Axial enhanced T1WI centered in the internal auditory canal.
Axial enhanced T1WI centered on both frontal and parietal convexities.
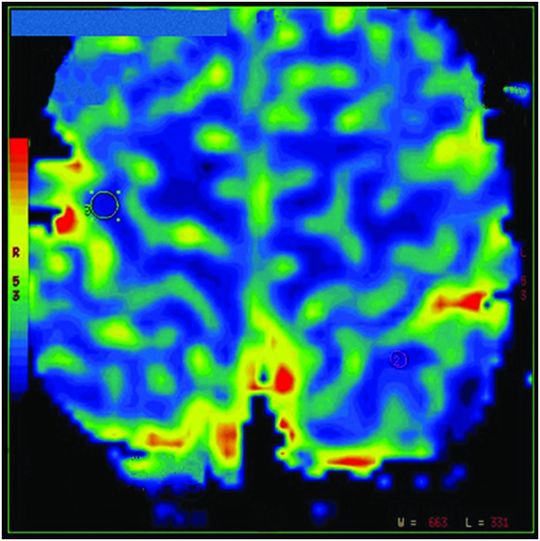
Axial perfusion-weighted image.
Chagas Disease
Primary Diagnosis
Chagas disease
Differential Diagnoses
Toxoplasmosis
Pyogenic abscess
Tuberculosis
Neurosarcoidosis
Brain metastasis
Imaging Findings
Fig. 46.1: Axial enhanced T1WI of the posterior fossa (centered in the internal auditory canal) demonstrated abnormal contrast enhancement in the fundus of the internal auditory canal, which extends to the geniculate ganglion (circle) with no significant changes in the adjacent temporal bone noted. Fig. 46.2: Axial T2-FLAIR image at the level of the convexity showed bilateral parietal and right frontal subcortical hyperintensities with mild mass effect in keeping with vasogenic edema (arrows). Note the three ill-defined, hypointense nodules in the subcortical white matter, one on the right side and two on the left side. Fig. 46.3: Axial enhanced T1WI centered on both frontal and parietal convexities, showed enhancement in the previously shown hypointense nodules (Fig. 46.2). On the right side, the nodules showed solid enhancement (arrows) and on the left the lesions showed ring enhancement (circle). Fig. 46.4: Axial DWI showed faint, hyperintense foci (arrows), which match the enhancing foci observed (Fig. 46.3). Fig. 46.5: Axial perfusion-weighted image showed that the enhancing lesions are cold and do not demonstrate increased perfusion.
Discussion
The findings of bilateral subcortical enhancing nodules with vasogenic edema accompanied by abnormal enhancement in the subarachnoid space (fundus of the internal auditory canal and of the facial nerve) are not specific for Chagas disease (CD). This association can be seen in various pathologies such as inflammatory processes, infectious diseases, and in cases of brain metastasis with meningeal carcinomatosis. However, two important details in this patient’s presentation are suggestive of CD. First, her origin is Brazil – an endemic region, and second, she has a previous history of heart transplantation.
In this patient, CD was presumably reactivated. Reactivation usually occurs secondary to immunosuppressive treatment, particularly after heart or liver transplantation. Reactivation of CD also occurs secondary to immunodeficiency diseases, especially AIDS. Although immunosuppressive therapy prevents rejection and graft-versus-host disease, it also increases the risk of CNS infection, which occurs in 5–10% of patients (brain abscess, encephalitis, or meningitis). Aspergillus, listeria, and cryptococcus are the most common causes of post-transplantation infection. Bacteria and opportunistic pathogens are more common in the first month after transplantation. Infections due to herpes viruses (cytomegalovirus or Epstein-Barr virus), fungi, atypical bacteria, or parasitic infestation develop most often five months post-transplant, with Toxoplasma gondii being the most common infectious organism. Six months after immunosuppression therapy is reduced, CNS infection becomes less common.
The association of enhancing lesions in the brain parenchyma and in the subarachnoid space may be found in infectious diseases such as in viral meningoencephalitis, pyogenic meningitis with cerebritis (with or without abscess formation), toxoplasmosis, and other opportunistic infections, tuberculosis, and fungal diseases. This pattern can be seen in some inflammatory diseases such as in neurosarcoidosis. Lymphoproliferative disorders and intracranial metastasis with meningeal carcinomatosis and brain parenchymal infiltration can also display this pattern.
In cases of tuberculous meningitis, the involvement of the subarachnoid space tends to be more important and evident in the basal cisterns (basilar meningitis). Intra-axial tuberculomas can occur isolated or associated with tuberculous meningitis and usually show ring of enhancement. Toxoplasmosis meningitis can manifest meningeal enhancement and typical parenchymal toxoplasmosis lesions show ring of enhancement with eccentric enhancing nodules (eccentric target sign). In cases of neurosarcoid, the extra-axial lesions tend to involve the subarachnoid spaces and the adjacent dura. The intra-axial lesions of neurosarcoidosis can have variable location such as the brain parenchyma itself, pituitary stalk, cranial nerves, and periventricular white matter typically with contrast enhancement. These lesions can be punctate, nodular, and mass-like.
Chagas disease is caused by Trypanosoma cruzi, a flagellated protozoan that affects an estimated 8–10 million people worldwide. Chagas disease is endemic in most South and Central American countries, affecting mostly people in low socioeconomic or rural regions. With the increase in urbanization and emigration, CD can be found in the United States and other parts of the world.
Classically the disease is transmitted by the bite of triatomine bugs. Other routes of transmission include transfusion of contaminated blood with T. cruzi, oral transmission (ingestion of fluids or food contaminated with triatomine feces containing T. cruzi), and vertical or congenital transmission (crossing the placenta). Other less common modes of transmission include transplantation of diseased organs, ingestion of contaminated human milk, and/or cross-contamination via laboratory accidents.
The disease has three distinct phases: acute, indeterminate, and chronic. In the acute phase (four to eight weeks) patients are usually asymptomatic or oligosymptomatic, showing mild symptoms such as fever, weakness, lymph node enlargement, hepato- and/or splenomegaly, and pruritus at the bite site. The indeterminate phase can last for many years, with no clinical manifestation of the disease (latent period). In the chronic phase, 20–40% of the patients (in the indeterminate phase) may show signs of cardiomyopathy and digestive disease (megaesophagus and/or megacolon), resulting in swallowing impairment and severe constipation.
In immunocompetent patients, meningoencephalitis is the most common manifestation of CD (in the chronic phase), especially in children. Central nervous system mass lesions are not typical in immunocompetent hosts. In immunosuppressed patients, CD may manifest as meningoencephalitis or a brain mass. The most common imaging finding in patients with CNS CD is ring-enhancing lesions, which can be solitary, multiple and small, or mass-like. Neurologic symptoms are variable; depend on the number, size, and location of the lesions; and may include headache, fever, cognitive changes, seizures, tremor, or hemiparesis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree