Fig. 20.1
A 16-year-old girl with a dysembryoplastic neuroepithelial tumor (DNET) and partial seizures. Sagittal (a) and axial (b) 18F-DOPA–PET/MRI fusion images show no significant radiotracer accumulation by the right temporal lesion (yellow arrow in a)
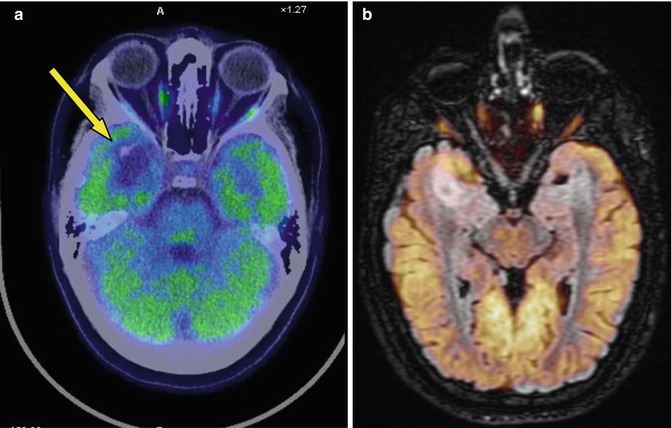
Fig. 20.2
Same patient. Axial 18F-FDG–PET/CT (a) and PET/MRI (b) fusion images show no significant radiocompound fixation in the temporal lesion (low metabolic lesion). On brain window CT, the lesion is well demarcated and hypodense (yellow arrow in a)
Case 2
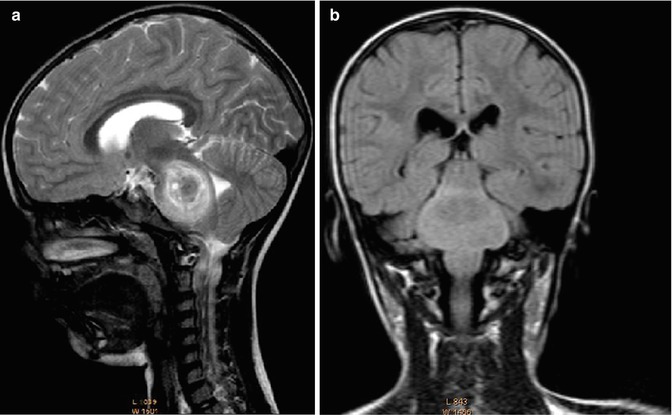
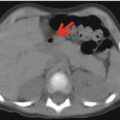
Fig. 20.3
A 5-year-old boy with headache, otalgia, diplopia, and strabismus, ataxic. (a, b) Sagittal and coronal MRI shows a large lesion of the pons that has caused its dimensional increase. The lesion appears inhomogeneous, with a parenchymal part and hemosiderin deposits. A glial tumor was suspected, but a vascular origin could not be excluded
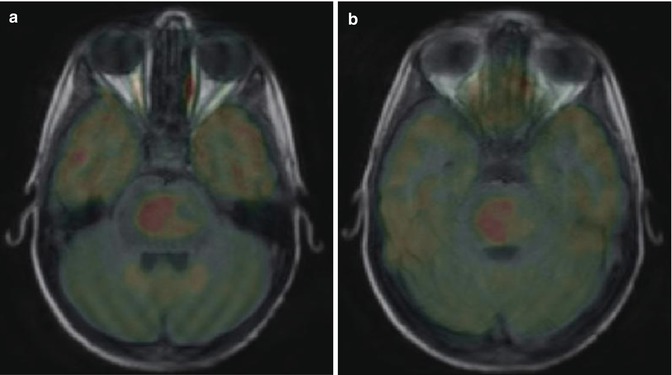
Fig. 20.4
Same patient as in Fig. 20.3. Axial PET/MRI fusion images (a, b) show the 18F-FDG-avid lesion in the pons (highly metabolic lesion); neurological view
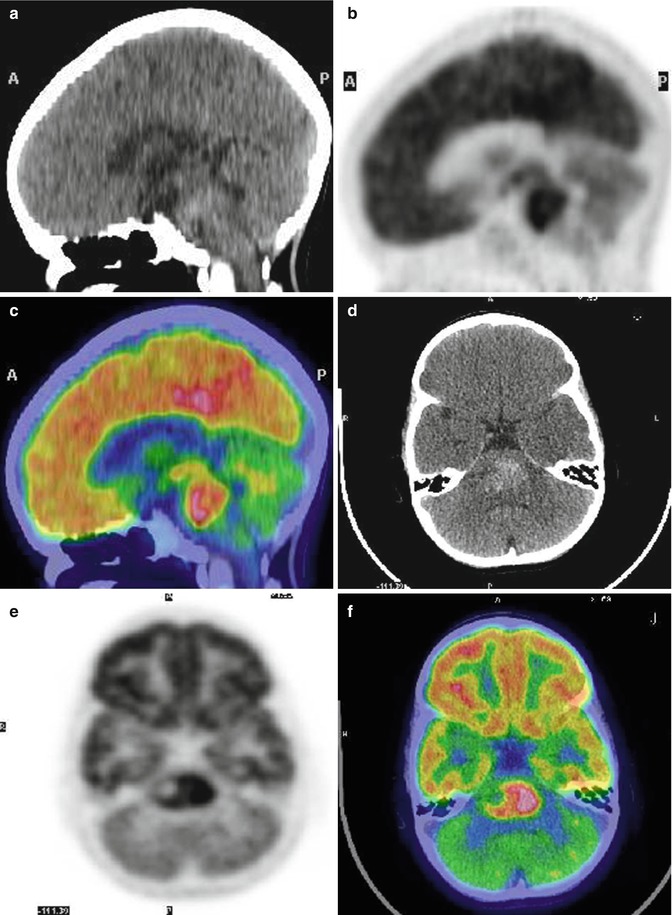
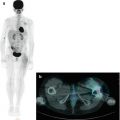
Fig. 20.5
Same patient as above. Sagittal (a–c) and axial (d–f) CT (a, d), PET (b, e) and PET/CT fusion (c, f) images show an intense FDG accumulation in the pons (SUVmax 6.19), above the cortex. To the right of the lesion is a photopenic area, indicating necrosis or hemorrhage. The high FDG accumulation suggests an aggressive lesion; neuroradiologic view. The patient died 2 months later
Teaching Point
18F-FDG–PET can be used in the differential diagnosis between high serial glial tumor and low grade and benign, e.g. vascular, lesions
In 1993, the distinct pathological entity known as dysembryoplastic neuroepithelial tumor (DNET) was entered into the WHO classification of brain tumors as a grade I tumor of neuroepithelial origin [1–3]. On neuroimaging, DNETs are cortical lesions with little mass effect and a predilection for the temporal lobes (Figs. 20.1 and 20.2). On computed tomography, DNETs are typically well-demarcated, hypodense, cortical lesions that in some cases cause a deformation of the overlying skull. Magnetic resonance images often show a solid and cystic mass, with the cystic portions appearing slightly more intense than cerebrospinal fluid.
Case 3
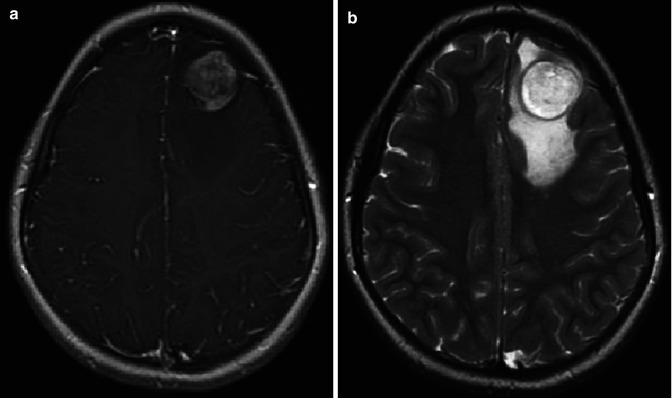
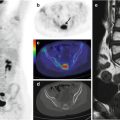
Fig. 20.6
An 11-year-old girl underwent liver transplantation 6 years earlier due to biliary atresia. Following a loss of consciousness, she was evaluated by MRI. Axial T1 (a) and T2 fast spin-echo (b) sequences show a superior frontal gyrus lesion, with a large edema component, surfacing the cortex. Spectroscopy and perfusion analysis showed an increase in the Cho/Cr ratio, a decrease in the NAA/Cr ratio, and an increase in relative cerebral blood volume (rCBV)
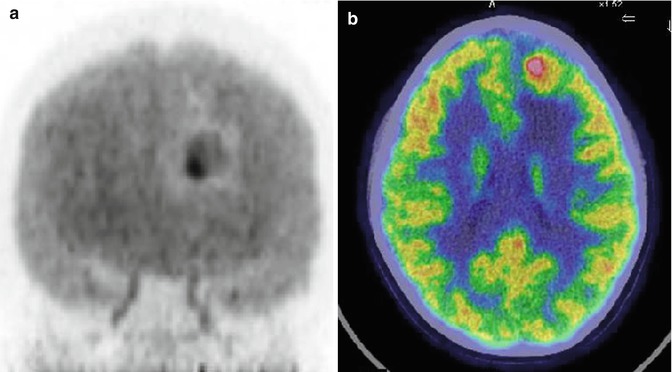
Fig.20.7




(a) Maximum imaging projection (MIP) and (b) axial PET/CT fusion images show the FDG-avid lesion in the left frontal lobe. On the MIP, note the photopenic area surrounding the highly metabolic component of the lesion due to edema. The patient underwent surgery. The finding was ganglioglioma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree