CASE 28 62-year-old woman with dyspnea and a 30-pack-year history of cigarette smoking Unenhanced axial chest CT (lung window) (Figs. 28.1A, 28.1B) demonstrates abnormal centrilobular areas of low attenuation with imperceptible walls. CT coronal reformation (Fig. 28.1C) shows the upper lobe distribution of disease. Proximal Acinar Emphysema (syn. Centrilobular, Centriacinar) None Fig. 28.1 Emphysema is defined as abnormal permanent enlargement of the airspaces distal to the terminal bronchiole accompanied by destruction of their walls with minimal or absent fibrosis. Emphysema is categorized according to the affected part of the pulmonary acinus. Proximal acinar (syn. centrilobular, centriacinar) emphysema involves the proximal aspect of the acinus with distension and destruction that primarily affects the respiratory bronchioles (Fig. 28.2). Proximal acinar (centrilobular) emphysema occurs primarily in cigarette smokers and is related to an imbalance between elastolytic and anti-elastolytic processes in the lung. Cigarette smoke impairs α-1-antiprotease’s inhibitory function, resulting in increased elastolytic activity with subsequent loss of the connective tissue attachments of the terminal bronchiole and damage to the lung’s elastic framework. These changes are responsible for terminal bronchiolar collapse and resultant airflow obstruction. Patients with proximal acinar (centrilobular) emphysema are typically adults between the ages of 55 and 75 years. They present with dyspnea and less commonly with cough. These patients may be thin and appear to be in respiratory distress. They exhibit prolonged expiration, breathe with pursed lips, and may sit leaning forward. Pulmonary function tests are characterized by increased total lung capacity (TLC) and residual volume (RV) and decreased diffusing capacity. • Increased lung volumes or lung height (measured ≥30 cm from right first rib tubercle to diaphragm dome) • Diaphragmatic flattening (highest level of diaphragmatic contour is <1.5 cm above a line connecting the costophrenic and vertebrophrenic junctions on PA view or a line connecting the sternophrenic and posterior costophrenic angles on lateral view) • Enlarged retrosternal clear space (horizontal distance between sternum and anterior margin ascending aorta >2.5 cm on lateral view) • Abnormal lucency in the upper lung zones
 Clinical Presentation
Clinical Presentation
 Radiologic Findings
Radiologic Findings
 Diagnosis
Diagnosis
 Differential Diagnosis
Differential Diagnosis
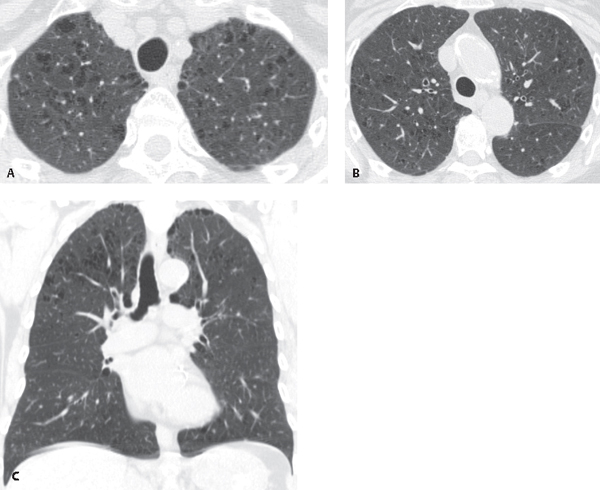
 Discussion
Discussion
Background
Etiology
Clinical Findings
Imaging Features
Radiography
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree