46 Carpal Tunnel Syndrome
Carpal tunnel syndrome is a neuropathy of the median nerve caused by compression of the nerve within the carpal canal. The most common cause found intraoperatively is degenerative or inflammatory thickening of the flexor tendon sheaths. Radiography should always be performed to exclude osseous stenosis of the carpal tunnel due to malalignment of the carpal bones. Sectional-imaging studies are required only when the situation remains equivocal: US to visualize the median nerve; CT when there is suspicion of an osseous carpal stenosis or an acute calcium deposit, and MRI to determine the nature and extent of space-occupying soft-tissue lesions within the carpal canal. These three procedures can demonstrate changes in the shape resp. signal intensity of the median nerve caused by compression. When postsurgical complaints persist, MRI is the evaluation method of choice.
Preliminary Remarks on Anatomy
The carpal tunnel is a 2.5cm-long osteofibrous canal on the palmar side of the carpus that contains the tendons of the finger flexors and the FCR and the median nerve ( Fig. 46.1 , Table 46.1 ). In the proximal section, the floor is formed by the capitate, hamate, and triquetrum. The radial wall is formed by the scaphoid, and the ulnar wall by the pisiform. The palmar side is bordered by the flexor retinaculum (transverse carpal ligament), which attaches to the tubercle of the scaphoid and the pisiform. The carpal tunnel is narrower in its distal section and is located deeper in the carpus. The distal floor section is formed by the capitate and trapezoid, the radial wall by the trapezium, and the ulnar wall by the hook of the hamate. The flexor retinaculum is thickest in the distal portion and inserts on the tubercle of the trapezium and the hook of the hamate.
The tendons of the flexor digitorum superficialis and flexor digitorum profundus muscles run within a common tendon sheath in two rows, one over the other. The tendon of the flexor pollicis longus muscle has its own sheath, which communicates with the synovial sac of the other flexors in 50 % of cases. This sheath lies radial of the aforementioned tendon sheath. The tendon of the flexor carpi radialis muscle lies outside the actual carpal tunnel along the trapezium and between the layers of the flexor retinaculum. The median nerve is located immediately below the flexor retinaculum and, very variably, usually radial of the middle line. Before entering the carpal tunnel the median nerve gives off its sensory palmar branch, and within the tunnel motor branches for the abductor pollicis brevis, the opponens pollicis, the superficial head of the flexor pollicis brevis, and the two ulnar-sided lumbrical muscles.

Boundary | Carpal Tunnel Entrance | Carpal Tunnel Exit |
Floor | Capitate | Capitate |
Roof | Flexor retinaculum | Flexor retinaculum |
Radial side | Scaphoid | Trapezium |
Ulnar side | Pisiform | Hook of the hamate |
Pathophysiology and Clinical Symptoms
A compression neuropathy of the median nerve can be caused either by narrowing of the cross-section of the tunnel or by an increase in volume of its contents. Tenosynovitis or chronic fibrosis of the flexor-tendon sheath is found in up to 85% of cases, usually as a result of repeated strain. Further causes are summarized in Table 46.2.
Clinically, there is burning pain, numbness and paresthesia of the first to third fingers and on the radial side of the fourth finger. Pain is triggered or increased at night by inactivity during sleep and can radiate into the forearm and the shoulder. Symptoms can also be provoked by percussing the palmar side of the carpus (Tinel’s sign) and forced flexion of the wrist (flexion test). In the chronic stage, there are atrophy of the thenar muscles. Atypical clinical symptoms are not uncommon, e.g., no loss of motor function due to extremely proximal separation of the motor branch for the thenar muscles or an atypical sensory distribution when there is proximal crossover between the median nerve and the ulnar nerve. Electroneurography (ENG) and electromyography (EMG) usually show decreased nerve-conduction velocity and lengthening of the motor and sensory nerve latency.
Diagnostic Imaging
Radiography
Radiography of the wrist and the carpal tunnel can provide evidence of an osseous carpal stenosis resulting from fractures, dislocations, or degenerative or inflammatory processes. Soft-tissue calcifications, as in acute hydroxyapatite deposition disease (Fig.46.3), can also be identified.
Ultrasonography
The median nerve can best be identified on axial scans. The tendons of the flexor pollicis longus muscle and the flexor digitorum superficialis tendon of the index finger can be localized by moving the fingers. The nerve usually lies immediately palmar of these structures (see Figs. 7.3 – 7.5 ). The tendon of the palmaris longus muscle, which is superficial to the flexor retinaculum just above the median nerve, can also serve as a guiding structure. The echogenicity of the nerve depends on the acoustic angle, but is always somewhat less than that of the tendons.
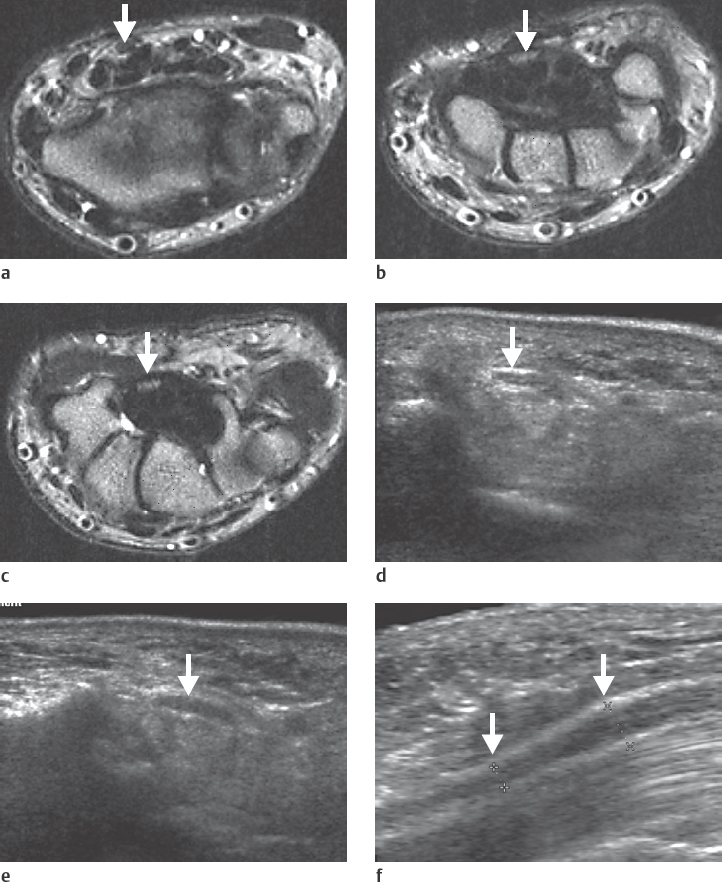
The three characteristic findings in the carpal tunnel syndrome, which can occur in isolation or in combination, are listed in Table 46.3 (Fig. 46.2 d-f).
The US findings can be quantified. The cross-sectional area A and the flattening ratio R of the nerve, as well as the palmar deviation PD of the flexor retinaculum serve as measuring parameters. The definitions of these parameters and their normal values can be found in Table 46.4 .

Besides these general changes, even the pathology causing the carpal tunnel syndrome can sometimes be identified with US.
Acute tenosynovitis is easily recognizable because of fluid accumulation around the generally thickened and indistinctly contoured tendons, whereas diagnosis of discrete thickening of the tendon sheaths is more difficult.
Ganglion cysts have smooth margins and are hypoechoic or anechoic.
Atypical muscles (Fig. 46.8b, c) can best be seen in longitudinal sections.
A persisting median artery (see Figs. 15.19 and 46.9 ) is associated with a proximal division of the median nerve in up to 10% of cases and can be identified in duplex US.
The advantages of US are its easy application and low costs. A disadvantage is the limited contrast resolution, which makes it difficult to identify the median nerve in the distal section of the tunnel and when it lies between the flexor tendons. Mild degrees of compression can be overlooked as a result of inherent errors in measurement.
Proximal swelling/pseudoneuroma of the median nerve:
|
Distal flattening of the median nerve:
|
Bulging of the flexor retinaculum:
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree