Vasantha Kumar Venugopal 3D printing is already shaking our age-old notions of what can and can’t be made. Hod Lipson 3D printing, better known in industrial parlance as additive manufacturing (AM), is a technology that has been in vogue for about 30 years now. Only recently has its use in healthcare and allied sciences increased manifold largely due to the expiry of patents of different technologies, which in turn cleared the way for arrival of a wide array of low-cost high-quality 3D printers. 3D printing or AM (as opposed to the traditional subtractive manufacturing) refers to a set of processes in which a three-dimensional object is a built object by adding material layer by layer, while subtractive manufacturing removes material to create parts. The materials that are used commonly include resins, thermoplastics (such as ABS, PLA) and metals. On the basis of the type of material used and the technique by which they are fused, different techniques have been defined. To put it in simple terms, 3D printing techniques can be used to recreate body parts and disease processes or pathological conditions into a physical 3D model using a range of materials from as simple as ABS plastic and resins to as complex as nylon or titanium. For example, an invasive tumour in brain or liver can be recreated in to a life-size three-dimensional model that shows the exact size, site and morphology of the tumour along with its extension in to blood vessels and other organs. There are five broad ways in which 3D printing can play a decisive role in healthcare. They are as follows: As the last two applications are out of the scope of a radiologist, we will discuss about the first three applications in this chapter. The starting point of any 3D printing service or application is the radiology department. Three-dimensional models are created using imaging data from the patient’s scan. It could be a CT scan, MRI scan or even ultrasound images depending upon the disease condition under question. For making a 3D model from such images, the data from the images needs conversion into some format, the existing 3D printers understand, usually an STL file. This conversion also includes a step called slicing during which the diseased anatomical structure or body part is separated from other normal body parts. These processes are in the exclusive domain of radiologists since they are best equipped to read the scan images and determine which body parts can be printed with utmost detail. Once such a file is created, the rest of the printing process can be smoothly overseen by a biomedical or a mechanical engineer. The process of 3D printing involves multidisciplinary team including radiologists, surgeons and engineers. The different steps in the process are as follows: This is the first and critical step in the 3D printing. The most common imaging methods useful for 3D printing are CT and MRI. In general, 3D models can be printed from any volumetric image data set with sufficient contrast to differentiate tissues. Acquisition of images using the appropriate protocol and slice thickness is the most important process. These parameters vary depending upon the anatomy that is to be printed. For optimal quality of the final print, slice thickness of CT scans should preferably be less than 1.25 mm. While thicker slices might reduce the accuracy of the model, very thin sections might consume more time for segmentation. The other parameters that need to be factored in while acquiring scans for creating a 3D printing workflow include intravenous contrast administration, the timing of the scan after contrast administration and reconstruction kernels. Artefacts in the images due to movements or metallic implants are an important consideration for 3D printing. Adequate artefact correction measures are needed for better segmentation. Segmentation is the process by which the anatomy of interest that needs to be printed is separated from the rest of the structures in the scan. For example, to make a 3D-printed model of a renal mass invading into the renal vein, the tumour, kidney and the invaded vein should be segmented or separated from other structures in the abdominal scan. This process can be of varying complexity. Depending upon the complexity of the task, it can be performed by semiautomated methods (thresholding, edge detection, etc.) or supervised manual methods by radiology technologist or a radiologist. There are several open-source and commercial software that are available to perform this segmentation task. Some of the commonly used segmentation software are listed in Table 1.27.1.
1.27: 3D printing and postprocessing
3D printing – basics
What is 3D printing?
Role of 3D printing in healthcare
Radiology – pivot of 3D printing
3D printing workflow
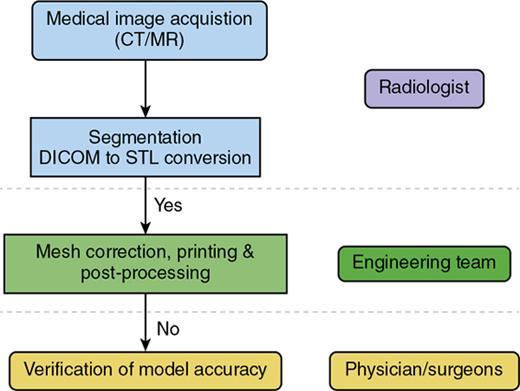
Image acquisition and segmentation
Open Source Segmentation Software
Commercial Segmentation Software
3D slicer
Materialise Mimics
ITK Snap
Amira
ImageJ
Label box
Anatomage Medical Design studio
Osirix
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree