patients with thymoma are typically adult men and women who usually present after the age of 40 years (in the fifth and sixth decades of life), although all age groups are affected. While many patients with thymoma are asymptomatic, approximately one-third present with chest pain, cough, dyspnea, and/or symptoms related to local invasion by the tumor (including superior vena cava syndrome). Approximately 15% of patients with myasthenia gravis have thymoma, and up to 50% of patients with thymoma develop myasthenia gravis. Other parathymic syndromes include pure red cell aplasia, polymyositis, systemic lupus erythematosus, rheumatoid arthritis, thyroiditis, and acquired hypogammaglobulinemia.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
Clinical Findings
Imaging Findings
Chest Radiography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine