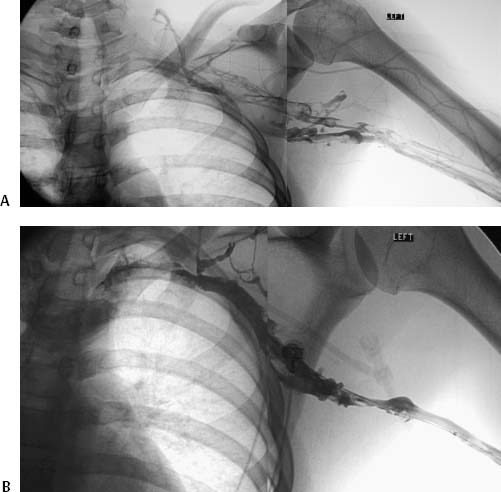
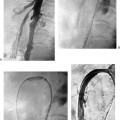
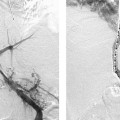
CASE 16 A 31-year-old minor league pitcher with a history of intermittent left-arm tenderness and swelling presented to the emergency room with an acute episode of marked pain and swelling after a game. Figure 16-1 Diagnosis and treatment of Paget-Schroetter syndrome. (A) Left-arm venogram performed by contrast injection of a left-hand IV shows thrombosis of the brachial, axillary, and subclavian veins. (B) Left-arm venogram after catheter-directed infusion of recombinant tissue plasminogen activator for 4 hours shows partial thrombolysis. (C) Repeat venogram after overnight infusion shows patent axillary and subclavian veins with occlusion at the level of the thoracic inlet. (D) Angioplasty was performed using a 12-mm balloon. (E) Repeat venography shows patency with persistent stenosis at the thoracic inlet. A left-arm venogram (Fig. 16-1A) performed by contrast injection through a left-hand intravenous (IV) line showed thrombosis of the left brachial, axillary, and subclavian veins with minimal development of collateral circulation. Paget-Schroetter syndrome (PSS). The ipsilateral basilic vein was punctured using direct sonographic guidance, and the occluded axillary and subclavian veins were traversed using a hydrophilic glide wire. A multiside-hole catheter was passed into the clot. Thrombolysis was performed overnight using recombinant tissue plasminogen activator (rTPA), infused at a rate of 0.5 mg/h with heparin infusing through a peripheral IV at 200 U/h. A repeat venogram performed after 4 hours of rTPA infusion (Fig. 16-1B) showed partial thrombolysis, and infusion was continued overnight. The patient reported progressive improvement of arm swelling overnight, and complete thrombolysis was achieved over 27 hours (Fig. 16-1C). At this time, complete occlusion was present at the level of the thoracic inlet with the arm in the neutral position, and angioplasty was performed to a diameter of 12 mm to bridge the gap to surgical intervention. Patency with persistent stenosis was achieved at the thoracic inlet (Fig. 16-1E). One week later, the patient underwent successful first rib resection and release of the anterior scalene muscle. Two years later, he is symptom-free and pitching again. PSS describes central venous thrombosis, typically involving the axillary and subclavian veins (Fig. 16-1). This syndrome affects young patients (mean age, early to mid thirties), and has a slight male predominance (55%). The underlying cause is venous compression at the level of the thoracic inlet. The finding of venous compression without associated thrombosis has often been called thoracic inlet syndrome (Fig. 16-2
Clinical Presentation
Radiologic Studies
Diagnosis
Treatment
Equipment
Catheter-Directed Thrombolysis
Discussion
Background
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree