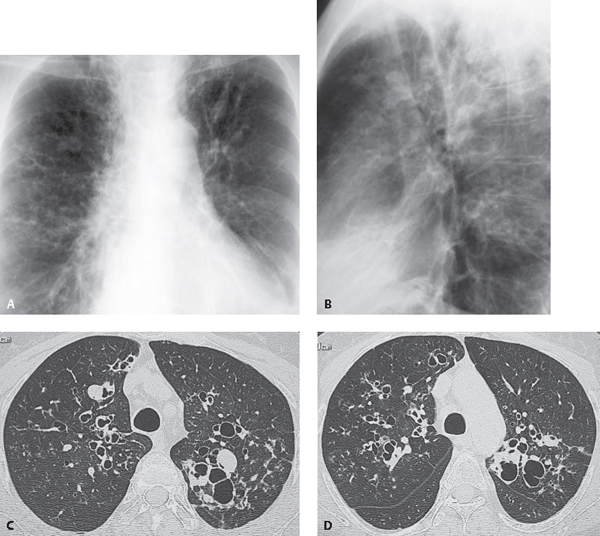
CASE 27 57-year-old woman with a long history of asthma Coned-down PA (Fig. 27.1A) and lateral (Fig. 27.1B) chest radiographs demonstrate ring-like opacities in the perihilar regions and upper lobes and a left upper lobe tubular opacity that appears to emanate from the hilum. Unenhanced chest CT (lung window) (Figs. 27.1C, 27.1D) demonstrates cystic bronchiectasis that predominantly involves the central aspects of the lungs with relative sparing of the lung periphery. Well-defined soft-tissue upper lobe nodules (Fig. 27.1C) represent mucoid impaction within dilated bronchi. Fig. 27.1 Allergic Bronchopulmonary Aspergillosis (ABPA) • Bronchiectasis of Other Etiologies Allergic bronchopulmonary aspergillosis (ABPA) is also known as allergic bronchopulmonary fungal disease, since species other than Aspergillus are sometimes implicated. Typically, Aspergillus fumigatus colonizes the airway lumen in patients with asthma. The retained bronchial secretions initiate immune complex and complement formation with resultant tissue injury. Acutely, the injury may manifest as transient subsegmental or lobar consolidation. Chronic changes damage the larger bronchi and produce central bronchiectasis, which is the imaging hallmark of ABPA. In asthmatic patients, CT detection of bronchiectasis involving three or more lobes, combined with findings of centrilobular nodules and mucoid impaction, is highly suggestive of ABPA. Affected patients typically have diffuse disease at the time of diagnosis, manifesting as central cystic and/or varicose bronchiectasis involving both lungs. ABPA is caused by type I and type III (IgE and IgG) immunologic responses to the fungal (usually Aspergillus
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
 Discussion
Discussion
Background
Etiology
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree