Inflammation |
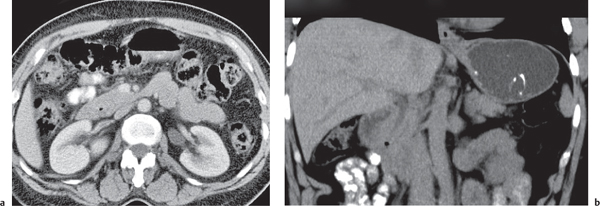
Cholecystolithiasis
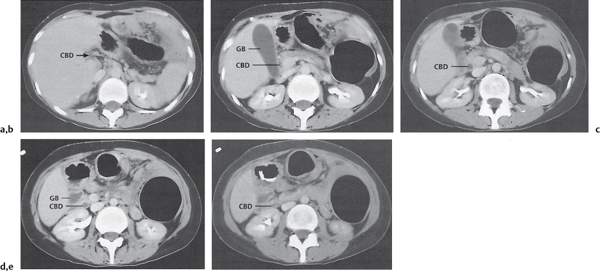
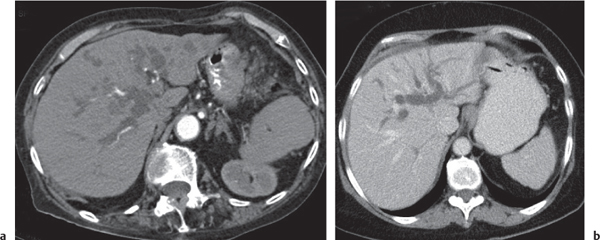
Fig. 20.4a–e |
Gallstones are composed of cholesterol, pigment (calcium bilirubinate), or a mixture of both. Stones are visible only if density is different than bile. Gaseous stones accrue by dehydration and excavation. Sludge consists of small cholesterol and pigment granules.
Scan recommendation:
Nonenhanced CT, although ultrasound is the imaging modality of choice.
Diagnostic pearls: Typically, pure cholesterol stones are large and iso-/hypodense as compared with bile. Pigmented stones are hyperdense, numerous, and small. Mixed stones either are masked by bile or are peripherally calcified with a hypodense center. Gaseous stones show central hypodense air streaks. Sludge appears slightly more dense than bile and may effect an intracystic sludge/bile level. |
Gallstones are usually accidental findings on CT scans. CT’s sensitivity to detect gallstones amounts to 80% at maximum. Dual-energy CT is favorable, as cholesterol stones are nicely visualized at high-kilovolt peaks. Gallbladder folds may simulate (rimmed) gallstones. Consider the 5F‘s (female, 40, fertile, fat, fair) as predisposing factors for cholecystolithiasis. |
Choledocholithiasis
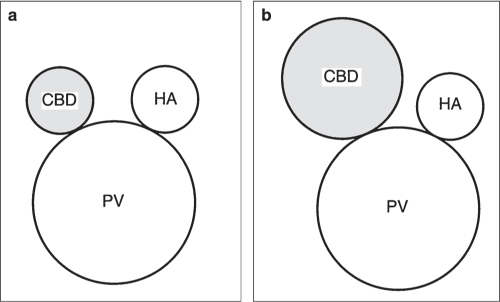
Fig. 20.5a, b |
Presence of gallstones in intra- or extrahepatic bile ducts with or without duct obstruction. The latter initially leads to extra-hepatic cholestasis followed by intrahepatic cholestasis.
Scan recommendation:
Nonenhanced CT, although magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiography (ERCP) are imaging modalities of choice. Cholesterol stones are visualized as hypodense filling defects. Pigmented stones usually appear hyperdense.
Diagnostic pearls: Rule out dilation and truncation of CBD (normally < 6 mm) and cholestasis proximal to it.
Twenty percent of stones are seen as homogeneous, high-attenuation structures within the water-attenuation bile or surrounded by soft tissue density of the duct. About 50% of stones are of soft tissue density and are recognized as target lesions surrounded by low-density bile or as a crescent sign. |
Cholangiography is the examination of choice.
Approximately 93% of all stones are secondary gallstones due to cholecystectomy, hyperalimentation, hemolytic anemias, metabolic syndrome, or ileocecal resection; ≤ 7% are primary duct stones due to bile duct sclerosis (recurrent cholangitis), congenital bile duct anomalies, motor disorder of the papilla of Vater, foreign bodies, or parasites.
Typical clinical signs are acute abdominal pain. Persistent choledocholithiasis may lead to pruritus, jaundice, and pancreatitis. Whereas small stones may pass spontaneously or could be fragmented by mechanical lithotripsy, larger stones usually require endoscopic sphincterectomy or surgical removal.
Thin collimation (≤ 1 mm) is necessary to display stones and ducts. Consider dual-source CT for better depiction of cholesterol stones. |
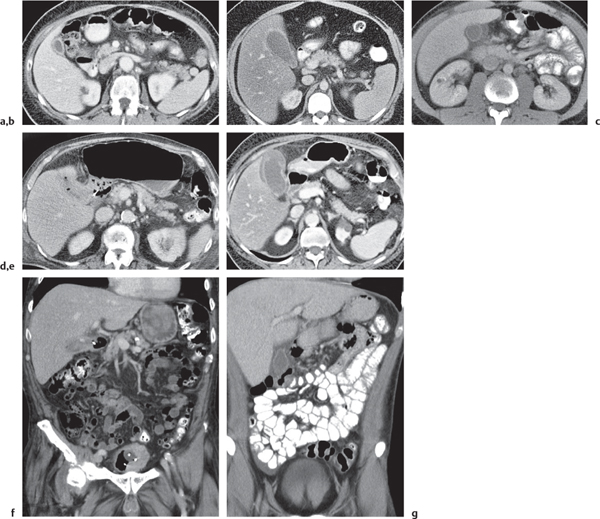
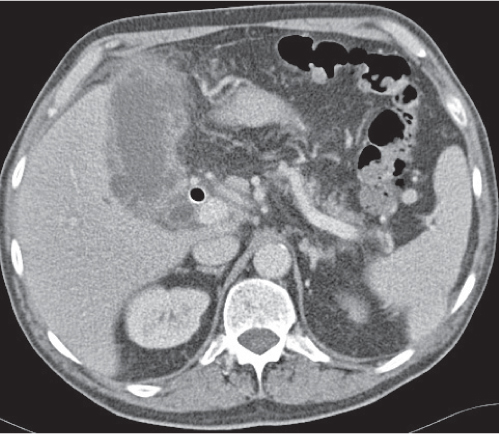
Cholecystitis
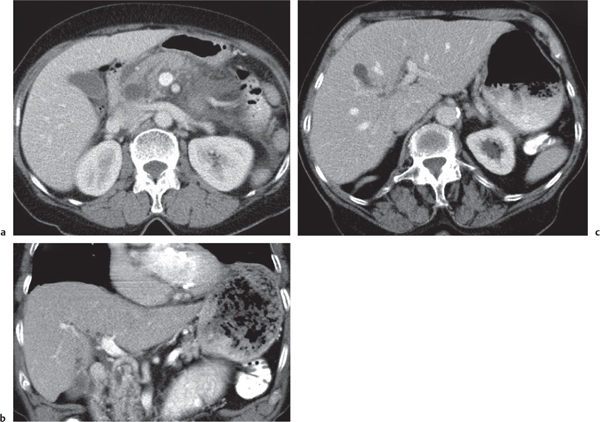
Fig. 20.6a–g |
Acute inflammation of gallbladder mainly (> 95%) due to cystic duct obstruction, to a lesser extent also due to secondary infection, inflammation, or ischemia.
Scan recommendation:
Multiphasic CT (nonenhanced CT, parenchymal phase [PP]). Nonenhanced CT: Regular thickening of gallbladder wall (> 3 mm) and stranding of pericholecystic fat, with or without gallstones.
PP: Hyperattenuation of gallbladder wall, often showing three layers (hypodense wall edema within hyperdense inner and outer layer); also, pericholecystic fluid/stranding of fat.
Diagnostic pearls: Thickened gallbladder wall and cholelithiasis are not suggestive of cholecystitis. Increased density of bile (> 20 HU), loss of clear demarcation of the gallbladder wall, and gallbladder lumen dilation (hydrops > 5 cm) are more specific findings. |
Marked contrast enhancement of the gall-bladder wall is typically seen in acute but not chronic cholecystitis.
Irregular wall thickening with zones of low density and pericholecystic fluid collection are suggestive of complicated cholecystitis. Air within gallbladder lumen or wall is indicative of emphysematous cholecystitis (typically > 24 h after onset of symptoms). Focal interruption of gallbladder wall is a sign of rupture/necrosis.
Irregular thickening of gallbladder wall, occasionally with calcifications and pericholecystic extension, typically is observed in the presence of xanthogranulomatous cholecystitis but also gallbladder carcinoma. |
Adenomyomatosis |
Nonspecific localized thickening of gallbladder wall and/or presence of intraluminal diverticula.
Scan recommendation:
Contrast-enhanced CT (DP): ~30 min after contrast administration (Biliscopin).
Diagnostic pearls: Localized isodense, wall-adherent noduli surrounded by hyperattenuating bile fluid. |
Hyperplastic mucosa, thickening of the muscularis, and expression of intramural diverticula (Rokitansky–Aschoff sinuses) are usually better depicted on MRCP or ultrasound. Predominantly found in the fundus of the gallbladder. Delayed scans after intravenous (IV) administration of Biliscopin are the only CT option to correctly visualize intraluminal diverticula. |
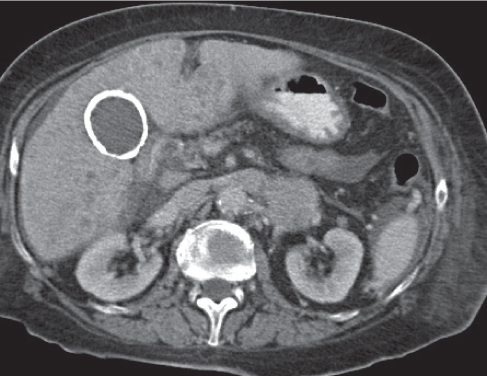
“Porcelain” gallbladder
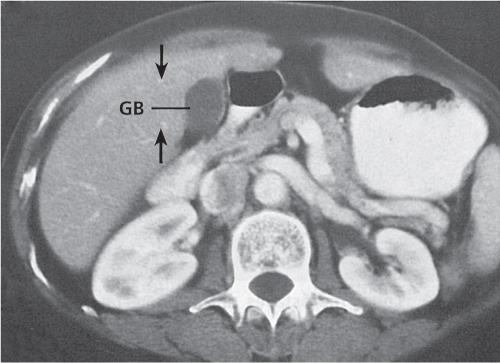
Fig. 20.7 |
(Partly) calcified gallbladder wall.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP): Mural calcifications visible on all scans.
Diagnostic pearls: Calcification of the gallbladder wall. |
Etiology unknown, most likely due to recurrent cholecystitis with accumulation of calcium carbonate in the wall of the gall-bladder. Predisposing factor for gallbladder carcinoma. |
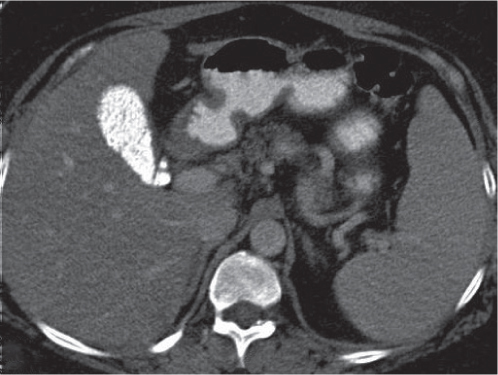
Milk of calcium bile
Fig. 20.8 |
Calcium carbonate collecting within gallbladder.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP).
Nonenhanced CT: High attenuating (> 140 HU) fluid within gallbladder.
PP: Gallbladder wall may or may not enhance.
Diagnostic pearls: Calcified liquid within the gallbladder. |
Rare; incidence < 0.3% of CT scans. Typically due to gallbladder stasis. Occurs in middle-aged patients, more often in women than men. |
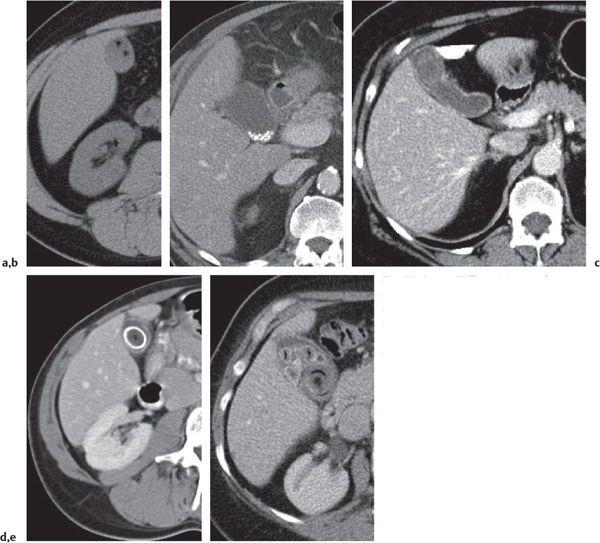
Primary sclerosing cholangitis (PSC)
Fig. 20.9a, b |
A chronic idiopathic inflammation of intra- and extrahepatic bile ducts.
Scan recommendation:
Multiphasic CT (nonenhanced CT, PP, delayed phase [DD]). Nonenhanced CT: Discontinuous dilation of bile ducts, which are partly filled with high-attenuating intraluminal calculi; in end stage, hypoattenuation of periportal region (fibrosis).
PP: Slight enhancement of bile duct walls.
DP: Late enhancement of periportal fibrosis.
Diagnostic pearls: Cirrhotic liver with late-enhancing periportal fibrosis and discontinuous dilation of bile ducts, which are partly filled with high-attenuating calculi. |
PSC typically affects young (< 50 y) male (> 70%) patients and is associated with other autoimmune diseases (e.g., Crohn disease, ulcerative colitis, and retroperitoneal fibrosis). Histologic features are bile duct destruction and severe periportal fibrosis. End stage of the disease is severe liver cirrhosis.
Clinical symptoms are intermittent abdominal pain, obstructive jaundice, and elevated liver enzymes. Imaging modality of choice is MRI/MRCP, although diagnosis often is possible only with ERCP. Liver transplantation is the sole treatment option. |
Congenital |
Choledochal cyst
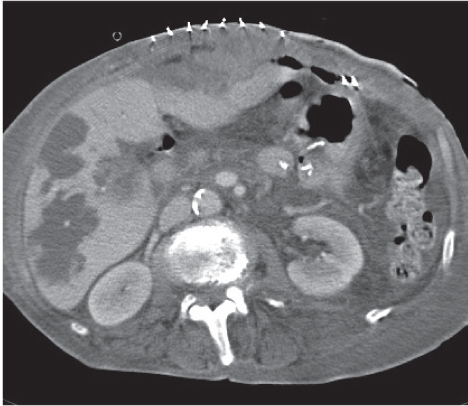
Fig. 20.10a–c |
Segmental dilation of any portion of bile ducts, predominantly of the common duct.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP).
Nonenhanced CT: Well-demarcated, near-water density cyst within bile ducts, with or without dilation of the ductal system.
PP: Slight enhancement of bile duct walls may be observed, but no enhancement of cysts.
Diagnostic pearls: Nonenhancing intra- and extrahepatic cystic lesions with direct affiliation to the bile ducts. Thirty minutes after Biliscopin, choledochal cyst will fill with contrast media; any other cystic lesions will not. |
A noncritical congenital malformation of large bile ducts, typically diagnosed during childhood and classified into five different types according to Todani (see introduction to this chapter). Clinical symptoms are intermittent abdominal pain, pruritus, and jaundice. Imaging modality of choice is MRI/MRCP. Complications (cholangitis/pancreatitis) may require surgical repair. Rule out other cystic lesions, including hepatic and pancreatic cysts, fluid collections, and enteric duplication cysts as differential diagnoses. |
Caroli disease
Fig. 19.10a, b , p. 679 |
Multifocal segmental saccular dilation of intrahepatic bile ducts (Todani cysts type V).
Scan recommendation:
Multiphasic CT (nonenhanced CT, PP).
Nonenhanced CT: Multiple near-water-density, dilated intrahepatic bile ducts.
PP: Very discrete central enhancement in cysts representing portal vein radicles.
Diagnostic pearls: Multiple low-attenuation cystic lesions are seen throughout the liver associated with dilated intrahepatic bile ducts. Dilated bile ducts may surround the accompanying portal vein radicles in a pathognomonic fashion. Intrahepatic stone disease is often associated. |
Rare congenital abnormality characterized by segmental dilation of intrahepatic bile ducts. Associated with cystic lesions of the kidneys. May simulate polycystic liver disease. Administration of biliary contrast agent (Biliscopin) 30 min prior to CT demonstrates contiguity of the cystic lesions with the biliary tree. Caroli syndrome is Caroli disease plus hepatic fibrosis. Clinical symptoms of CD are intermittent abdominal pain, pruritus, fever (cholangitis), and jaundice. Overall prognosis is poor.
MRI/MRCP is imaging modality of choice. |
Common bile duct (CBD) diverticulum |
Diverticulum-like outpouchings of extrahepatic bile ducts in the presence of otherwise normal-sized bile ducts.
Scan recommendation:
Contrast-enhanced CT (DP): ~30 min after contrast administration (Biliscopin).
Diagnostic pearls: Localized isodense and wall adherent diverticula are surrounded by hyperattenuating bile fluid. |
Congenital diverticula of the CBD are uncommon. Diverticula in the intrahepatic ducts are rare.
MRI/MRCP is imaging modality of choice. |
Trauma |
Gallbladder trauma |
Traumatic rupture of the gallbladder wall.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP).
Nonenhanced CT: Gallbladder often not discernible but distinct hypodense fluid in pericholecystic fat. High- attenuation of bile/high-attenuation of intra- or extracystic clots typically represents hemorrhage.
PP: Gallbladder remains not discernible; blood and extracystic fluid remain isodense as on nonenhanced CT.
Diagnostic pearls: Fluid collection in pericystic fat after trauma. |
Often associated with laceration of the liver as well as the head/corpus of the pancreas. Typically observed in the wake of seat-belt injuries.
Contrast material, milk of calcium bile, and gallstones should be excluded before making the diagnosis of hemobilia pericystic hemorrhage.
Due to self-limitation of bleeding (intra-abdominal compartments), a no-touch treatment may often be favorable to laparotomy. |
Postoperative fistula or cystic duct remnant |
Postoperative leakage (fistula) after bile duct surgery or cystic duct remnant after cholecystectomy.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP).
Nonenhanced CT: Irregular cavity or tubular duct remnant isodense to CBD.
PP: Slight enhancement in periphery of irregular cavity. Tubular duct remnant remains isodense to CBD.
Diagnostic pearls: Irregular fluid collection with discrete peripheral contrast enhancement seen after bile duct surgery. |
Patients with duct remnants often present symptoms similar to a cholecystitis. On the other hand, patients with fistulas may be symptom-free. If fistulas become secondary infection, typical symptoms are fever and abdominal pain.
Caveat: Duct remnants may contain gallstones. |
Infection |
Ascending (acute suppurative) cholangitis
Fig. 20.11 |
Acute inflammation of intra- and extrahepatic bile ducts due to ascending infection.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP). Nonenhanced CT: Dilated bile ducts appear either hypo- or hyperdense (pus), obstructing stones hypo-/iso-/hyperdense to bile. PP: Slightly hyperdense thickened bile duct wall. Demarcation of associated hepatic abscesses if present.
Diagnostic pearls: Dilated bile ducts are seen filled with hyperattenuating material on precontrast scans and with distinct mural hyperattenuation on postcontrast scans. |
Occurs typically due to acute bile duct obstructions (intraductal stones/iatrogenic/external lesions) after manipulation of bile ducts/pancreatic ducts during ERCP or after surgery (e.g., biliodigestive anastomosis/Whipple operation).
Acute cholangitis usually caused by Escherichia coli infection. May quickly proceed to liver abscesses. Treatment of choice is antibiotic therapy and removal of obstructing agent. |
Recurrent pyogenic cholangitis |
Intra- and extrahepatic bile duct dilation (up to 3–4 cm in diameter) with associated biliary calculi and debris.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP).
Nonenhanced CT: The density of biliary stones is variable—usually either iso- or hyperdense as compared with normal liver parenchyma.
PP: Markedly dilated, near-water-density extra- and intrahepatic bile ducts with slightly hyperdense, mildly thickened (2–3 mm) duct walls.
Diagnostic pearls: Distinct cholestasis with numerous intra- and extrahepatic biliary stones but lacking gallbladder stones. |
Endemic in Southeast Asia; also known as Asian cholangiohepatitis, intrahepatic pigment stone disease, and biliary obstruction disease. Parasites and bacteria are suspects as the cause. Typical clinical symptoms are recurrent fever, abdominal pain, and jaundice. Severe complications include liver abscess, biliary cirrhosis, and cholangiocarcinoma. Treatment of choice is long-term antibiotic therapy, surgical/interventional/endoscopic biliary drainage, and sphincterotomy. Differential diagnosis: cholangiocarcinoma (delayed enhancement on DP scans). |
Worm infestation |
Intraductal colonization of parasites/worms.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP). Nonenhanced CT/PP: Soft tissue filling defects with or without obstruction of the bile ducts.
Diagnostic pearls: Soft tissue filling defects with distinct cholestasis and lacking gallbladder stones. |
Ascaris and liver flukes ascend from the duodenum into the bile ducts. Liver flukes (Clonorchis sinensis and Fasciola hepatica) are nematodes measuring 1 to 2 cm in length. They inhabit smaller bile ducts and form oval or linear filling defects. Echinococcus may cause partial obstruction due to cyst membranes, daughter cysts, or scolices discharged from a communicating hepatic cyst. |
Neoplasms |
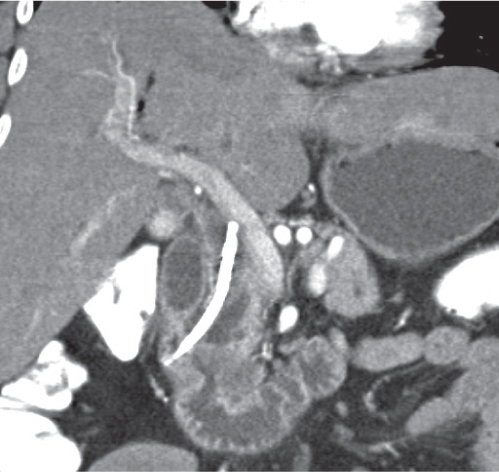
Cholangiocarcinoma Fig. 20.12 |
Intraductal neoplasm originating from epithelium of bile ducts.
Scan recommendation:
Multiphasic CT (nonenhanced CT, AP, PP).
Nonenhanced CT: Often not discernible though hypodense lesion within dilated intra- or extrahepatic bile ducts.
AP: Intrahepatic tumors often show an early peripheral enhancement subsequently followed by scattered central enhancement.
PP: Distinct enhancement of bile duct walls.
Diagnostic pearls: Mass at the level of bile duct bifurcation, hilar lymph nodes, distinct intrahepatic cholestasis, and biliary obstruction (Klatskin tumor). |
Any obstruction between the level of confluence of hepatic ducts and the pancreatic portion of the common biliary duct is highly suspicious for cholangiocarcinoma. Cholangiocarcinoma usually arises in larger bile ducts and is identifiable on CT scans in 70%. Often associated with ulcerative colitis, sclerosing cholangitis, liver fluke disease, gallstones, and choledochal cysts. Treatment of choice is surgery or biliary stenting. Radiation therapy may be applied in a more palliative setting. Poor overall outcome (mean survival rate 6 months after diagnosis). Cholangiocarcinoma is typically accompanied by global intrahepatic bile duct dilation, whereas metastases or primary liver tumors usually cause either no or only segmental bile duct dilation. |
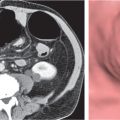
Ampullary carcinoma
Fig. 20.13 |
Adenocarcinoma of the ampulla of Vater arising from epithelial cells of the CBD.
Scan recommendation:
Multiphasic CT (nonenhanced CT, acute phase [AP], PP). Nonenhanced CT: Soft tissue mass at papilla of Vater, cholestasis, and dilation of the pancreatic duct (double duct sign).
AP: Ampullary mass hypodense as compared with pancreas.
PP: Mass becomes isodense to pancreas.
Diagnostic pearls: Mass at papilla of Vater with double duct sign and peripancreatic lymph nodes. |
Often indistinguishable from primary pancreatic neoplasm; thus, scan parameters should allow parallel assessment of the pancreas: hydro-CT (100 mL of water orally 5 min prior to examination, 5 mL Buscopan IV); biphasic CT (AP/PP) thin-slice collimation and coronal MPR. Treatment of choice is surgery (Whipple operation). Overall prognosis is poor: 5-y survival rate < 40%. |
Gallbladder carcinoma
Fig. 20.14 |
Malignant neoplasm in > 90% of cases originating from epithelial cells of gallbladder wall.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP).
Nonenhanced CT: Eccentric thickening of the gallbladder wall/focal mass protruding into the gallbladder lumen, partly calcified.
PP: The mass usually enhances well.
Diagnostic pearls: Direct tumoral extension into the liver and portal vein is a frequent finding. |
Gallbladder carcinoma associated with “porcelain” gallbladder and chronic inflammation due to gallstones. Affects mainly women (> 75%). Often simulates inflammatory gallbladder disease, especially in presence of gallstones or adjacent liver invasion. Cholecystectomy is treatment of choice. |
Biliary intraductal papillarymucinous neoplasm (IPMN) |
IPMN of bile ducts.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP).
Nonenhanced CT: Segmental dilation of intra- and/or extra-hepatic bile ducts.
PP: Intraductal mass tends to attenuate after contrast but is usually not distinguishable from bile fluid.
Diagnostic pearls: Segmental intrahepatic bile duct dilation without reasonable “downstream” obstruction. |
Very rare disease, mainly affecting Southeast Asian populations. In presence of nodal-free disease, promising good prognosis after surgical resection of affected liver segments. Differential diagnosis: Klatskin tumor (usually leads to global intrahepatic cholestasis). |
Pancreatic or metastatic carcinoma
Fig. 22.14 , p. 727 |
Abrupt bile duct interruption due to surrounding soft tissue mass.
Scan recommendation:
Biphasic CT (nonenhanced CT, PP).
Nonenhanced CT: Global dilation of intra- and/or extrahepatic bile ducts.
PP: Differentiation of retroperitoneal structures, lymph nodes, liver, and biliary system.
Diagnostic pearls: Ill-defined mass in portal region leading to abrupt bile duct interruption and global intrahepatic bile duct dilation. |
The most common causes are pancreatic carcinoma, lymphoma, and metastases to lymph nodes in the portal region. Direct invasion from other carcinoma of adjacent organs, such as stomach, kidney, and adrenal glands, is rare. |