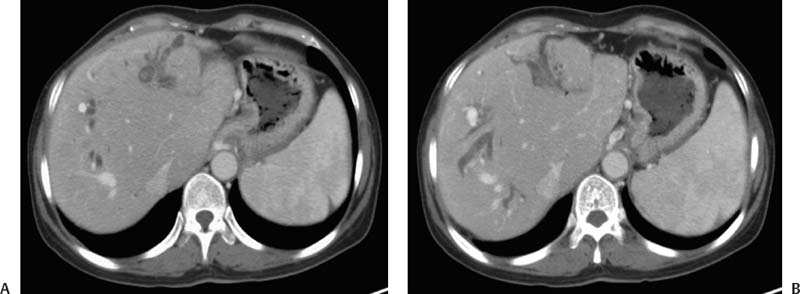
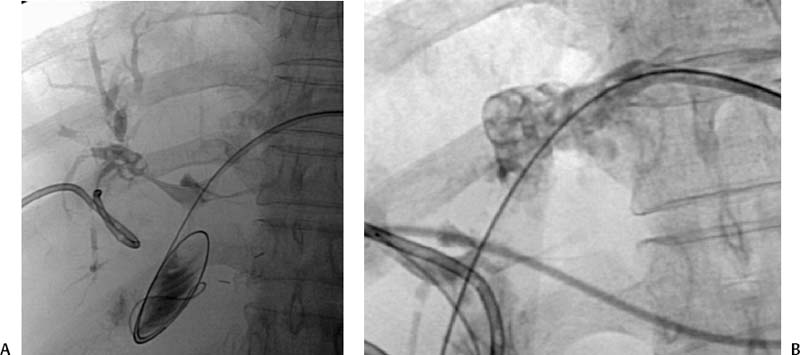
CASE 41 A 35-year-old immigrant from Malaysia with a history of prior abdominal surgery for biliary obstruction presented to the emergency department with fever, abdominal pain, and jaundice. She was hypotensive at 90/45 mm Hg. Liver function tests were markedly elevated in a pattern consistent with biliary obstruction. Figure 41-1 A 35-year-old immigrant from Malaysia with a history of prior abdominal surgery for biliary obstruction presented with abdominal pain, jaundice, and sepsis. (A) Contrast-enhanced axial CT shows bilobar intrahepatic bile duct dilatation, worse on the left. Predominantly noncalcified intraluminal stones are present in the left lobe. (B) Additional image shows patchy intrahepatic duct dilatation in the right lobe and marked dilatation in the left lobe. Abdominal CT showed asymmetric intrahepatic bile duct dilatation, worse in the left lobe compared with the right. Multiple intraductal stones were present, the vast majority of which were noncalcified (Fig. 41-1). Oriental cholangiohepatitis (recurrent pyogenic cholangitis). Endoscopic retrograde cholangiopancreatography (ERCP) failed to facilitate biliary decompression. The gastroenterologist encountered a Roux-en-Y choledochojejunostomy and had difficulty crossing the biliary-enteric anastomosis. The patient was referred to interventional radiology and underwent bilateral percutaneous transhepatic cholangiography (PTC). Marked intrahepatic ductal dilatation was verified, left greater than right. The main left intrahepatic duct was completely obstructed. Injection of the right intrahepatic biliary system from the left approach showed multiple intraluminal stones and patchy segmental duct dilatation (Fig. 41-2). Bilateral internal-external biliary drains were placed. During subsequent procedures, the stones were broken up with a radial jaw device and a trilooped snare (Fig. 41-3) and pushed into the enteric loop with a balloon. Accustick set (Boston Scientific, Natick, Massachusetts) Standard 0.035” guidewire (Boston Scientific, Natick, Massachusetts) 7 and 9F dilators (Cook, Bloomington, Indiana) 8F standard biliary drain (Boston Scientific, Natick, Massachusetts) Contrast material
Clinical Presentation
Radiologic Studies
Diagnosis
Treatment
Equipment for PTC
Discussion
Background
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree