40 Infectious Arthritis
Acute forms of arthritis occur as immunological reactions after infections or through hematogenous spread or direct infection of the joint, usually with bacterial, less commonly with tuberculous, viral, or parasitic pathogens. Diagnostic imaging of the hand is discussed synoptically for etiologically and pathophysiologically different articular infections along with their clinical and laboratory findings.
Pathoanatomy and Clinical Symptoms
Infectious arthritis usually involves monoarticular inflammation caused directly by pathogens with cartilaginous and bony destruction and can lead to fibrous or osseous ankylosis. Staphylococci are the most common pathogens in 70%. Streptococci and Haemophilus influenzae are found in children, Neisseria gonorrhoeae in young women, and Gram-negative rods especially in patients with an immune deficiency. In principle, reactive arthritis, which breaks out after a latency period following an infectious disease, must be differentiated from infectious forms of arthritis. The following pathogens have been identified in the synovium or joint fluid recently: Chlamydia, Borrelia burgdorferi (Lyme disease), Mycobacterium leprae, Schistosoma haematobium (bilharziosis), and various viruses, especially hepatitis B and rubella. The discussion of whether infectious arthritis occurs in parallel with or complementary to an immunological pathogenesis is ongoing.
Pathways of Infection
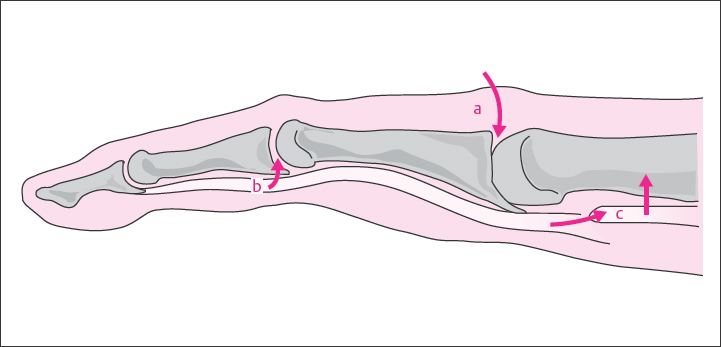
Organisms can enter a joint in different ways ( Fig. 40.1 ):
Hematogenous spread of pathogens: The organisms reach the synovial membrane directly via the circulation or indirectly from an epiphyseal or periarticular focivia connecting vessels. Metastatic spread is especially common in the carpal joints.
Spread of infection through tissues: The inflammation spreads from soft tissues either through the joint capsule or along the tendon sheaths into the joint cavity so that the articular access can be relatively far from the arthritic focus. An osteomyelitic infection can penetrate into the joint via the destroyed articular cartilage.
Direct implantation: The infection arises after surgical opening of the joint or an injury that has penetrated the joint.
Diagnostic Imaging
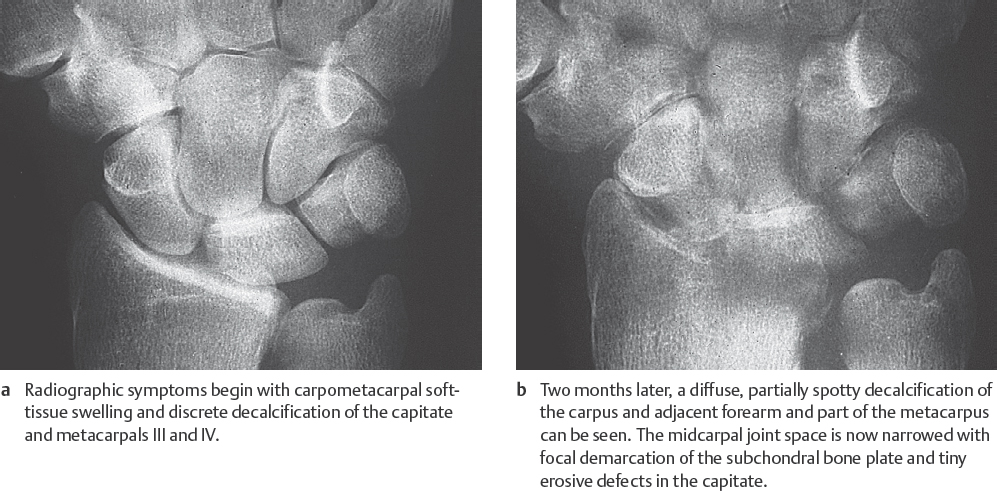
Radiography
The stages of so-called soft-tissue signs, collateral signs (periarticular osteopenia), and direct signs of arthritis progress in acute, pyogenic arthritis in days to weeks ( Fig. 40.2 ) and in a tuberculous articular infection in months to years. Without treatment, severe destruction and ankylosis develop.
Nuclear Medicine
Three-phase skeletal scintigraphy with 99mTc phosphonates provides early detection of local hyperemia by radionuclide perfusion (phases I and II) and can differentiate to a certain extent between arthritis and osteomyelitis in phase III. Scintigraphy is useful in localizing the primary source of the infection, but differentiation between sterile and infectious arthritis is not possible.
Inflammatory scintigraphy with 99mTc-HMPAO-labeled autologous leukocytes and Tc-nanocolloid, as well as
Immunoscintigraphy with 99mTc-labeled murine monoclonal granulocytes or human unspecific immunoglobulin, selectively demonstrates acute granulocyte-induced inflammations. Aseptic or chronic forms of arthritis, such as tuberculous or leprous arthritis, generally cannot be located with either of these two procedures.
Ultrasonography
Large joint effusions, articular and periarticular soft-tissue swelling (see Fig. 42.2 ), and concomitant soft-tissue abscesses can be identified with high-resolution ultrasonography (US).
Arthrography
When a diagnostic joint puncture is performed to obtain pathogens, arthrography can also be performed to demonstrate defects in the articular cartilage or capsule.
Computed Tomography
CT scans can demonstrate not only osseous erosions in the joint, but also inflammatory soft-tissue thickening, but it is less sensitive than MRI. In infectious inflammations, CT is indicated to locate foreign bodies, as well as intraosseous and intra-articular air when radiographs prove unremarkable. Aside from US, CT can be useful in controlling the puncture of joints and abscesses.
Magnetic Resonance Imaging
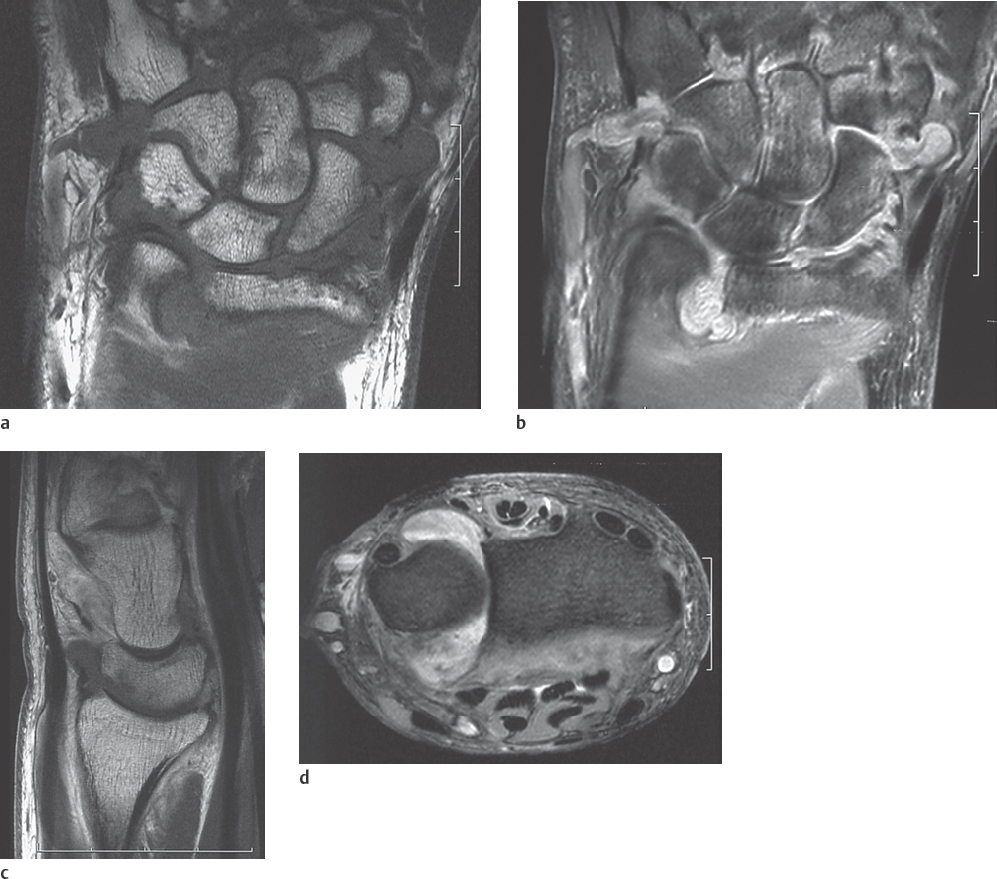
As described in the chapters on noninfectious forms of arthritis (Chapters 34–39), MRI is the imaging procedure of choice for confirmation and staging of the spread of synovial joint diseases. Joint effusions, as well as the almost always concomitant bone-marrow and soft-tissue edemas, appear hyperintense in T2-weighted sequences (PD- or T2-weighted FSE, both fat-saturated, STIR/SPIR FSE). Cartilaginous defects caused by arthritis can be visualized directly with a T2*-weighted GRE or a fat-saturated PD-weighted FSE sequence (Fig. 40.3d). The inflamed soft tissues (synovium, joint capsules, ligaments, tendon sheaths) can be visualized in several (oblique) imaging planes. They usually show increased enhancement of intravenously administered gadolinium in T1-weighted SE sequences with fat suppression (Fig. 40.3a, b). Concomitant osteomyelitis generally cannot be differentiated. MRI results mostly do not provide information on the etiology of the arthritic disease.
Disease Entities
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree