Fig. 7.1
Multiple two-dimensional (2D) ultrasound images produced by sweeping a conventional one-dimensional (1D) ultrasound transducer over an anatomic structure of interest. The 2D images can be reformatted to display images in three dimensions (3D)

Fig. 7.2
Ultrasound transducer with a two-dimensional (2D) array remains stationary while electronically sweeping the ultrasound beam over an anatomic structure of interest. The three-dimensional (3D) images are generated in real time
Once the data acquisition has been completed, images can then be displayed in either B-mode (gray scale) or Doppler using a variety of display techniques. The most common display techniques are (1) multiplanar reformatting, (2) volume rendering, and (3) surface rendering [14, 15]. Multiplanar reformatting is the most common display technique and displays planar cross-sectional images that resemble conventional 2D ultrasound images but are extracted from the 3D image (Fig. 7.3). The 2D planes are shown with 3D cues. The orthogonal plane view displays three perpendicular planes simultaneously, and the cube view shows the 3D image as a polyhedron which represents the boundaries of the reconstructed volume [14]. Each plane can be manipulated relative to any of the other planes. The polyhedron in the cube-view display technique can be rotated in any direction. The volume rendering display technique shows the entire 3D image projected onto a 2D plane. The surface rendering display technique only displays an image of the surfaces of structures. Some of these display techniques can also be combined.


Fig. 7.3
Multiplanar reconstruction 3D images of the thyroid in the coronal plane are show anteriorly at the level of the isthmus and thyroid cartilage (arrows) in (a) and more posteriorly in (b). Several small cystic nodules are noted (arrows) in (b)
3D ultrasound has advantages and disadvantages compared with 2D ultrasound (Table 7.1) [15]. Advantages of 3D ultrasound include that it stores all data continuously, it allows for a more rapid examination/faster data acquisition because it is not necessary for the ultrasonographer to select single images to save, and data can be manipulated to display images in any plane or produce 3D reconstructions, which allows for the assessment of exact spatial relationships. 3D ultrasound with Doppler can also allow for a more accurate assessment of the vascularity of a structure, as it can evaluate the vessels during a 360° rotation of the volume rather than rely on the ultrasonographer’s choice of the plane for the evaluation of vascularity. The main disadvantage of 3D ultrasound compared with 2D ultrasound is that 3D ultrasound may have inferior image quality because of the lower resolution of the extracted planes from volume data [16]. In addition, 3D ultrasound images require large data sets and computational requirements to process and display the data and may be subject to motion and reconstruction artifacts.
Table 7.1
Comparisons between two-dimensional (2D) and three-dimensional (3D) ultrasound
2D ultrasound | 3D ultrasound |
|---|---|
Superior image quality | Inferior image quality because of the lower resolution of the extracted planes from volume data |
Images not subject to motion artifact | Images may be subject to motion and reconstruction artifact |
Smaller data set | Larger data set |
Stores only images that the ultrasonographer selects | Stores all data continuously |
Slower data acquisition | Faster data acquisition |
Some views impossible to achieve because of restrictions related to patient anatomy or position | Data can be manipulated to display images in any viewing plane |
Comparisons of structures over time dependent on images selected to be saved | Permits comparisons of full data sets over time which may lead to more accurate follow-up |
There is interobserver variability in the evaluation of thyroid echogenicity, borders, and volume | There is better interobserver reproducibility in the evaluation of thyroid echogenicity, borders, and volume |
Thyroid volume calculations are operator dependent: the ultrasonographer must find the perfect angle and location of the transducer to measure three perpendicular axes | Thyroid volume calculations are not operator dependent |
Thyroid volume calculations are an estimate based on a regular geometric shape (i.e., each thyroid lobe is assumed to be an ellipsoid) | Thyroid volume calculations are more exact (sum of cross-sectional areas of each 2D image multiplied by the interslice distance) |
Applications of 3D ultrasound technology in the evaluation of thyroid disease can broadly be divided into three categories: risk assessment of thyroid nodules for malignancy, preoperative assessment of extrathyroidal extension of thyroid cancers, and thyroid volume calculations for radioactive iodine administration.
7.3 Risk Assessment of Thyroid Nodules for Malignancy
Thyroid nodules are common in the general population, especially in women. The risk of malignancy in a thyroid nodule is 7–15 %, and the most accurate and cost-effective way to distinguish between a benign and a malignant thyroid nodule is fine-needle aspiration (FNA) biopsy [1]. Nodules are selected for FNA biopsy based on their size and appearance on 2D ultrasound. The American Thyroid Association (ATA) recommends FNA biopsy of nodules ≥1 cm with intermediate or high suspicion for malignancy based on sonographic pattern (hypoechoic, irregular margins, microcalcifications, evidence of extrathyroidal extension , taller-than-wide shape) and of nodules ≥1.5 cm with low suspicion for malignancy based on sonographic pattern (isoechoic, hyperechoic, partially cystic with eccentric solid areas) [1]. Nodules ≥2 cm that are spongiform or partially cystic without any suspicious features may be biopsied or observed [1].
While most thyroid nodules are benign, 2–25 % of FNA biopsy results are in an indeterminate category (atypia/follicular lesion of undetermined significance, follicular neoplasm/suspicious for follicular neoplasm , suspicious for malignancy) [1]. Although most nodules that have indeterminate cytology will ultimately prove to be benign [17, 18], many patients are referred for surgery for definitive diagnosis. Therefore, any technique that can either diminish the concern for malignancy and avoid FNA biopsy, or be applied after an indeterminate cytology result may help to reduce the need for thyroidectomy for definitive diagnosis of a benign thyroid nodule .
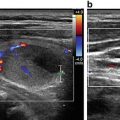
3D ultrasound may be able to refine the selection of thyroid nodules for FNA biopsy by more clearly demonstrating nodule characteristics such as overall shape, margins, and vascular patterns compared with static 2D imaging (Fig. 7.4). In a study of 71 nodules, 16 of which were malignant, evaluated with 3D ultrasound with power Doppler, Slapa and colleagues found the following features associated with malignancy: ill-defined border in multiplanar reformation mode, lobulated shape of the nodule in the c-plane (the plane parallel to the ultrasound probe), and the density of central vascularization within the lowest or highest ranges [19]. The combination of these three features was demonstrated to have a sensitivity of 100 % and a specificity of 60–69 % for the assessment of malignancy, and the application of these criteria for selection of nodules to undergo FNA biopsy would have decreased the number of biopsies from 71 to 38 without missing a malignant nodule [19]. Similarly, Li and colleagues found that irregular shape of a thyroid nodule on 3D ultrasound had high sensitivity (91 %) and specificity (88 %) in identifying malignant thyroid nodules in a study of 103 nodules , 53 of which were malignant [20]. In three cases (one benign and two malignant), the shape of the thyroid nodule was deemed to be regular on 2D but irregular on 3D ultrasound [20].


Fig. 7.4
Sagittal surface-rendered reconstructed 3D image shows a lobulated border along the superior border of the nodule (arrow)
The evaluation of thyroid nodule vascularity by 3D ultrasound may also be useful in the evaluation of a thyroid nodule for malignancy within certain subtypes of nodules. Molinari and colleagues studied 20 nodules with features of malignancy on 2D ultrasound (hypoechogenicity, microcalcification, irregular margins), 15 of which were follicular neoplasms and 10 of which were malignant [21]. 3D ultrasound with an IV contrast agent demonstrated that the malignant nodules had statistically higher vascular density, number of vascular trees, number of branching nodes, and vascular tortuosity than benign nodules [21]. While the assessment of vascular density of thyroid nodules would probably not change the indication for FNA biopsy , it may increase or decrease the risk of malignancy in a follicular neoplasm, and thus has the potential to influence the choice of operation (diagnostic thyroid lobectomy vs total thyroidectomy).
7.4 Preoperative Assessment of Extrathyroidal Extension of Thyroid Cancers
The most common type of thyroid cancer is papillary thyroid cancer (PTC ), comprising approximately 85 % of cases of differentiated thyroid cancer [1]. The treatment of PTCs by the majority of surgeons in the United States is total or near-total thyroidectomy with appropriate lymph node dissection [22]. However, large studies have not shown a difference in outcomes between total or near-total thyroidectomy and thyroid lobectomy for PTCs <1.0 cm, and thus thyroid lobectomy is an acceptable treatment for PTCs <1.0 cm without extrathyroidal extension [23, 24]. Previous studies have shown that extrathyroidal extension is an independent risk factor for cancer recurrence [25] and upstages the T stage from T1 to T3. Therefore, the preoperative identification of extrathyroidal extension may change the extent of thyroidectomy for PTCs <1.0 cm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree