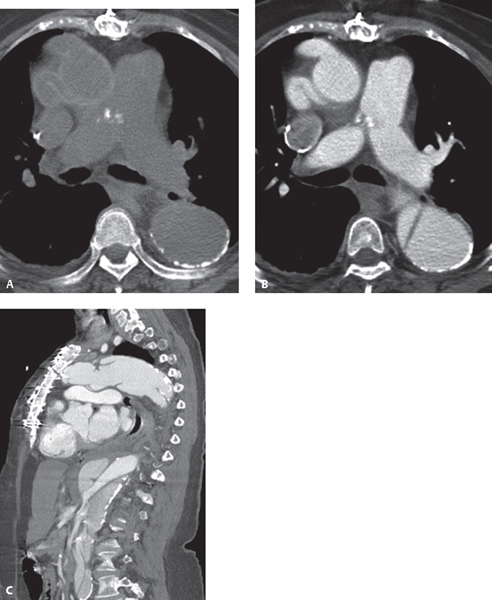
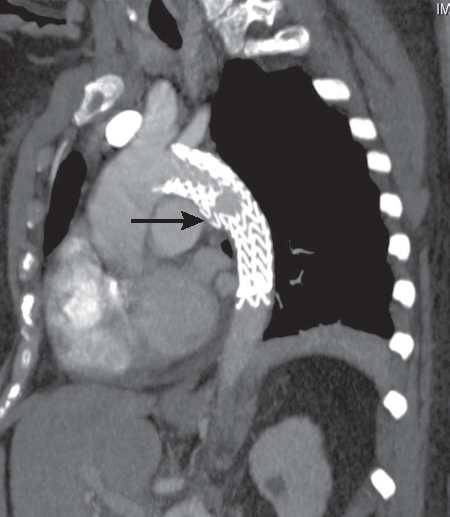
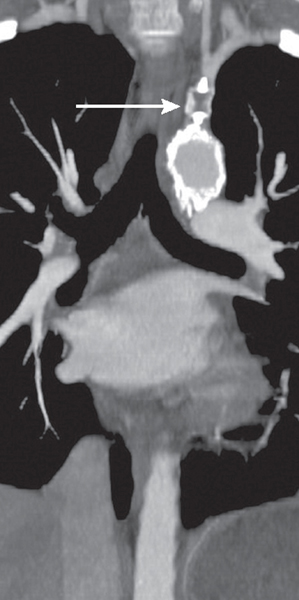
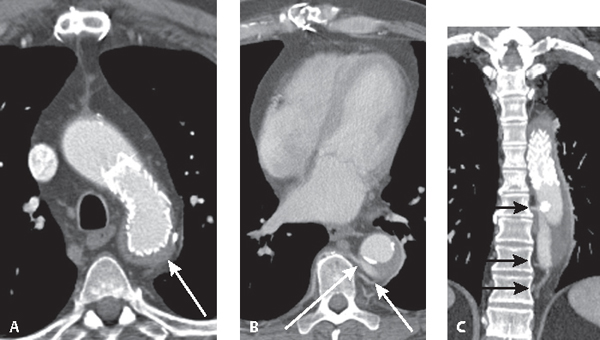
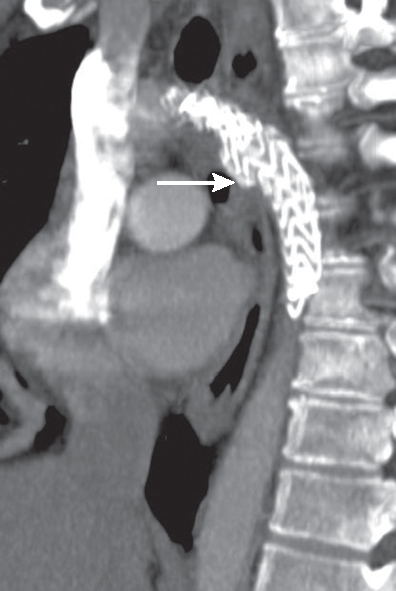
CASE 192 Series of five unrelated patients who share in common the surgical placement of synthetic interposition grafts or the deployment of endovascular stent grafts Unenhanced (Fig. 192.1A) and contrast-enhanced (Fig. 192.1B) axial and sagittal oblique CTAs (Fig. 192.1C) of a 70-year-old woman following total ascending aorta and aortic arch replacement with “elephant trunk” reconstruction and interposition graft and a trifurcated Gelweave (Vascutek, Inchinnan, Scotland) 12/8/8 branch vessel graft with subclavian artery reimplantation show a dissecting descending thoracic-abdominal aortic aneurysm and intimomedial flap. Sagittal oblique CTA (Fig. 192.2) of a 62-year-old man with ATAI treated with an endoluminal stent-graft demonstrates coverage of the post-traumatic pseudoaneurysm (arrow) but occlusion of the left subclavian artery origin. Coronal CTA (Fig. 192.3) of a 46-year-old man with ATAI treated with endoluminal stent-graft shows the stent-graft en face and covering the left subclavian artery origin. An Amplatzer occlusion device (AGA Medical Corp., Plymouth, MN) is seen in the proximal subclavian artery (arrow). A left-carotid-to-subclavian arterial bypass graft was performed the day before (not illustrated). Arterial phase axial CT (Fig. 192.4A) of a 63-year-old man with endovascular stent deployment for treatment of a descending aortic aneurysm shows an intramural-extra-stent collection of blood consistent with “type II endoleak” (arrow). Delayed axial (Fig. 192.4B) and coronal CTA (Fig. 192.4C) images reveal that the endoleak source emanates from the seventh, eighth, and ninth intercostal arteries (arrows). Sagittal oblique CTA (Fig. 192.5) of a 52-year-old man with ATAI treated with endoluminal stent-graft 12 months earlier and now complicated by a “type III endoleak.” Although there is coverage of the post-traumatic pseudoaneurysm, contrast media can be identified both medially (arrow) and laterally between adjacent contiguous stent-grafts. Fig. 192.1 (Images courtesy of Jennifer Hubert, MD, VCU Medical Center, Richmond, Virginia.) Fig. 192.2 Fig. 192.3 Synthetic Interposition Grafts and Endovascular Stents None Fig. 192.4 Fig. 192.5 Two common techniques of aortic root graft repair are the interposition graft and inclusion graft. An inter-position graft entirely replaces the diseased segment of aorta, which is resected and removed. All vascular branches, including the coronary arteries, are reimplanted. Radio-opaque vascular pledgets and rings are used to reinforce the various anastomoses and cannulation sites (Fig. 192.6). An inclusion graft is inserted directly into the aortic lumen, leaving a potential space between the native aorta and graft. This potential perigraft space may continue to have persistent slow blood flow of little clinical consequence or eventually thrombose. Complex, extensive thoracic aortic aneurysms are difficult and challenging to manage. A single operative procedure replacing the ascending aorta, arch, and descending thoracic aorta subjects the patient to a prolonged procedure, multiple incisions, longer cross-clamp times, and increased blood loss. In the past, difficulty establishing proximal control of the aorta during staged repairs was often complicated by excessive and sometimes catastrophic bleeding. In 1983, the elephant trunk two-stage technique for reconstructing the diseased aorta was introduced. Stage I involves graft replacement of the ascending aorta and aortic arch with or without separate valve replacement. The distal portion of the graft is inverted and its folded edge is sutured to the descending aorta just distal to the left subclavian artery and the outer “windsock” portion or “elephant trunk” is left “hanging” in the descending aorta (Figs. 192.1C, 192.7A). Stage II is performed at a later date, during which time this portion of the graft is retrieved and the distal anastomosis completed (Fig. 192.7B). The technique obviates cross-clamping of the proximal aorta, reducing bleeding and other complications.
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Synthetic Interposition Grafts
Complications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine