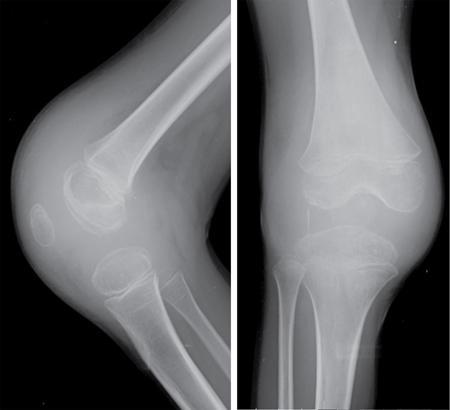
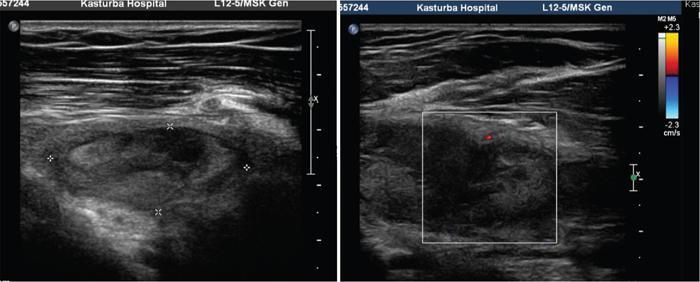
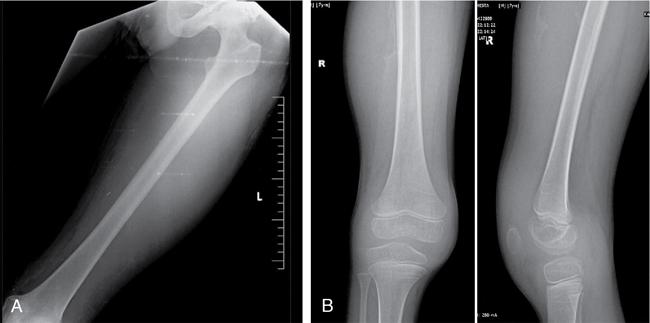
Prakashini Koteshwar Haemophilia is an X-linked recessive disorder of clotting mechanism. There are three forms: namely Haemophilia A, B and C. Haemophilia A is caused by factor VIII deficiency. Haemophilia B is caused by a deficiency of factor IX and Haemophilia C is due to a lack of clotting factor XI. Haemophilia A is 4 times commoner than B form. Occurrence rate is 1 in 5,000 live male births. The worldwide incidence is more than 400,000 people. Most women are only carriers and inheritance is always from mother to son as defective gene is located on X chromosome. Pathophysiology: factors VIII and IX are intrinsic clotting factors. Factor VIIII is a critical factor which accelerates the function of factor IX. Thus, deficiency of these factors by 75% causes bleeding in human beings. Deficiency is either due to genetic, acquired or structural defects in the factor protein. Haemophilia can be of mild, moderate or severe in degree depending on amount of these activation factors, which varies from <1% of normal clotting activity in severe grade haemophilia, 1%–4% in moderate grade and 5%–25% in milder grade. Factor VIII is a protein produced by the liver, activates factor X helps in producing thrombin and prothrombin without which fibrin, a component required in stability of clot will not be formed. Factor VIII inhibitor can develop as many as 30%–40% of patients with severe haemophilia A, less than 1% of functional factor VIII. As an immune response to treatment with factor VIII replacement, factor VIII inhibitors IgG antibodies are produced. Such inhibitors inactivate and hinder coagulation by attaching to the factor VIII proteins. Clinical features: it varies from mild to severe grade depending on amount of factor VIII deficiency. Milder form will show bleeding only during surgery or unexplained excessive bleeding from small cuts. Sometime blood in urine and stool, bruises, nose bleed and swelling and pain in joints due to the bleeding may be the presentation. Incidence of common sites of bleeding are, haemarthrosis in 70%–80%, followed by muscle or soft tissue bleeding in 10%–20% and bleeding into central nervous system or gastrointestinal wall in < 5%. Among the joints most commonly knee (45%) and elbow (30%) involved followed by ankle and shoulder joint. Minor bleeding conditions like haematuria, gum bleed, tooth extraction bleed and sublingual haematoma are commonest early presentation. Bleeding into the joint called as haemarthrosis is a most common manifestation. Initial stage of haemarthrosis produces mild tightening of joint, followed by swelling and pain. Distension of joint due to blood causes synovial proliferation leading to release of cytokines. By the middle age the joint deformity manifests due to destruction of joint. Imaging: Usual and unusual imaging manifestations of different organ systems are discussed here after. Haemarthrosis and haemophilic arthropathy: recurrent bleeding into the joints most commonly knee and elbow induces chemical reaction due to the release of cytokines and kinin by the blood products. This chemical reaction causes proliferation of synovium and damage to the cartilage resulting in pannus formation and subchondral erosion. Recurrent bleeding induces inflammation and hyperemia leading to epiphyseal excessive growth and juxta articular osteoporosis. Radiograph of knee joint shows widening of intercondylar notch, squaring of the patella, joint space narrowing, subchondral cysts, osteoporosis and accelerated degenerative changes. The displacement of certain structures in and around the joint is seen in case of acute joint bleeding. Anterior displacement of patella and quadriceps tendon, fullness of suprapatellar recess which will be of relatively higher density because of blood when compared to simple effusion (Fig. 2.5.1). Similarly, in elbow haemarthrosis shows, elevation of anterior and posterior fat pad (Fig. 2.5.2) and in case of shoulder haemarthrosis there will be inferior displacement of humerus (Fig. 2.5.3). Recurrent episodes of bleeding into the joint causes arthropathy changes by middle age (Fig. 2.5.4A and B). Haemophilic arthropathy can be graded by two scales. First one is Arnold–Hilgartner scale which is prognostic scale and Patterson scale is an additive scale with a score of 13 maximum for a joint indicates severely affected. Arnold scale consists of stage 0–5, healthy joint 0, normal radiography is 1, osteoporosis and soft tissue swelling 2, epiphyseal enlargement with disorganization of joint in stage 3, cartilage injury stage 4 and osteoarthritic changes in 5, similar to rheumatoid or degenerative arthritis. In Patterson scale, each joint is scored as 0, 1 and 2 based on absent, mild, pronounced features of osteoporosis, narrowing of joint space, cortical irregularity, erosion, subchondral cyst, disorganization and destruction. Total score is 78, more than 13 indicates severely involved joint. Ultrasound: joint effusion with internal echoes indicates haemarthrosis. Synovial hypertrophy, cortical irregularity and soft tissue collection can be well assessed with high frequency probe. Since ultrasound is a non-invasive and time saving modality, can be used as prognostic tool. Haematoma in soft tissue can appear heterogenous to anechoic to hypoechoic depending on stage of haematoma (Fig. 2.5.5). MRI: The stage of haemarthrosis, T1 image will show hyperintense joint fluid, with blooming on gradient sequence. Due to the recurrent bleed, haemosiderin deposition takes place which appears as hypointense signal on T2W imaging. Early stage of synovial hypertrophy is better seen on post-contrast T1 fat sat sequence as enhancing synovium lining the joint effusion. Associated arthropathy changes, cartilage injury and subchondral disease can be well assessed on proton density sequence. Earliest changes in synovium of joint before the clinical symptoms can be detected by MRI, thus it is a sensitive tool. Haemosiderin may be deposited along with the intra-articular ligaments and tendons. MRI is also useful in monitoring the progress of arthropathy. Osteopenia of bones due to disuse because of recurrent joint arthrosis can present with fractures. MRI is useful in monitoring response to the prophylactic treatment in patients with early stage of the disease and also, it can help in the selection of patients with more advanced disease for synovectomy, by surgical, chemical or radioisotope method. Differential diagnosis of haemophilic arthropathy includes juvenile rheumatoid arthritis, gout, synovial osteochondromatosis, pigmented villonodular synovitis and amyloid arthropathy. Pseudotumour is a known entity since 1918, uncommon complication of severe form of haemophilia in a frequency of 1%–2%. It is a condition where there is recurrent bleeding into the muscle, tendon insertion region, within the bone or subperiosteal region leading to encapsulation. It is a slowly expanding painless swelling usually follows trauma, commonly seen in femur, pelvis and tibia. Soft tissue pseudotumour can erode or sometime cause significant destruction of adjacent bone. Soft tissue calcification will be seen as a sequel. Chronicity of pseudotumour incites reactionary subperiosteal reaction and sometimes subperiosteal bleed itself cause significant elevation of periosteum, giving curvilinear calcification or strut that parallels the bone and projects into soft tissue, close mimic of Ewing or infection (Fig. 2.5.6A and B). As the pseudotumour enlarges there will be compartment syndrome leading to necrosis of muscle and skin. Secondary compression of nerves will cause pain. Other complications are pathological fracture, infection and fistula formation. Osseous pseudotumour can be seen as lytic lesion, unilocular of multilocular in meta or epiphysis with sclerotic margin or completely destructive lesion. Usually trabeculae are maintained within the lytic area. Dystrophic or sequestrational calcification or ossification can be seen within (Fig. 2.5.7A and B). Differentials are any lytic benign or malignant bone tumuors like cyst, GCT, plasmacytoma, telangiectatic osteosarcoma or metastasis.
2.5: Bleeding diathesis
Bleeding diathesis
Haemophilia



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








