20 The Pericardium
Introduction
The lungs and the heart reside in separate compartments within the thoracic cavity. The lobes of the lung are located in two pleural cavities and the heart is located within the pericardial cavity, which occupies most of the lower mediastinum. The pleura and pericardium are potential fluid–filled spaces within the pleural and pericardial cavities (spaces) that are lined by thin mesothelial linings. The pericardium is composed of outer fibrous and two inner serous layers and contains a small amount of fluid. The pericardial cavity is involved in many inflammatory and malignant diseases. Along with the development of novel techniques for percutaneous access to the pericardial, increased interest in the detailed anatomy of the pericardial space and its recesses has developed. This chapter discusses the embryology and anatomy of the pericardial cavity. Common pathologies are briefly described. The epicardial and mediastinal fats are included in the discussion.
Embryology
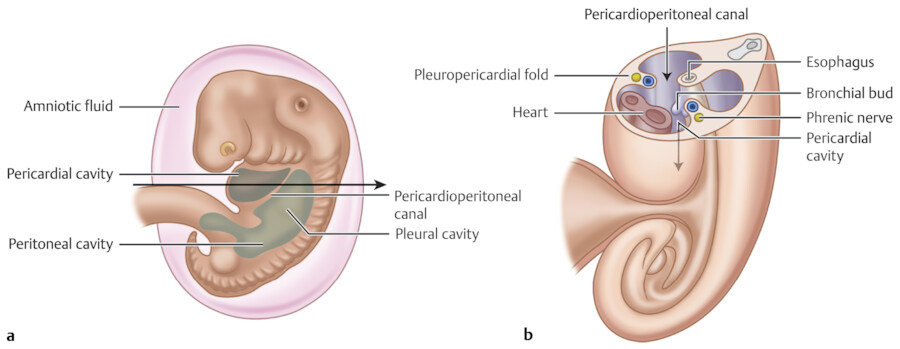
The pleural, pericardial, and peritoneal cavities originate from a single large intraembryonic coelom (cavity). The intraembryonic coelom is lined by the visceral and parietal layers of the lateral plate mesoderm, the splanchnopleura and the somatopleura, respectively. In early embryonic stage (i.e., week 4 of embryo), the intraembryonic coelom at the cranial level consists of a middle pericardial cavity and two pericardioperitoneal canals posterolaterally (Fig. 20‑1, Fig. 20‑2). Within a few days, the lung buds start to grow from the primitive mediastinal mesoderm in midline out into the pericardioperitoneal canals. At the same time, the septum transversum, from which the anterior part of the diaphragm will derive, grows to divide the pericardioperitoneal canals into the peritoneal cavity and the thoracic cavity. In the human embryo, it is suggested that initially two folds grow out of the body wall: the ventral one is called the pleuropericardial membrane (fold) and the dorsal one is called the pleuroperitoneal membrane (fold). With rapid outgrowth of the lung buds from the foregut, the pericardioperitoneal canals expand into the future pleural cavity and the primitive mesenchyme splits into two layers that form the fibrous pericardium medially and the chest wall laterally. 1 , 2 Within the fibrous pericardium remains the phrenic neurovascular bundles.
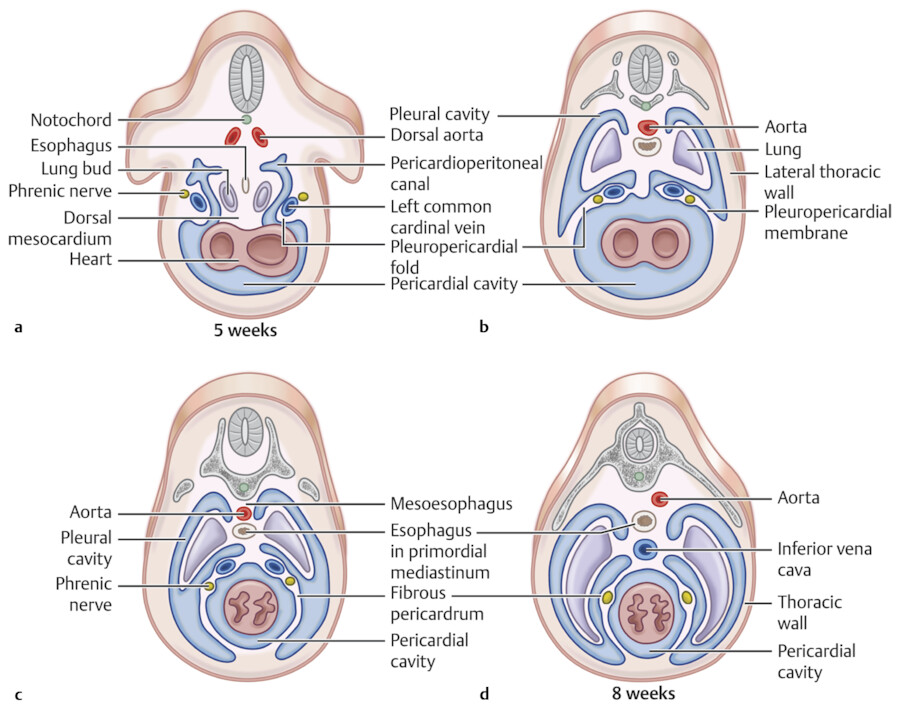
The pleuropericardial membrane on each side grows inward toward the lung hilum. By week 7, the pleuropericardial membranes fuse with the dorsal mesocardium (primitive mediastinum) to obliterate the remaining communication between the two pericardioperitoneal canals (pleural cavities) and separate them from the pericardial cavity. At the caudal end of the pericardioperitoneal canals and during week 6, the pleuroperitoneal membranes, which are attached dorsolaterally to the body wall, grow to separate the pleural cavity from the peritoneal cavity. The pleuroperitoneal membranes fuse with the dorsal mesentery of the esophagus and the septum transversum to form the posterior part of the diaphragm.
Complete separation of the pleural, pericardial, and peritoneal cavities requires an active role of the pleuropericardial and pleuroperitoneal membranes. The mechanisms that drive this process have remained obscure. It is important to know that pleuropericardial membranes contain the common cardinal veins (ductus cuvieri 1 , 2 ; Fig. 20‑2). The common cardinal veins drain the primitive venous system into the sinus horns of the primitive heart. Therefore, development of the pericardium and sinus horn formation are coupled, and sinus horn defects are tightly associated with pleuropericardial abnormalities including the pericardium. As a reminder, the sinus horns develop from pericardial precursors that differentiate into the sinus venosus myocardium around the systemic venous connections to the atrium. They form only after the outflow tract, the left and right ventricles, and common atrium have already been established. In adults, most of the right sinus horn myocardium is incorporated into the right atrium to form the sinus venarum. In humans, the left sinus horn will lose its connection to the body and forms the coronary sinus.
Pericardium
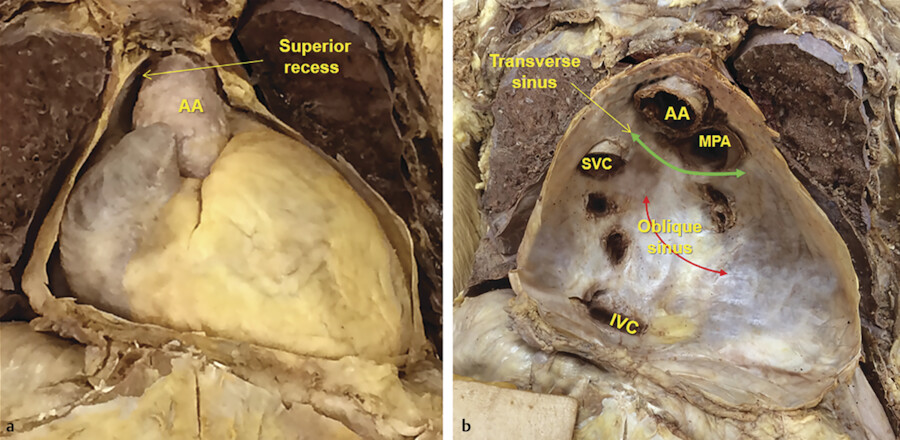
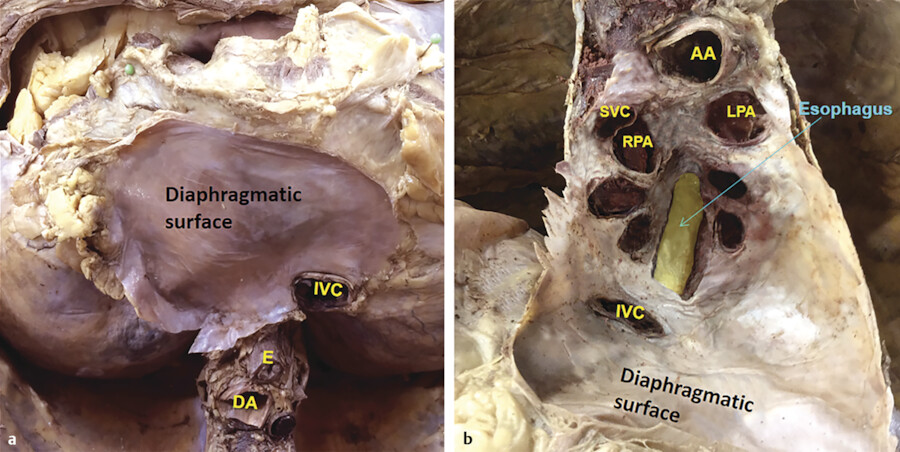
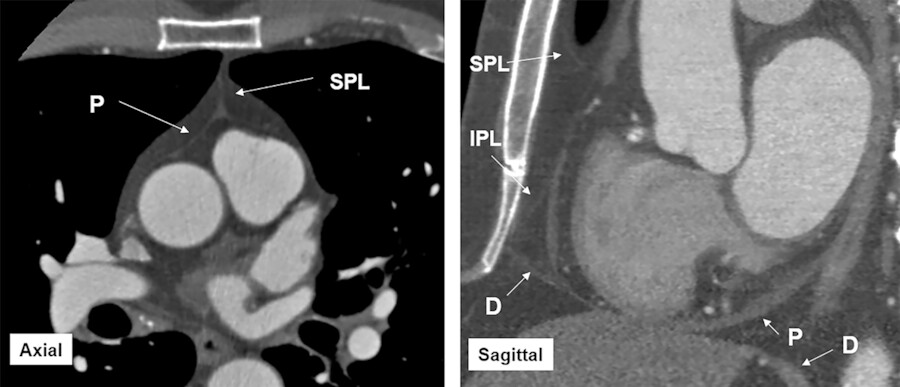
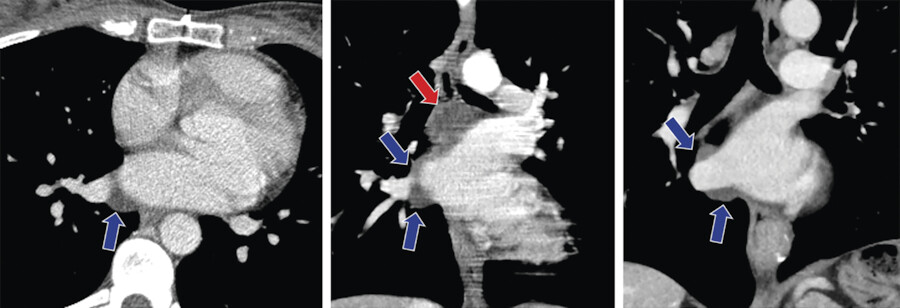
The pericardium surrounds the heart and extends out to cover part of the superior vena cava (SVC), ascending aorta, main pulmonary artery, ostial pulmonary veins, and inferior vena cava (Fig. 20‑3 , Fig. 20‑4 , Fig. 20‑5 , Fig. 20‑6). The pericardium is a flask-shaped sac consisting of an outer fibrous component and an inner double-layered serous sac that surrounds the heart. 3 , 4 , 5 The outer serous layer, which is closely attached to the fibrous layer is the parietal pericardium. The visceral serous pericardium, or epicardium, adheres to the heart and great vessels and forms recesses and sinuses. While the parietal layer of the pleura is largely attached to the body wall, the serous parietal pericardium is largely aligned with the free aspect of the parietal pleura (mediastinal pleura) to form a double-layered wall that is further stiffened by deposition of fibrous material between them. This fibrous material is the fibrous pericardium that is the remnant of the pleuropericardial membranes that anchors the heart in the mediastinum and separates the pericardial from the pleural cavities. 1 , 2
Normally, the pericardial sac contains 15 to 25 mL of fluid, allowing visualization of the pericardial recesses on computed tomography (CT) or magnetic resonance imaging (MRI) studies. 3 , 4 , 5 The fibrous pericardium is fused with the central tendon of the diaphragm inferiorly and with the tunica adventitia of the great vessels superiorly (Fig. 20‑6). Anteriorly, it is attached to the sternum by superior and inferior sternopericardial ligaments (Fig. 20‑7; see Chapter 3). The serosal pericardium is avascular, but the fibrous pericardium is supplied by pericardial branches of the internal thoracic artery anteriorly and the mediastinal and bronchial branches posteriorly. The phrenic nerves descend in the fibrous pericardium between it and the mediastinal pleura and send branches to the pericardium, which contain vasomotor and sensory fibers.
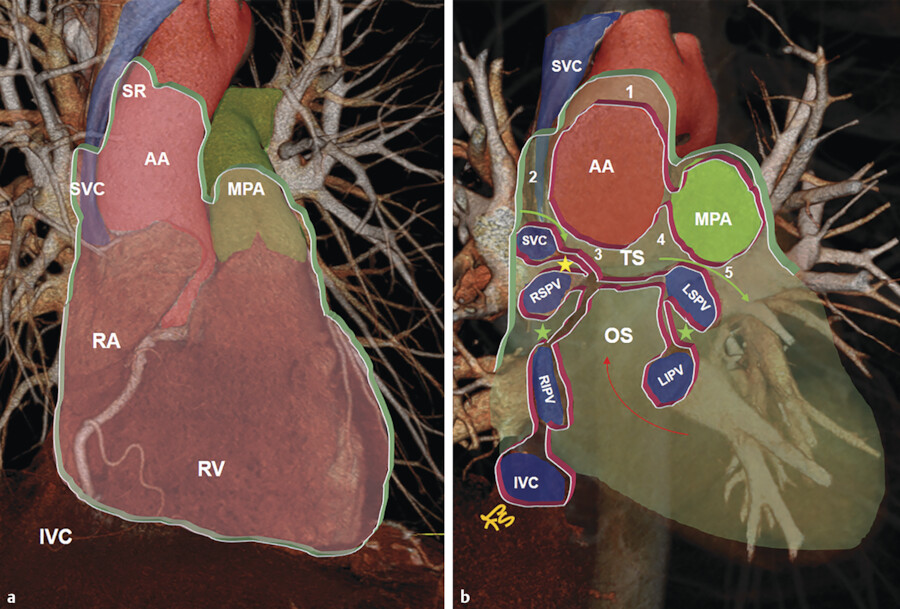
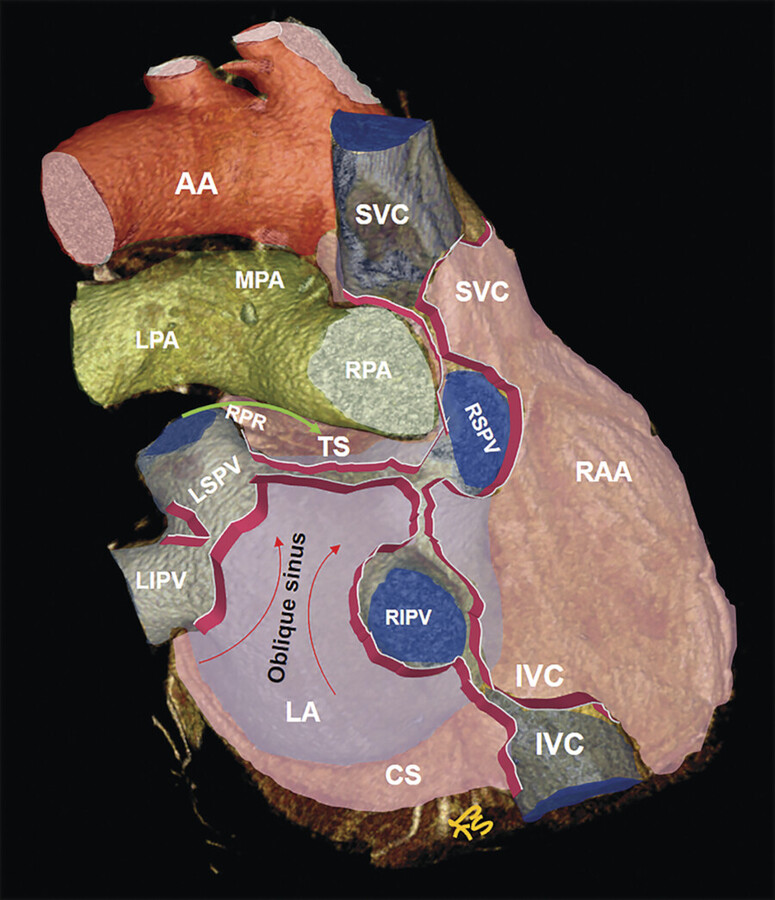
Pericardial Reflection
The reflections of the serosal layers are arranged around two complex tubes. One tube encloses the aorta and pulmonary trunk. The second tube encloses the SVC, the inferior vena cava, and the four pulmonary veins 5 , 6 (Fig. 20‑4). The length and pattern of coverage of the major vessels are variable. CT is the best imaging modality to show the extent of the pericardium over the vessels. 7 Pericardial reflection over the ascending aorta and the main pulmonary artery is at the junction of vessels originated from the truncus part of the embryonic outflow tract proximally and the rest of vessels distally which are derived from the neural crest. The SVC is covered by the pericardium over its distal part at the cavoatrial junction. The intrapericardial portion of the SVC is 2 cm laterally and 3 cm medially. 8 Pericardial reflections over the pulmonary veins are very variable 9 (Fig. 20‑8).
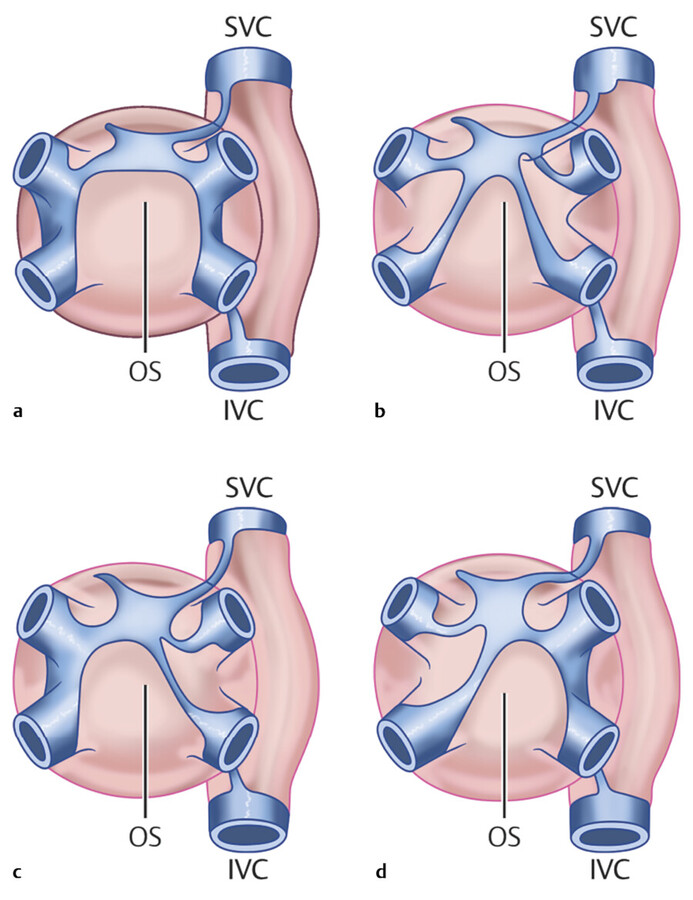
Transverse Sinus
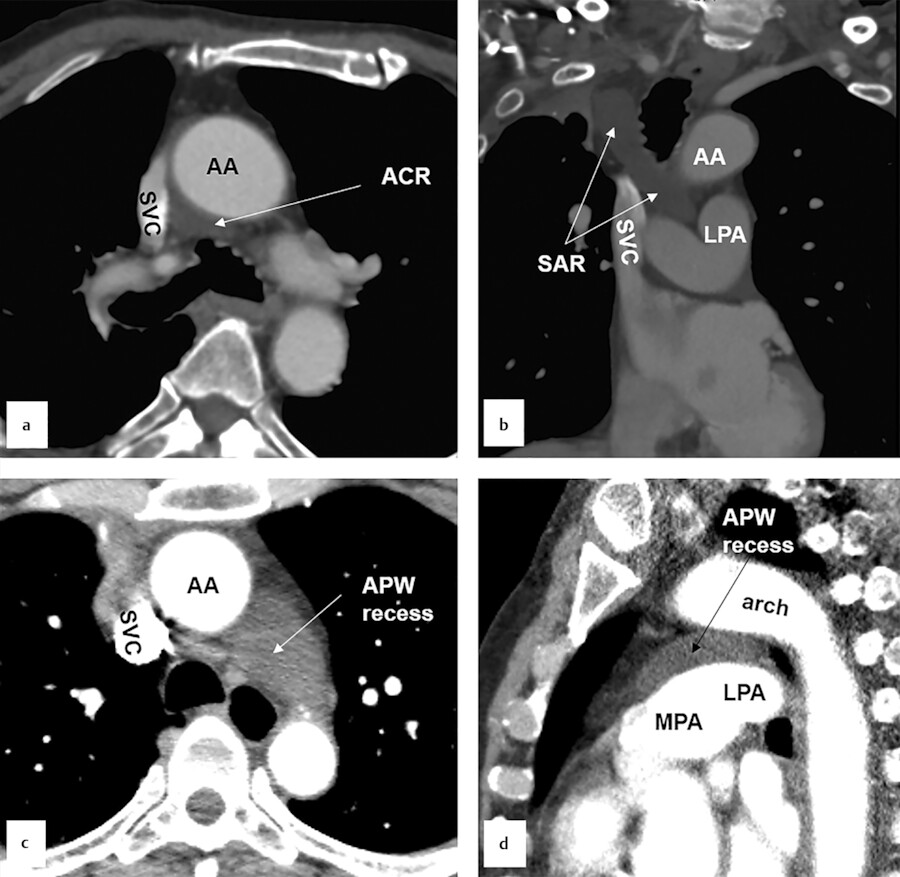
The transverse sinus is the passage between these two pericardial tubes (Fig. 20‑4 b). The transverse sinus is located inferior and posterior to the aorta and the pulmonary trunk, and above and anterior the left atrium. It is possible to pass a finger through the transverse sinus. 10 Its posteroinferior boundary is formed by a pericardial reflection extending transversely between the right and left superior pulmonary veins at their junctions with the left atrium. The right pulmonary artery exits the transverse sinus soon after its takeoff from the main pulmonary artery (Fig. 20‑5). The transverse sinus is subdivided into the superior and inferior aortic recesses and the right and left pulmonic recesses 3 , 4 , 5 , 6 (Fig. 20‑4 , Fig. 20‑9). Some authors further subdivide the aortic recess, based on its relationship to the aorta, into posterior (inferior), lateral, anterior, and superior portions (Fig. 20‑4 , Fig. 20‑9). The superior extent of the transverse sinus along the aortocaval space forms the superior aortic recess. 3 , 4 , 5 , 6 Cephalad extension of this recess into the superior right paratracheal region (high-riding recess) can be mistaken for pathologies such as a bronchogenic cyst 11 , 12 (Fig. 20‑10).
The anterior extension of the superior aortic forms a characteristic crescent in front of the aorta and main pulmonary artery (Fig. 20‑9). On the right side, the sinus is continuous with the recess around the SVC (aortocaval recess; Fig. 20‑10). Inferior extension of the transverse sinus along the posterior wall of the aorta and above the left atrium is called the inferior aortic recess. Lateral extent of the transverse sinus forms the left and right pulmonic recesses on each side between the pulmonary artery and the left atrium 13 (Fig. 20‑4 , Fig. 20‑5). The left pulmonic recess is bounded medially by the fold of ligament of Marshall (Fig. 20‑9). Of relevance to interventional electrophysiology, the inferior aortic recess allows access to the epicardial aspect of the noncoronary and left coronary aortic sinuses. 14
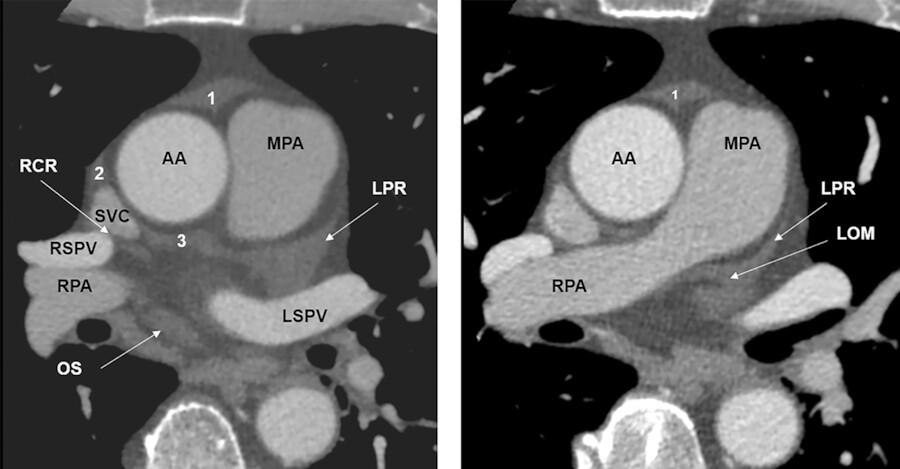
Oblique Sinus
The oblique sinus is located behind the left atrium, in the region between the four pulmonary veins and commonly contains a small amount of fluid, which makes it visible in 80 to 90% of CT scans 10 (Fig. 20‑4 , Fig. 20‑5). Posteriorly, it is bounded by the pericardial reflection on the ostial region of the pulmonary veins and the inferior vena cava where it forms small recesses. Superiorly, the oblique sinus is separated from the transverse sinus by a double reflection of serous pericardium extending between the left and right superior pulmonary veins 14 (Fig. 20‑4 , Fig. 20‑5). The size and shape of the oblique sinus is variable (Fig. 20‑8). The average width of the oblique sinus opening is 41 ± 7 mm and its depth is 31 ± 6.3 mm. 9 The depth of the pulmonary vein recesses is also variable and may be confused with pathologies such as enlarged lymph nodes (Fig. 20‑11). The left pulmonary vein recess is depicted at CT more often (60%) than the right pulmonary vein recess (30%). 10 Immediately behind the oblique sinus, the esophagus and the plexal branches of the vagus nerve pass (Fig. 20‑6). This anatomical relationship varies and its clinical relevance is related to cases admitted for radiofrequency ablation of the posterior wall of the left atrium with the potential injury of the passing esophagus and vagal nerves. The fold of Marshall is located in the left superior aspect of the sinus containing ligament or vein of Marshall, which is located between the left atrial appendage and the left superior pulmonary vein. 14 , 15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree